4 جمادي الاخرة 1435 هـ Ped.Lec. by Dr.Nadhim
4/4/2014
Thrombocytopenia in Infants and Children
Objectives:
1. Explain the relationship between platelet count and bleeding risk.
2. State the underlying pathologic mechanisms that may lead to clinically significant thrombocytopenia.
3. Describe the typical presentation and natural history of immune (idiopathic) thrombocytopenic purpura (ITP) in children.
4. List the features of the complete blood count and peripheral blood smear that suggest a serious disorder associated with decreased platelet production.
5. Discuss the treatment modalities that have been proven to be effective in raising the platelet count to a safe level in children who have ITP and are experiencing significant bleeding manifestations.
Platelets
Circulating platelets perform many critical hemostatic functions. When small blood vessels are transected, platelets accumulate at the site of injury, forming a hemostatic plug.Platelet adhesion is initiated by contact with extravascular components, such as collagen, and facilitated by the presence and binding of von Willebrand factor.
Secretion of mediators of hemostasis (eg, thromboxane, adenosine 5 diphosphate, serotonin, and histamine) cause firm aggregation via fibrinogen binding and increase local vasoconstriction.
Platelets also are necessary for normal clot retraction. Bleeding risk increases with a low platelet count.
Platelet counts:
Platelets, in general, have a brief 7 to 10 days life in the blood, after which they are removed from the blood circulation. The number of platelets in the blood is referred to as the platelet count and is normally between 150,000 to 450,000 per micro liter (one millionth of a liter) of blood. Platelet counts less than 150,000 are termed thrombocytopenia. Platelet counts greater that 450,000 are called thrombocytosis.Causes of thrombocytopenia:
The system used most often to categorize the different causes of thrombocytopenia is based on the underlying pathologic mechanism leading to the thrombocytopenia, that is, either increased destruction or decreased production of platelets or increased splenic sequestration (capturing of circulating platelets in the spleen).
Increased destruction of platelets
Disorders involving increased destruction or removal of platelets from the circulation typically result in the appearance of enlarged platelets on the peripheral blood smear (PBS), indicating that the bone marrow is producing new platelets to compensate for the increased destruction. The destructive mechanisms resulting in thrombocytopenia are:
● Immune-mediated destruction
● Platelet activation and consumption
● Mechanical platelet destruction
● Platelet sequestration and trapping
● Immune-mediated
–Immune thrombocytopenic purpura–Neonatal alloimmune thrombocytopenia
–Neonatal autoimmune thrombocytopenia
–Autoimmune diseases
–Drug-induced
● Platelet activation/consumption
–Disseminated intravascular coagulation
–Hemolytic-uremic syndrome
–Thrombotic thrombocytopenic purpura
–Kasabach-Merritt syndrome
–Necrotizing enterocolitis
–Thrombosis
● Mechanical platelet destruction
● Platelet sequestration
–Chronic liver disease
–Type 2B and platelet-type von Willebrand disease
–Malaria
Decreased production of platelets:
Impaired platelet production may be due to loss of
bone marrow space from infiltration, suppression
or failure of cellular elements, or a defect in
megakaryocyte development and differentiation. In
this setting, examination of the bone marrow generally
shows decreases in the number of megakaryocytes.
Causes of marrow dysfunction include:
● Infection
● Cyanotic heart disease
● Bone marrow failure or infiltration
● Nutritional deficiencies
● Genetic defects
● Infection
● Cyanotic congenital heart disease● Bone marrow failure or infiltrate
–Acute lymphoblastic leukemia and other malignancies
–Acquired aplastic anemia
–Fanconi pancytopenia
● Nutritional deficiencies
● Genetically impaired thrombopoiesis
–Thrombocytopenia with absent radii syndrome
–Congenital amegakaryocytic thrombocytopenia
–Wiskott-Aldrich syndrome
–X-linked thrombocytopenia with thalassemia
–Giant platelet disorders
–Bernard-Soulier syndrome
–May-Hegglin/Fechtner/Epstein and Sebastian syndromes
ITP
"idiopathic thrombocytopenic purpura"
The most common cause of acute onset of thrombocytopenia in an otherwise well child is (autoimmune) idiopathic thrombocytopenic purpura (ITP).
ETIOLOGY.
1–4 wk after exposure to a common viral infection, an autoantibody directed against the platelet surface develops. The exact antigenic target for most such antibodies in most cases of acute ITP remains undetermined.
After binding of the antibody to the platelet surface, circulating antibody-coated platelets are recognized by the Fc receptor on the splenic macrophages, ingested, and destroyed.
Most common infectious viruses have been described in association with ITP, including Epstein-Barr virus and HIV in the latter usually chronic.
CLINICAL MANIFESTATIONS.
1.No symptoms
2.Mild symptoms: bruising and petechiae, occasional minor epistaxis, very little interference with daily living
3.Moderate: more severe skin and mucosal lesions, more troublesome epistaxis and menorrhagia
4.Severe: bleeding episodes—menorrhagia, epistaxis, melena—requiring transfusion or hospitalization, symptoms interfering seriously with the quality of life
Sudden onset of generalized petechiae and purpura.
Often there is bleeding from the gums and mucous membranes, particularly with profound thrombocytopenia (platelet count <10 × 109/L).
history of a preceding viral infection 1–4 wk before the onset
Splenomegaly is rare, as is lymphadenopathy or pallor.
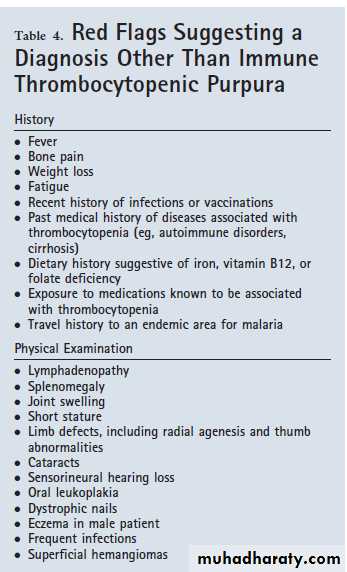
The presence of abnormal findings, such as hepatosplenomegaly or remarkable lymphadenopathy, suggests other diagnoses (leukemia).
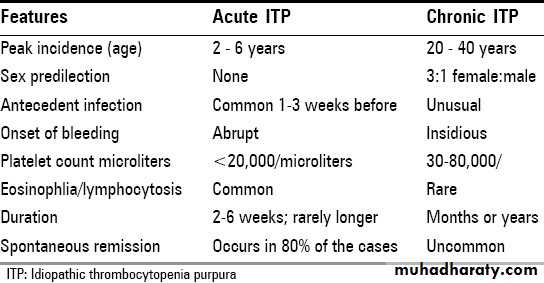
When the onset is insidious, especially in an adolescent, chronic ITP or the possibility that thrombocytopenia is a manifestation of a systemic illness, such as systemic lupus erythematosus (SLE), is more likely.
Fewer than 1% of patients have intracranial hemorrhage.
Approximately 20% of children who present with acute ITP go on to have chronic ITP.
LABORATORY FINDINGS.
Severe thrombocytopenia (platelet count <20 × 109/L) is commonplatelet size is normal or increased, reflective of increased platelet turnover
Hemoglobin value, white blood cell (WBC) count, and differential count should be normal.
Hemoglobin may be decreased if there have been profuse nosebleeds or menorrhagia.
Bone marrow examination shows normal granulocytic and erythrocytic series, with characteristically normal or increased numbers of megakaryocytes. Some of the megakaryocytes may appear to be immature and are reflective of increased platelet turnover.
In adolescents with new-onset ITP, an antinuclear antibody test should be done to evaluate for SLE.
A Coombs test should be done if there is unexplained anemia to rule out Evans syndrome (autoimmune hemolytic anemia and thrombocytopenia)
HIV studies.
Indications for bone marrow aspiration
abnormal WBC count or differential
unexplained anemia
findings suggestive of bone marrow disease on history and physical examination.
DIFFERENTIAL DIAGNOSIS.
Exposure to medication that induces drug-dependent antibodies
Splenic sequestration due to previously unappreciated portal hypertension
Rarely, early aplastic processes, such as Fanconi anemia
Amegakaryocytic thrombocytopenia and thrombocytopenia-absent radius (TAR) syndrome
HUS
DIC
HIV
Wiskott-Aldrich syndrome
Management of thrombocytopenia:
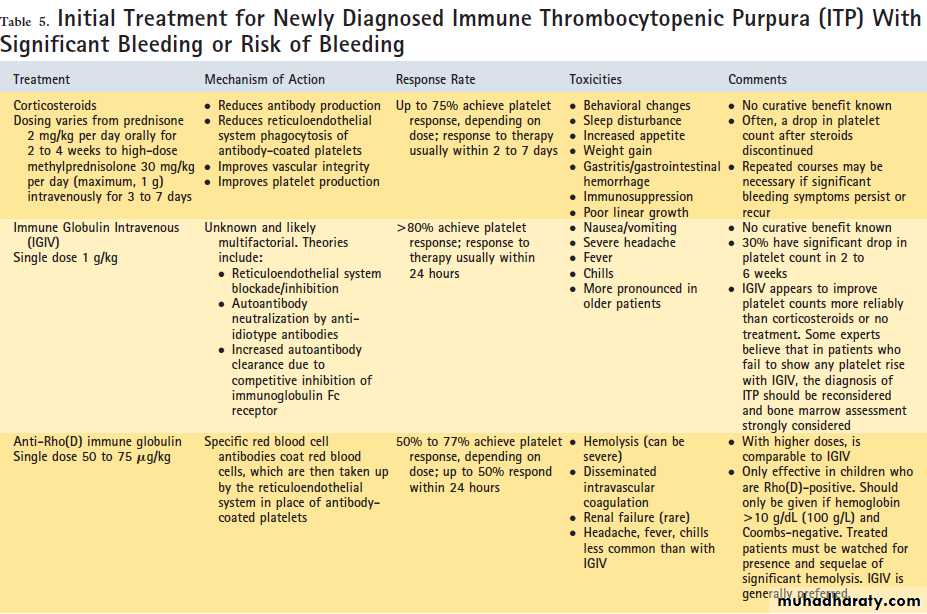
Management of thrombocytopenia in an individual patient should be guided by an understanding of its cause and predicted clinical course.Correction of the cause may not be possible (eg, congenital thrombocytopenias) or may not be necessary (eg, mild-to-moderate ITP).
The principal management goal in all patients who have thrombocytopenia is to maintain a safe platelet count to prevent significant bleeding, not to achieve a normal platelet count.
What constitutes a safe platelet count in a particular patient varies, depending on the cause of the thrombocytopenia and consideration of all other aspects of hemostasis.
For patients who have significant bleeding symptoms, treatment is essential. Asymptomatic or minimally symptomatic thrombocytopenia may be treated if the thrombocytopenia is severe or the perceived risk of bleeding is great
Activity Restrictions
When moderate-to-severe thrombocytopenia is recognized, implementing reasonable precautions to minimize bleeding risk is recommended.
These steps include trauma precautions (eg, avoidance of contact sports and use of a helmet while cycling) and avoidance of medications that have anti platelet or anticoagulant activity (including aspirin-containing preparations, ibuprofen, and other nonsteroidal anti-inflammatory drugs).
Invasive Procedures
A platelet count greater than 50 × 103 micro L (provides safety for most invasive procedures. If the risks of potentially serious bleeding are believed to be severe, a platelet count of greater than 100 × 103 micro L) is often required by surgeons or anesthesiologists.For common minor procedures, such as tooth extractions, a platelet count of 30 to 50 × 103 micro L often is sufficient.
For patients who have lower platelet counts, some measure to increase the platelet count immediately before the procedure may be required.
A short course of corticosteroids (prednisone 2 mg/kg per day for 1 week) or a single dose of immune globulin intravenous (IGIV) (1 g/kg) is often sufficient to increase the platelet count acutely for procedural hemostasis.
Platelet transfusions can be used in urgent situations. Although platelet survival in the circulation of patients who have destructive thrombocytopenias may not be normal, platelet transfusion nearly always provides prompt, satisfactory hemostasis, even if only for a short duration.
Emergency Management of Critical Bleeding
Patients who have severe thrombocytopenia and critical bleeding require immediate transfusion of platelets regardless of the cause of the thrombocytopenia.
ICH is the most serious consequence of severe thrombocytopenia.
Early diagnostic imaging should be considered for patients who have severe thrombocytopenia and neurologic signs or symptoms to identify ICH.
For patients who have unstable or progressive ICH, emergency craniotomy may be necessary.
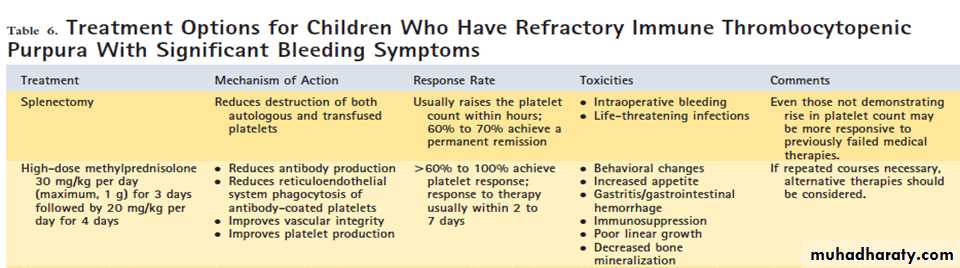
For patients who have ITP with life-threatening bleeding, in addition to platelets, adjunctive treatment with high doses of corticosteroid (intravenous methyl-prednisolone 30 mg/kg
لا تثق بشخص قلبه ابيض ......... يا اخي كل العالم قلوبها حمرة شمعنى هالشخص بالذات قلبه ابيض**من اطرف وامنطق (اسم تفضيل من المصدر منطق) ما قرأت**
^_^