24 ذو القعدة 1434 هـ = 29/9/2013 MEDICINE Lec.
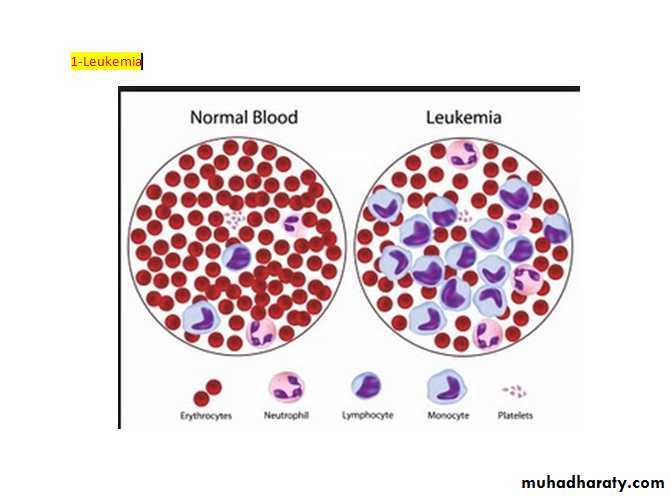
Leukaemias:
Leukaemias are a group of malignant disorders of the haematopoietic tissues characteristically associated with increased numbers of white cells in the bone marrow and/or peripheral blood.
The incidence of leukaemias approximately 10/100.000 per annum.
Males to females ratio being about 3:2 in acute leukaemias 2:1 in chronic lymphocytic laukaemia (CLL) and 1.3:1 in chronic myeloid leukaemia (CML).
Geographic variation in incidence does occur. Acute lymphoblastic leukaemia (ALL) have a striking rise over the age of 50. Chronic leukaemias occur mainly in middle and old age.
Aetiology:
The cause of leukaemia is unknown in the majority of patients. Several factors are associated with the development of leukaemia:Ionizing radiation.
Cytotoxic drugs particularly alkylating agent which induce myeloid leukaemia.
Exposure to benzene in industry.
Retroviruses.
Genetics (increase incidence in down's syndrome).
Immunological ex. Hypogammaglobulinaemia.
Classification:
Leukaemias are classified according to the clinical behavior of the disease into four main groups acute lymphoblastic, acute myeloid, chronic lymphocytic, and chronic myeloid.A more detailed classification developed for example the subclassification of lymphoblastic type is of value in the treatment as the common type responds well to treatment and carries the best chance of long-term remission.
Other classification might indicate the variable degree of maturation ex. In AML.
Subclassification of leukaemia:
*Acute lymphoblastic:
Common type (pre-B).
T cell.
B. cell.
Undifferentiated.
*Acute myeloid: FAB classification
M0 undifferentiated
M1 minimal differentiation.
M2 differentiated.
M3 promyelocytic.
M4 Myelomonocytic.
M5 Monocytic.
M6 eryturocytic.
M7 Megakaryocytic.
*Chronic lymphocytic:
B- cell – common.
T- cell – rare.
Chronic myeloid:
Ph2 positive.
Ph2 negative, BCR- abI3 positive.
P2 negative, BNCR- abI3 – negative.
Eosinophilic leukaemia.
FAB= French – American – British.
Ph= Philadelphia chromosome.
BCR= break point cluster region, abl = Abelson oncogene.
Acute leukaemias (AL):
There is a failure of cell maturation in AL. this immature cells accumulate in the bone marrow at the expense of the normal haematopoietic elements. Eventually this proliferation spills into the blood.Clinical features:
The clinical features are usually those of bone marrow failure (anaemia, bleeding and infection). 50% presented with fatigue as the first symptoms, anorexia and weight loss are also common. Fever with or without infections is the initial symptoms in 10% of patients. 5% of patients show signs of abnormal haemostasis.Occasionally bone pain, lymphodenopathy, nonspecific cough, headache, or diaphoresis is the presenting symptoms, rarely patients may present with symptoms from a mass lesion which represent a tumour of leukaemic cells and is called a (granulocytic Sarcoma or Chloroma).
Physical signs such as fever, splenomegaly, hepatomegaly, lymphadenopathy, sternal tenderness, and evidence of infection and haemorrhage are often found at diagnosis.
M3 AML may present with significant haemorrhage.
M5 AML may present with bleeding associated with coagulopathies.
Investigations:
Blood examination usually shows anemia with a normal or raised MCV (normochromic normocytic), reduced reticulocyte count due to decreased erythropoiesis.
The leukocyte count may vary from as low as 1x109/L to as high as 500x109/L or more. In the majority of patients the leukocyte count is below 100x109/L.
Thrombocytopenia is usually severe.
Blast ells and other primitive cells in the peripheral blood is diagnostic. Sometimes the blast cells count could be very low in the peripheral blood and bone marrow examination is necessary for diagnosis.
The bone marrow is the most valuable diagnostic investigation and provide material for cytology, cytogenetics and immunological phenotying. A trephine biopsy should be taken if no marrow is obtained (dry tap). The leukaemic blast cells represent more than 20% of the marrow cells.
The presence of Auer rods in the cytoplasm of blast cells indicate myeloblastic type of leukaemia.
Other investigation required such as: Haemostatic function, renal function, hepatic function, and cellular proliferation (LDH and uric acid).
Management:
The first decision must be whether or not to give specific treatment. It may not be appropriate for the elderly or patients with other serious disorders.
A.Specific therapy:
Adequate survives should be available for the specific therapy to be given:
Treatment of infection.
Correction of anaemia with red cell concentrate.
Control of bleeding by platelets transfusion.
If possible central venous catheter insertion to facilitate the circulation.
The aim of treatment is to destroy the leukaemic clone of cells without destroying the residual normal stem cell. Specific therapy include three phases:
Remission induction: the bulk of the tumour is destroyed by combination chemotherapy. The patients goes through a period of severe bone marrow hypoplasia requiring intensive support.
Remission consolidation: residual disease is destroyed during this phase resulting in a periods of marrow hypoplasia.
Remission maintenance: repeating cycle of drug administration used in acute lymphoblastic leukaemia.
This specific therapy may extend for up to 2 years if relapse does not occur thereafter specific therapy is discontinued and the patient observed.
In patients with ALL it is necessary to give therapy to the CNS (consist of a combination of cranial irradiation and intrathecal methotrexate.
If a patient fails to go into remission with induction treatment, alternative drug combination may be tried.
The early relapses the worse the prognosis.
Phase Lymphoblastic Myeloid
Induction Vincristine (I.V) Daunorubicin (I.V)
Prednisolon oral cytorabin (I.V)
L. asparaginase (I.V) Etoposide (I.V)
Daunorubicin (I.V) Tioguanine (oral)
Metnotrexate (intrathecal)
Consolidation Daunorubicin (I.V) cytarabine I.V
Cytarabine (I.V) Amsacrine IV
Etoposide (I.V) Mitoxantrone
Metnotrexate (I.V) Mitozantrone (I.V)
Maintenance prednisolon (oral)
Vincristine (I.V)
Mercaptopurine (oral)
Methotrexate (oral)
Pro myelocytic leukaemia (M3) can be treated by tretenoin (ATBA) together with combination chemotherapy for remission induction and then receive consolidation chemotherapy (Daunorubincin and cytarabine) followed by maintenance tretenoin or chemotherapy.
Complete remission (CR) is defined after examination of both blood and bone marrow and should last ≥ 4 weeks.
The blood neutrophil count must be ≥ 1500/microliter and the platlets count ≥ 100.000/ML. circulating blast should be absent. Bone marrow cellularity should be > 20% with trilineage maturation.
The bone marrow should contain <5% blast, and Aure rods should be absent. Extramedullary leukaemia should not be present.
B.Supportive therapy:
Potentially causative therapy which involves periods of severe bone marrow failure would not be possible without adequate supportive care.
Anaemia treated with red cell concentrate (Hb > 10mg/dL).
Bleeding: thrombocytopenic bleeding requires platlets transfusion (prophylactic transfusion maintain the platlet count > 10 x 109/L. coagulation abnormalities may need treatment with FFP.
Infection: fever (> 38C°) lasting over 1 hour in aneutropenic patient (neutrophil count < 1 x 109/L) indicate possible septicaemia. Parantral braod spectrum antibiotics therapy is essential example aminoglycoside with braod spectrum pencilline. The most common organisms associated with severe neutropenia are gram positive bacteria such as staph. aureas and staph. epidermid is gram negative infection with E-coli, pseudomonas and klebsiella are more likely to cause rapid clinical deterioration. Pneumocytic karinii may affect patients with lymphoblastic leukaemia and may need prophylasis with co-trimaxazol. Oral monilial infection is common and prophylaxis with fluconazol is often consider.
Systemic fungal infection with candida or pulmonary aspergillosis may need intravenous amphotericin 0.5-1 mg/kg/day for at least 3 weeks.
Herpes simplex infection occurs frequently and may need prophylactic treatment with acyclovir (200 mg 5 times/ day). The value of isolation facilities is debatable.
Metabolic problems: continuous monitoring of renal, hepatic and haemostatic function is necessary together with fluid balance measurements.
Poor prognostic features in acute leukaemia:
Increasing age.Male.
High leukocyte count of diagnosis.
Cytogenetic abnormality.
CNS involvement at diagnosis.
Antecedent haematological disorder.
Allogeneic bone marrow transplantation:
Indications:Neoplastic disorders affecting totipotent or pluripotent stem cell (ex. Leukaemia).
Failure of haematopoiesis ex. (aplastic anaemia).
Inherited defect in blood cell production ex. (thalassaemia, immune deficiency diseases).
In born errors of metabolism.
Healthy marrow or stem cells collected from the peripheral blood of a normal donar may be injected intravenously into a recipient who has been suitably conditioned.
The conditioning therapy used most of frequently is high dose cyclophosphamide and total body irradiation.
The injected donar cells home o the marrow, engraft and produce enough erythrocytes, granulocyte and platlets for the patients need after about 3-4 weeks. It may take several years to regain normal immunological function. The use of peripheral blood stem cells is associated with more rapid engraftment and immunological reconstitution making the procedure safer. The donars immunological system can recognize malignant recipient cells and destroy them. This immunological (graft versus disease) effected is a powerful tool against many haematological tumours and can be boosted in post transplantation relapse by the infusion of T cell taken from the donar so called donar leukocyte infusion.
Haematological indication for allogeneic B.M. transplant:
AML in first remission –
CML in chronic phase –
lymphoblastic leukaemia (T & B) in first remission –
ALL (common type) in second remission –
a plastic anaemia –
acute myelofibrosis –
lymphoma –
myeloma and immune deficiency syndrome.