Oxygen therapy
Oxygen used in therapy should be prescribed with the same care as a drug1- High oxygen concentration therapy is reserved of low PaO2 in association of normal or low PaO2 (type I respiratory failure), as in pneumonia and pulmonary edema.
2- Low oxygen concentration therapy is reserved for a state of low PaO2 with raised PaCO2 (type II respiratory failure).
3- Continuous oxygen therapy is given in persistent hypoxemia due to chronic obstructive pulmonary disease.
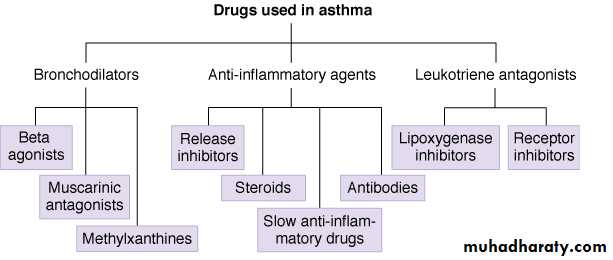
Drugs Used to Treat Asthma
Asthma
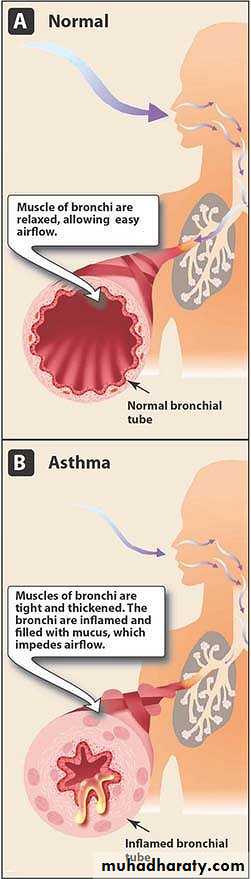
• Definition• Asthma is an inflammatory disease of the airways characterized by acute bronchoconstriction causing shortness of breath, cough, wheezing, and rapid respiration.
Asthma
PhathphysiologyAirflow obstruction in asthma is due to bronchoconstriction that results from:
• Contraction of bronchial smooth muscle
• Inflammation of the bronchial wall
• Increased mucous secretion
• Approaches to Treatment
• Prevention of exposure to allergen(s)• Reduction of the bronchial inflammation and hyperreactivity.
• Dilatation of narrowed bronchi
Reduction of the bronchial inflammation and hyperreactivity.
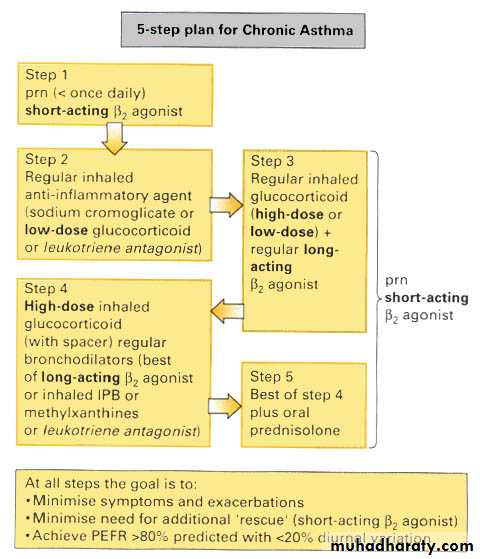
• Glucocorticoids• Mast Cell Stabilizers: Sodium cromoglicate
• Other drugs. Ketotifen
• Glucocorticoids
• Prednisolone (orally)• Beclomethasone, budesonide (by inhalation)
• Glucocorticoids
• MOA:• Inhibition of the influx of inflammatory cells into the lung after allergen exposure
• Inhibition of the release of mediators from macrophages and eosinophils, and T lymphocytes)
• Reversing mucosal edema
• Decreasing the permeability of capillaries
• Inhibiting the release of leukotrienes.
• After several months of regular use reduce the hyperresponsiveness of the airway smooth muscle to stimuli, such as allergens, irritants, cold air, and exercise.
• Increase the number of B2 recepters so promote bronchodilatation mediated by B2 receptors
• Oral/systemic: Patients with severe exacerbation of asthma (status asthmaticus) may require intravenous administration of methylprednisolone or oral prednisone.
• Inhaled Corticosteroids Side Effects:
• Pharyngeal irritation• Coughing
• Dry mouth
• Oral fungal infections
• Dysphonia
• Sodium Cromoglicate
• MOA:• Stabilize the cell membranes of inflammatory cells (mast cells, monocytes, macrophages
• Preventing release of harmful cellular contents (Indirect-acting agents that prevent bronchospasm)
• PK:
• Poorly absorbed from the gastrointestinal tract• Well absorbed from the lung
• Eliminated unchanged in the urine and bile.
Uses:
• Chronic asthma• Children asthma
• Pregnant wemon
• Exercise induced asthma
• Allergic rhinitis
• Other drugs: Ketotifen is a histamine H1-receptor blocker which may also have some antiasthma effects.
• Bronchodilators:
• Adrenergic agonists• Xanthine Derivatives
• Antimuscarinic bronchodilator
• Adrenergic agonists
• Nonselective adrenergicsExample: epinephrine
• Nonselective beta-adrenergics
• Example: isoproterenol
• Selective beta2 drugs
• Example: albuterol
• Beta-adrenoceptor Agonists
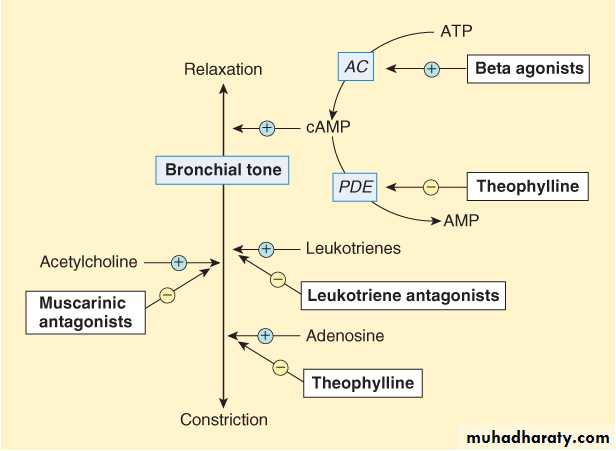
• MOA• Activation of beta2 receptors activate cAMP, which relaxes smooth muscles of the airway and results in bronchial dilation and increased airflow.
• B2- adrenoceptor activation also stabilises mast cells
Beta-adrenoceptor Agonists
• Albuterol, terbutaline, salbutamol• Rapid onset of action 15-30 minute
• Short-acting and provide relief for 4-6 hours
• Drug of choice for acute asthma
Beta-adrenoceptor Agonists
Salmeterol and Formoterol
• Slow onset of action
• Long-acting,12 h or more
• Used for prophylaxis
Side effect:
• Cardiac arrythmia• Oral and parenteral B2 agonist cause vasodilatation in the skeletal muscle vessels and this may lead to hypotension and tremor.
• Xanthine Derivatives:
Theophylline, a methylxanthine• Inhibition of phosphodiesterase (PDE),since this enzyme hydrolyzes cyclic nucleotides and this lead to increase cAMP
• Cause bronchodilation by relaxing smooth muscles of the airways.
• Relief of bronchospasm and greater airflow into and out of the lungs.
• Causes CNS stimulation.
• Causes cardiovascular stimulation: increased force of contraction and increased HR, resulting in increased cardiac output
• Increased blood flow to the kidneys (diuretic effect).
Pk:
• Rapid and complete Absorption from GIT.
• 90% is metabolised by the liver.
• The t l/2 is 8 h.
• Tobacco smoking enhances theophylline clearance by inducing hepatic P450 enzymes.
• Low therapeutic index.
Use of theophylline in status asthmaticus.
Side Effect of Theophyllin
• Nausea and diarrhoea, Vomiting, Gastroesophageal reflux during sleep• The chief dangers are cardiac arrhythmia, hypotension, hypokalaemia and seizures.
Drug Interaction of Theophyllin
• Enzyme inhibition by erythromycin, oral contraceptives increases the plasma concentration of theophylline.
• Enzyme inducers such phenytoin and rifampicin reduce the concentration.
• Antimuscarinic Bronchodilators
• Blockade of muscarinic (M3) receptors and causes bronchodilation, the preferred antimuscarinics• Ipratropium
• Oxitropium.
These synthetic compounds, prevents absorption after inhalation and minimizes antimuscarinic effects outside of the lung.
Uses: acute severe asthma when combined with B2-adrenoceptor agonists.
Leukotriene Receptor Antagonists
• Montelukast• Zafirlukast
MOA:
Montelukast, Zafirlukast are competitively prevent the bronchoconstrictor effects of leukotrienes
• By blocking their receptor
• Prevent leukotrienes from attaching to receptors on cells in the lungs and in circulation.
• Blocking the Inflammation in the lungs
Montelukast (once per day)
Zafirlukast (twice per day)
Leukotriene receptor antagonists Uses:
• Prophylaxis and chronic treatment of asthma
Omallizumab
It is a recombinant DNA-derived monoclonal antibody that selectively binds to human immunoglobulin E (IgE). This leads to decreased binding of IgE to the high-affinity IgE receptor on the surface of mast cells and basophophils. Reduction in surface-bound IgE limits the degree of release of mediators of the allergic responseIt is useful in moderate and sever allergic asthma in patients who are poorly controlled by conventional therapy
Its use is limited due to high cost.
Drugs used for allergic rhinitis
• Antihistamines (H1-receptor blockers)They are used in the treatment of sneezing and watery rhinorrhea, they are also used for pruritis
• Sedative first-generation drugs
Diphenhydramine
Chlorphenaramine
Adverse effects
Sedation, antimuscarinic effects, fatigue, dizziness
Drugs used for allergic rhinitis (continue)
• Non-sedative second-generation drugs
They are relatively selective for H1 receptor enter the brain less readily than do sedating antihistamines
Drugs used for allergic rhinitis (continue)
• α- adrenoceptor agonistNasal decongestants are used to constrict dilated arterioles in the nasal mucosa and reduce airway resistance such as phenylephrine
Oxymetazoline- long acting
Pseudoephedrine- oral
These drugs can be used in combination with antihistamine and for short peroid since they produce rebound congestion
Drugs used for allergic rhinitis (continue)
• CorticosteroidsTopical steroids may be more effective than systemic antihiastamine in relieving the nasal symptoms of allergic and non allergic rhinitis
Beclomethazone
Flunisolide
Systemic absorption is minimal
Drugs used for allergic rhinitis (continue)
• cromolynIntranasal cromolyn is used before contact with an allergen