General Principles ofGastrointestinal FunctionLec. 1dr-Rajaa Ahmad
The alimentary tract provides the body with a continualsupply of water, electrolytes, and nutrients. To achieve this requires (1) movement of food throughthe alimentary tract; (2) secretion of digestive juicesand digestion of the food; (3) absorption of water,various electrolytes, and digestive products; (4)circulation of blood through the gastrointestinalorgans to carry away the absorbed substances; and(5) control of all these functions by local, nervous, and hormonal systems.Proteins, fats, and complex carbohydrates are broken down into absorbable units(digested) in the small intestinethe products of digestion and the vitamins, minerals, and water cross the mucosa and enter the lymph or the blood(absorption)
These functions of the digestive system include:
1. Motility. This refers to the movement of food through the digestive tract through the processes of :a. Ingestion: Taking food into the mouth.
b. Mastication: Chewing the food and mixing it with saliva.
c. Deglutition: Swallowing food.
d. Peristalsis: Rhythmic, wave like contractions that
move food through the gastrointestinal tract.
2. Secretion. This includes both exocrine and endocrine secretions.
a. Exocrine secretions: Water, hydrochloric acid, bicarbonate, and many digestive enzymes are secreted into the lumen of the gastrointestinal tract. The stomach alone, for example, secretes 2 to 3 liters of gastric juice a day.b. Endocrine secretions: The stomach and small intestine secrete a number of hormones that help to regulate the digestive system.
3. Digestion. This refers to the breakdown of food molecules into their smaller subunits, which can be absorbed.
4. Absorption. This refers to the passage of digested end products into the blood or lymph.
5. Storage and elimination. This refers to the temporary storage and subsequent elimination of indigestible food molecules.
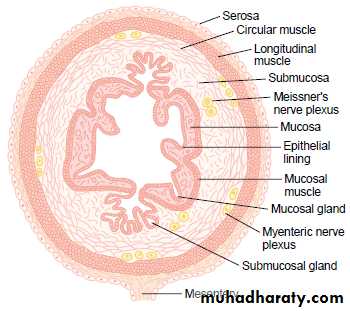
the intestinal wall, including the following layers from outer surface inward: (1) the serosa, (2) a longitudinal muscle layer, (3) a circular muscle layer, (4) the submucosa, and (5) the mucosa. In addition, sparse bundles of smooth muscle fibers, the mucosal muscle, lie in the deeper layers of the mucosa. The motor functions of the gut are performed by the different layers of smooth muscle.
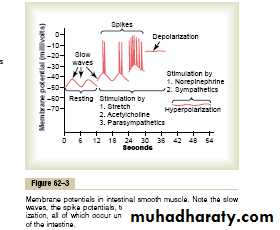
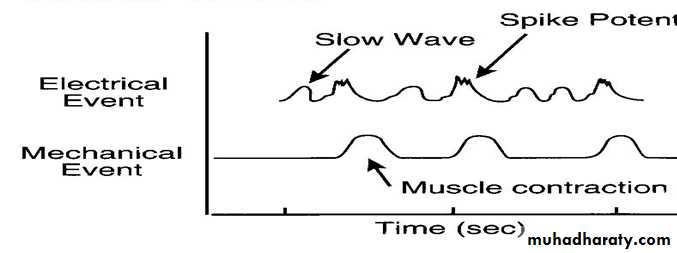
The smooth muscle of the GIT is excited by continual slow, intrinsic electrical activity along the membranes of muscle fibers. This activity has three types of electrical waves.
1.Slow waves potential or basic electrical rhythm(BER).
2.Spike or action potentials.
3.Changes in The voltage of resting membranepotential.
Are not action potential.
These BER caused by specialized cells called “interstitial cells of Cajal that are act as electrical pacemakers for smooth muscle cells.These pace-maker cells they are mainly excite the appearance of intermittent spike potentials, and the spike potentials in turn actually excite the muscle contraction. The slow waves usually do not by themselves cause muscle contraction in most parts of the gastrointestinal tract, except perhaps in the stomach. Instead, they mainly excite the appearance of intermittent spike potentials, and the spike potentials in turn actually excite the muscle contraction.
Slow waves potential or basic electrical rhythm (BER) or pace-maker waves.
Are true action potential. The normal resting membrane potential (RMP) in smooth muscle fibers of GIT between is -50 to -60mv. the channels responsible for the action potentials are calcium -sodium channels , they allow large numbers of calcium ions to enter along with smaller numbers of sodium ions .These channels are much slower to open and close .
The slowness of opening and closing of these channels accounts for the long duration of the action potentials.
The movement of large amounts of calcium ions to the interior of the muscle fiber during the A.P plays a special role in causing the intestinal muscle fibers to contract.
Spike Potentials (SP)
Under normal conditions the RMP averages -56mv, but multiple factors can change this level:A- Depolarization :depolarization is due to calcium ion influx. Factors that depolarize the membrane:
1- Stretching of the muscle.
2- Stimulation by acetylcholine (ACH).
3- Stimulation by Parasympathetic that secret ACH at these never endings.
4- Cold (colic pain).
5- Stimulation by several specific gastrointestinal hormones.
changes in voltage of the resting membrane potential (RMP)
B- Hyper polarization of the membrane: when the potential becomes more negative, the fiber becomes less excitable. Factors that hyperpolarization membrane.
1- Norepinephrine (NE) or epinephrine.
2- Heat 3- Pain
4. Stimulation of sympathetic nerves that secrete mainly NE at their never endings.
1. Enteric (intrinsic) nervous system.
2. Autonomic (extrinsic) nervous system.NEURAL CONTROL
Enteric nervous system is important in controlling GIT motility and secretion.The GIT has a nervous system all its own called the enteric nervous system. It lies entirely in the wall of the gut beginning in the esophagus and extending all the way to the anus .there are two major networks of nerve fibers that are intrinsic to GIT:
ENTERIC NERVOUS SYSTEM (ENS)
a- myenteric plexus (Auerbach’s plexus)
An outer plexus between the longitudinal and circular muscle lagers. The myenteric plexus controls mainly the GIT movements (Motility) or peristalsis.
b- an inner plexus called submucosal or Meissner’s plexus lies in the sub mucosa . This plexus controls GI secretion, and local blood flow, and local absorption.
Because the myenteric plexus extends all the way along the intestinal wall and because it lies between the longitudinal and circular layers of intestinal smooth muscle, it is concerned mainly with controlling muscle activity along the length of the gut. When this
plexus is stimulated, its principal effects are
(1)increased tonic contraction, or “tone,” of the gut wall,
(2) increased intensity of the rhythmical contractions,
(3) slightly increased rate of the rhythm of contraction,
and (4) increased velocity of conduction of excitatory
waves along the gut wall, causing more rapid movement
of the gut peristaltic waves.
1- Acetylcholine (ACH) which excites GI activity.
2-Noreopinephria almost inhibits GI activity.3- ATP
4-serotonin.
5- Dopamine .
6- Cholecystokinin (CCK)
7- somatostain.
8- gases: nitric oxide (No) and carbon monoxide (CO).
10- Vasoactive intestinal peptide (VIP).
Neurotransmitters secreted by ENS
sensory nerve endings that originate in the gastrointestinal epithelium or gut wall and send afferent fibers to both
plexuses of the enteric system, as well as
(1) to the prevertebral ganglia of the sympathetic nervous system,
(2) to the spinal cord, and (3) in the vagus nerves all
the way to the brain stem. These sensory nerves can
elicit local reflexes within the gut wall itself and still
other reflexes that are relayed to the gut from either
the prevertebral ganglia or the basal regions of the brain.