Impaction (2)
Complications of impacted lower third molar:
• Pain• edema
• and trismus.
• These are considered as acute reversible inflammatory response to surgical trauma. They can be minimized by gentle surgical technique, the use of NSAIDs or steroids, these complications peak after 48 hours and resolve within a week.
• Postoperative hemorrhage.
• Infection
• and abscess formation.
• Alveolar osteitis (dry socket), it occurs 3-4 days postoperatively due to blood clot disintegration, the predisposing factors include:
• Smoking history.
• Women taking oral contraceptives.
• Preexisting infection.
• Excessive surgical trauma. Localized osteomyelitis.
• Temporal or permanent nerve dysfunction of the inferior dental nerve and lingual nerve, this is manifested as anesthesia, paraesthesia or dysesthesia. Recovery of normal sensation may take few days to several months.
• Fracture mandible, uncommon, due to applying excessive force during extraction.
• Loss of the tooth or the root into the lingual space, if the displaced tooth can be palpated it can be directed back to the socket using finger pressure or it can be retrieved using a long tissue forceps, no blind attempt should be made, if retrieval fails another operation is needed.
•
Other lines of treatment
➢ Observation; when impacted teeth do not meet the indications of removal, periodic observation is needed.➢ Coronectomy; also called partial tooth removal, partial odontectomy or intentional root retention, is indicated to avoid damage to the inferior dental nerve in high risk cases. The tooth involved should not be mobile, not infected or involved with caries in its root, the crown and the coronal portion of the roots removed until they are 2-3 mm below the crestal bone, no treatment for the exposed pulp is needed and the retained portion of the roots should not be mobilized during the procedure.
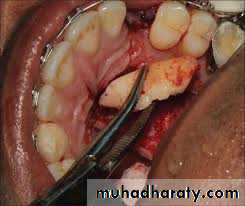
➢ Operculectomy; which is the excision of the soft tissue overlying the impacted tooth, it is indicated only in selected cases, subsequent excision may be needed.
➢ Orthodontic extraction; is another technique that decreases the risk of Inferior alveolar nerve injury. It is a combined orthodontic-assisted surgical approach that decreases the risk of neurologic complications and facilitates the surgical extraction of impacted mandibular third molars that are in close proximity to the mandibular canal
➢ Surgical transplantation; in selected cases, when the first molar is badly carious or unrestorable, the impacted tooth is carefully extracted and transplanted in the socket of the first molar after extraction and splinted.
Impacted upper third molars:
The main indications for removal include:• Non-functional teeth that are difficult to keep clean, especially those buccally inclined that may cause cheek bite or those over-errupted that cause trauma to the retro-molar tissue. • Those associated with a cyst or tumor. • Pericoronitis of the partially erupted teeth, although this is much less common than lower third molars.
• Resorption of the second molars (rare). • Preparation for the provision of prosthesis. OPG is the radiograph of choice. Periapical view, although it produces more detailed image, maybe unsatisfactory because of the angle of projection.
According to Archer (1975) the impacted upper third molar can be classified as vertical, horizontal, mesioangular, distoangular, buccoangular, linguoangular or inverted. He also classified the impacted upper third molars according to the depth compared to the adjacent second molar into: Class A: the occlusal surface of the impacted tooth is at the same level of the occlusal surface of the second molar. Class B: the occlusal surface of the impacted tooth is at the middle of the adjacent second molar. Class C: the occlusal surface of the impacted tooth is below the cervical line of the second molar or deeper.
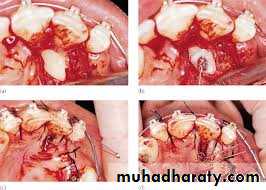
Surgical technique:
the incision is made across the tuberosity (blade No 12 is suitable) to the distobuccal aspect of the second molar and up to the buccal sulcus as a relieving incision, the incision can be extended to the mesiobuccal aspect of the second molar to improve access especially in case of deeply impacted third molars.After bone removal to expose the crown (if needed) a Warwick James' elevator or a straight elevator is used to elevate the tooth.
This is followed by copious irrigation and suturing.
Complications
➢ Hemorrhage, hematoma formation and periorbital edema. ➢ Oroantral fistula.➢ Displacement of the tooth or root into the maxillary antrum, this may be relieved by Cald-well-Luc approach.
➢ Displacement of the tooth into the infratemporal fossa lateral to the pterygoid plates, good tissue retraction is needed to relieve the tooth, X-ray maybe required to localize the tooth.
Fracture of tuberosity, if the fracture involves a small segment, it can be removed with the bone, followed by smoothing of the edges and careful suturing. If the segment is judged to be large it can lead to significant sinus opening which is difficult to close. The clinician should stop and splint the tooth using brackets or wire for 6 weeks to allow healing.
➢ Infection.
➢ Dry socket is uncommon in the maxilla.
Impacted maxillary canine
Impacted maxillary canineMaxillary canines are impacted in about 1%-3.5% of the population; the rate among female patients is twice as high as that in males. The proposed causes for maxillary canine impaction include:
• Maxillary canines start their development at a higher level than the adjacent teeth and erupt after them.
• The long distance that this tooth needs to travel into its normal position there is an increased chance of deflection.
• The space for its eruption may be taken up by the first premolar.
• Disturbance of the axis of the tooth germ, scar tissue in the path of eruption.
• Failure of resorption or ankylose of the root of the deciduous predecessors, or their early loss.
• Missing lateral incisor which acts as a guide for the canine.
• Genetic theory; This theory is based on the observation that palatally impacted maxillary canines are often associated with other dental abnormalities, such as tooth size, shape, number and structure, all of which have been found to be genetically linked. These anomalies are thought to arise in embryonic development from a shared hereditary trait.
If the maxillary canine fails to erupt by the age of 13 years, its position should be investigated, the orthodontist should be consulted to determine if the tooth can be brought to normal occlusion.
Classification of impacted maxillary canine
Classification helps much in the diagnosis and treatment planning. The following classification suggested by Archer (1975):Class I: Impacted canines in the palate
1: Horizontal
2: Vertical
3: Semi-vertical
Class II: Impacted canines located on the labial surface
1: Horizontal2: Vertical
3: Semi-vertical
Class III: Impacted canine located labially and palatally; crown on one side and the root on the other side
Class IV: Impacted canine located within the alveolar process, usually vertically between the incisor and first premolar
Class V: Impacted canine in edentulous maxilla
Clinical examination
The position of the tooth may be obvious by the presence of a bulge either palatally or buccally. The palatal impaction is more common than the buccal one (this finding was based on plain film studies, studies using CT scanning showed different distribution). Some authors believe that the buccal impaction is associated with arch length deficiency while the palatal impaction is not.Palpation of the maxilla through the labio-buccal sulcus may reveal the presence of the bulge buccally.
The lateral incisor may be proclined due to the presence of the canine labial to the root or may be retroclined if the canine is palatal
Radiographic examination and assessment
The radiographic views that can be used include;periapical, occlusal, OPG, lateral skull view cone beam CT (CBCT) can also be used. The
periapical radiograph provides a detailed view of the tooth, surrounding bone, root formation, the presence of root resorption of the adjacent lateral incisor or the presence of any pathology. Localization of the canine is important especially when it can not be determined clinically. Methods of localization include:
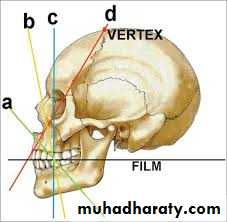
• Buccal object rule (parallax method, tube shift technique) in which two periapical films are taken, shifting the tube horizontally distally between exposures, if the un-erupted tooth moves in the same direction in which the tube is shifted it is localized palatally, if it moves in opposite direction it is buccally located, in a rule called SLOB (Same Lingual Opposite Buccal).
• In shifting the tube vertically inferiorly between exposures; the buccally located tooth will move inferiorly while the palatally impacted tooth will move superiorly.
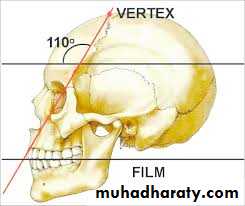
• Vertex occlusal projection; which produces an axial view of the incisors, will demonstrate the bucco-palatal localization of the canine.
• Periapical occlusal method; uses a standard periapical view and an occlusal view to give two different views of the impacted tooth.
• OPG; can be used to localize impacted canine on the basis that palatally impacted canine appear magnified. It can also demonstrate the vertical angulation and its height.
Options of treatment :
• Retention or leave in situ; indicated when:• The canine is asymptomatic and its extraction may lead to damage to the adjacent teeth.
• There is absence of infection, abnormal widening of the follicle, resorption of the adjacent roots or any other associated pathology.
• Aesthetically acceptable. The patient should be kept under annual review to verify that these complications have not arisen, the opinion of an orthodontist is important.
• Surgical exposure and orthodontic traction; is the procedure that allows natural or orthodontically guided eruption of the impacted teeth.
Certain criteria must be fulfilled:
• There should be adequate space in the arch to accommodate the tooth.• There should be an unobstructed path of eruption.
• After eruption the tooth should be in near to normal position in all planes.
• The timing of the procedure should be as close as possible to the normal eruption time.
Surgical approach for exposure:
The approach is through a palatal envelope flap, extending from the first molar to the first molar on the other side in bilateral impaction cases, or from the first molar to the first premolar on the other side in unilateral impaction casesBuccally impacted teeth are approached through a 3-sided buccal flap, depending on its location.
After reflection of a full mucoperiosteal flap, the crown is exposed using bur and a low speed handpiece or a sharp curette in cases of thin overlying bone. The exposure should be conservative taking care not to expose the cementoenamel junction (CEJ) as this was shown to result in increased incidence of external root resorption.
After exposure of the crown and hemostasis the orthodontist can attach a bracket to the crown at the same session.
In palatally positioned canine, a window is excised in the soft tissue before replacing the flap, if the bracket is not attached at the same operation the window is packed with a suitable pack until it epithelializes for 2-3 weeks. In buccal approaches it is more appropriate to suture the flap above the crown (apically repositioned flap) and the area below covered with a pack to ensure that the tooth will erupt into an area of keratinized mucosa.
Palatal envelope flap
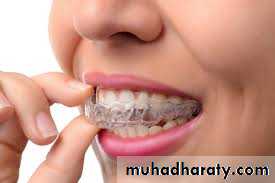
• Transplantation; in this procedure the canine is carefully extracted and transferred to a surgically prepared socket in the dental arch with minimum delay. The transplanted tooth should be splinted in its new position for about a month with an orthodontic appliance.It is essential to have sufficient space to accommodate the crown of the canine.
Success rate is increased when the un-erupted teeth still have open apex and when the handling of the root is kept to minimum to ensure the viability of the cementum and periodontal membrane.
Endodontic treatment should be performed as soon as possible after surgery (about 6-8 weeks), periodic follow up is required to allow early detection of root resorption which is common.
• Removal;
• surgical extraction maybe performed when the other options are unavailable. The main indications include:• Before construction of a dental prosthesis.
• To permit orthodontic alignment of other anterior teeth.
• When there is resorption of the roots of adjacent teeth.
• When a follicular cyst has developed.
• Infection although uncommon.
Extraction can be performed with retention of the primary canine with restorative procedures to improve esthetic contour,
extraction can also be accompanied with extraction of the primary canine and orthodontic closure of the space by the first premolar.
Implant supported crown can also be used to close the space created by extraction of the impacted canine and the primary canine.
Possible complications include:
• Palatal hematoma formation, this can be prevented by an acrylic splint to support the soft tissue.• Perforation into the floor of the nose, but it rarely causes a problem.