Hemolytic Anemia د.بهاء
Definition:Those anemias which result from an increase in RBC destruction
Classification:
- Congenital / Hereditary
- Acquired
Causes:
INTRACORPUSCULAR HEMOLYSIS
Membrane Abnormalities
Metabolic Abnormalities
Hemoglobinopathies
EXTRACORPUSCULAR HEMOLYSIS
Nonimmune
Immune
Classification of Hemolytic Anemias:
Hereditary:1. Abnormalities of RBC interior
a.Enzyme defects: G-6-PD def,PK def
b.Hemoglobinopathies
2. RBC membrane abnormalities
a. Hereditary spherocytosis etc.
b. PNH
c. Spur cell anemia
Acquired:
Extrinsic factors
a. Hypersplenism
b. Antibody: immune hemolysis
c. Mechanical trauma: MAHA
d. Infections, toxins, etc
Membrane Defects:
1- Microskeletal defects
Hereditary spherocytosis
2- Membrane permeability defects
Hereditary stomatocytosis
3- Increased sensitivity to complement
Paroxysmal nocturnal hemoglobinuria
1.Hereditary Spherocytosis
Usually inherited as AD disorder
Defect: Deficiency of Beta Spectrin or Ankyrin Loss of membrane in Spleen & RES becomes more spherical Destruction in Spleen
C/F:
- Asymptomatic
- Fluctuating hemolysis
- Splenomegaly
- Pigmented gall stones- 50%
Complications:
Clinical course may be complicated with Crisis:
- Hemolytic Crisis: associated with infection
- Aplastic crisis: associated with Parvovirus infection
Invx:
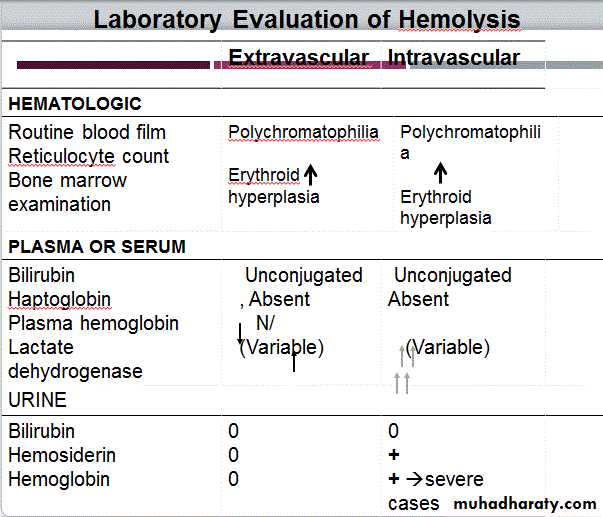
- Test will confirm Hemolysis
- B Smear: Spherocytes
- Osmotic Fragility: Increased
- Screen Family members
Management:
- Folic Acid 5mg weekly, prophylaxis life long
- Spleenectomy
- Blood transfusion in Ac, severe hemolytic crisis
X 2.Hereditary Elliptocytosis:
Equatorial Africa, SE Asia
AD / AR
Functional abnormality in one or more anchor proteins in RBC membrane- Alpha spectrin , Protein 4.1
Usually asymptomatic
Mx: Similar to H. spherocytosis
Variant:
3.SE-Asian ovalocytosis:
Common in Malaysia , Indonesia…
Asymptomatic-usually
Cells oval , rigid ,resist invasion by malarial parasites
Red Cell Enzymopathies:
Physiology:EM pathway: ATP production
HMP shunt pathway: NADPH & Glutathione production
1- Glucose-6-Phosphate Dehydrogenase ( G6PD ) Deficiency:
- Pivotal enzyme in HMP Shunt & produces NADPH to protect RBC against oxidative stress
- Most common enzymopathy -10% world’s population
- Protection against Malaria
- X-linked
Clinical Features:
- Acute drug induced hemolysis:
Aspirin, primaquine, quinine, chloroquine, dapsone….
- Chronic compensated hemolysis
- Infection/acute illness
- Neonatal jaundice
- Favism
Invx:
- E/O non-spherocytic intravascular hemolyis
- P. Smear: Bite cells, blister cells, irregular small cells, Heinz bodies, polychromasia
G-6-PD level
Treatment:
- Stop the precipitating drug or treat the infection
- Acute transfusions if required
X 2. Pyruvate Kinase Deficiency
- AR
- Deficient ATP production, Chronic hemolytic anemia
Inv;
- P. Smear: Prickle cells
- Decreased enzyme activity
Treatment:
- Transfusion may be required
Autoimmune Hemolytic Anemia:
- Result from RBC destruction due to RBC autoantibodies: Ig G, M, E, A
- Most commonly-idiopathic
- Classification:
1- Warm AI hemolysis: Ab binds at 37degree Celsius
2- Cold AI Hemolysis: Ab binds at 4 degree Celsius
1. Warm AI Hemolysis:
- Can occurs at all age groups
- F > M
Causes:
- 50% Idiopathic
- Rest - secondary causes:
1. Lymphoid neoplasm: CLL, Lymphoma, Myeloma
2. Solid Tumors: Lung, Colon, Kidney, Ovary, Thymoma
3. CTD: SLE, RA
4. Drugs: Alpha methyl DOPA, Penicillin , Quinine, Chloroquine
5. Misc: UC, HIV
Invx:
- E/O hemolysis, MCV
- P Smear: Microspherocytosis, n-RBC
- Confirmation: Coomb’s Test / Antiglobulin test
Treatment:
- Correct the underlying cause
- Prednisolone 1mg/kg po until Hb reaches 10mg/dl then taper slowly and stop
- Transfusion: for life threatening problems
- If no response to steroids *Splenectomy or
*Immunosuppressive: Azathioprine, Cyclophosphamide
2. Cold AI Hemolysis:
- Usually IgM
- Acute or Chronic form
Chronic:
C/F:
- Elderly patients
- Cold, painful & often blue fingers, toes, ears, or nose (Acrocyanosis)
Invx:
- E/O hemolysis
- P Smear: Microspherocytosis
- IgM with specificity
Other causes of Cold Agglutination:
- Infection: Mycoplasma pneumonia, Infec Mononucleosis- PCH : Rare cause seen in children in association with cong syphilis
Treatment:
- Treatment of the underlying cause
- Keep extremities warm
- Steroids treatment
- Blood transfusion
Non-Immune Acquired Hemolytic Anemia:
1- Mechanical Trauma
A). Mechanical heart valves, Arterial grafts: cause shear stress damage
B).March hemoglobinuria: Red cell damage in capillaries of feet
C). Thermal injury: burns
D). Microangiopathic hemolytic anemia (MAHA):
By passage of RBC through fibrin strands deposited in small vessels disruption of RBC eg: DIC,PIH, Malignant HTN,TTP,HUS
2- Infection
- F. malaria: intravascular hemolysis: severe called ‘Blackwater fever’
- Cl. perfringens septicemia
3.Chemical/Drugs:
- Oxidant denaturation of hemoglobin
- E.g: Dapsone, sulphasalazine, Arsenic gas, Cu, Nitrates & Nitrobenzene
Ideal Group
A.H.Yahia