Geriatric and Prosthetic Dentistry
Definitions
Geriatrics: The branch of medicine that deals with the diagnosis and treatment of diseases and problems specific to the aged.Gerodontics: the treatment of dental problems of aging persons; also spelled geriodontics
Gerodontology : the study of the dentition and dental problems in aged or aging persons
Classification of geriatric patients
I-According to changes:(1) physiologic
(2) psychology(3) pathologic
II-According to functional status:
1-Functionally independent old adults
2-Frail old adults3-Functionally dependent old adults
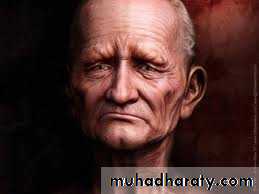
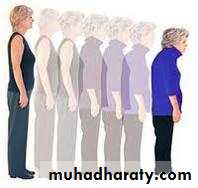
Classification of geriatric patientsPhysical manifestations
Hair shade-off, skin rankled, and the face has different changes in expressions.Hair, skin & face
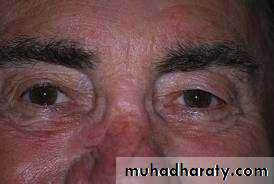
Hearing, smelling and vision sensesMay be Impaired …
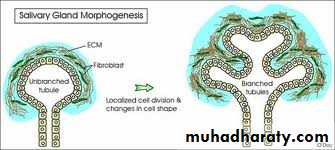
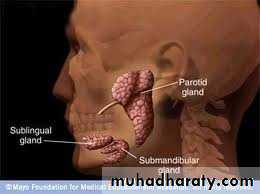
Secretory glands
RespirationGonads and genitourinary tract
All my be functionally interruptedAlso changes may occurs obviously to:
Mental condition
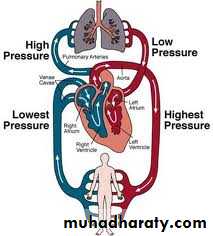
Blood and vascular system
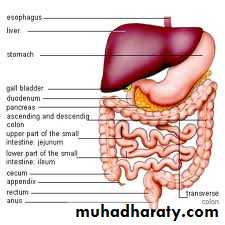
GITOral manifestations
Oral manifestations• Dental tissues
• A-enamel may be abraded
• B-dentin, calcified
• C-pulp has recession
D-hyper cementosis
2. Periodontal tissues
Decrease fibroblasts, more coarse fibers
•
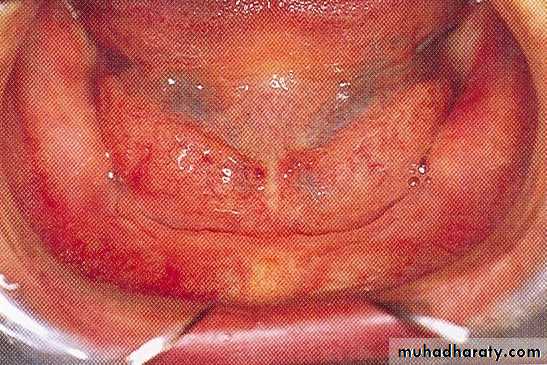
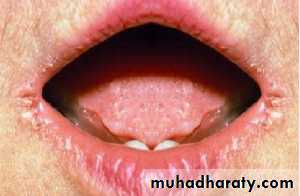
3. Oral mucosa
decrease in thickness, increase permeability and so decrease tissue tolerance to appliances. presence of hyperkeratosis flabby tissues in denture wearers.4. Gingiva
loss of stippling and
hypertrophy.
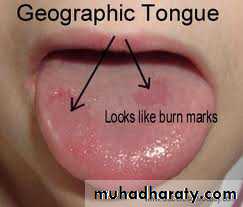
Tongue
Enlarged by loss of teeth and decrease in taste buds, it become lobulated, coarse or flat, and red.Geographic tongue may appear as an emotional episode.
Saliva
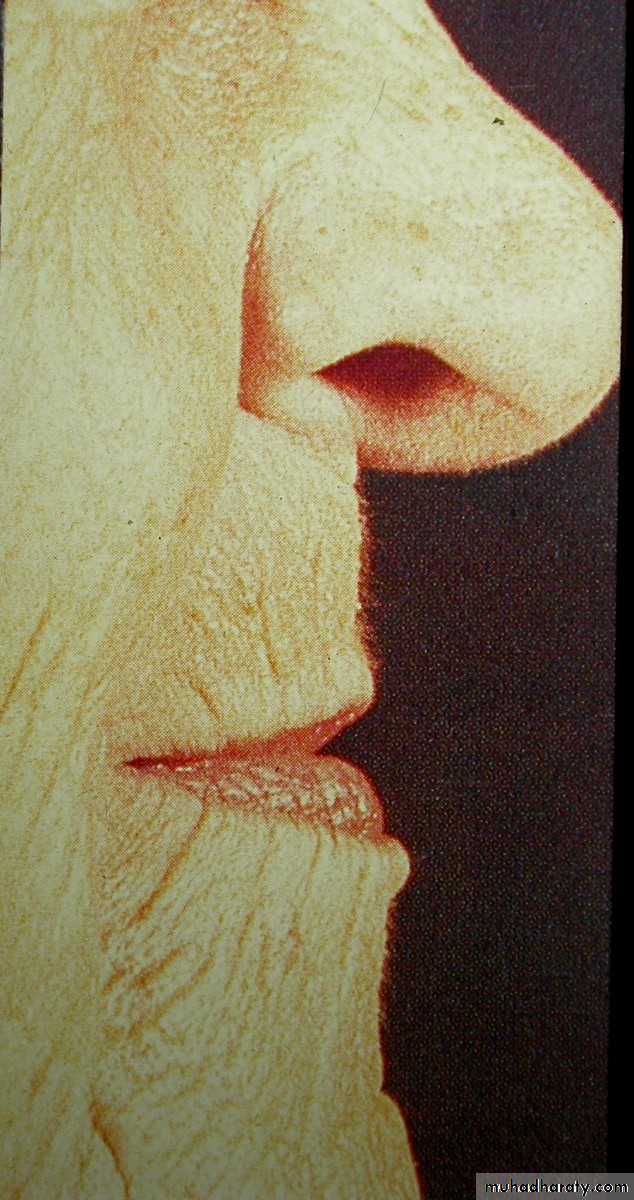
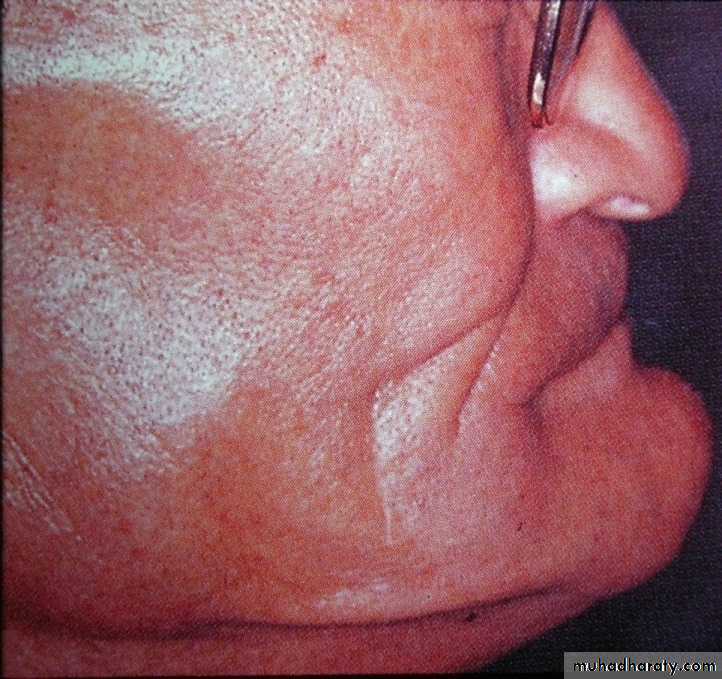
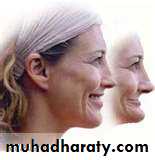
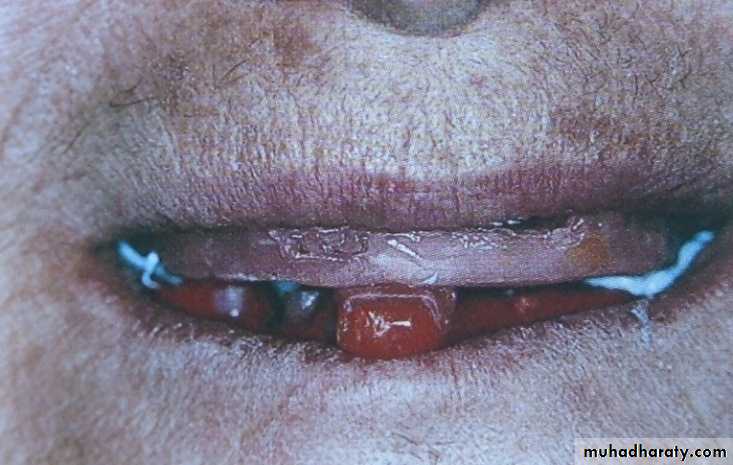
Viscous in consistency and decrease in amount.Lip and Facial Muscles
Angular cheilitis is very common. Falling in of lips due to the loss of adequate support and muscle tone. The facial musculature loses elasticity and resiliency with advancing.Tempromandibular joint
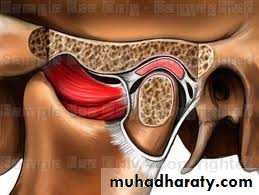
By aging flattening of the articular fossa and condyle, the disk become thinner and so the joint becomes smaller.Also joint dysfunction may occur as a result of change in occlusion or muscle hyperactivity caused by emotional stress.
Over closure for many years may damage the articular disc causing pain and limitation of range of movement of the jaws. Old patient may suffer from osteoarthritis or rheumatoid arthritis also T.M.J. can be affected
Tempromandibular joint
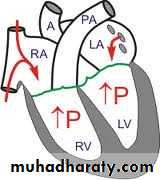
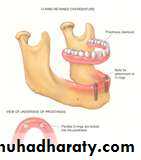
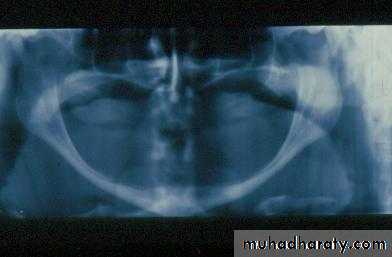
Residual bone and maxillomandibular relationship:Osteoporosis has a direct relation to the ridge resorption.
Pattern of bone loss in mandible differs from that of the maxilla and so the mandible become larger and the maxilla become smaller.
Progression of resorption
Pathophysiology of Edentulous bone lossFactors influencing edentulous bone loss
• 1) metabolic Factor: Vit. D deficiency,malnutrition…• 2) Osteoporosis : normal with aging
• 3) osteomalacia: un mineralized & impaired bone healing is present
• 4) drug therapy : drugs associated with decreased bone density
5) mechanical factors: such as:
ill-fitting dentures
Parafunctional activity
6) anatomic factor:
(a) long face (dolichocephalic)
tend to have longer ant. alveolar ridge in the vertical plane. than those with short face (brachycephalic)(b) short face (brachycephalic)
are capable of higher biting forces in both the molar and ant. regions..After loss of teeth, higher biting forces enhance edentulous bone loss.
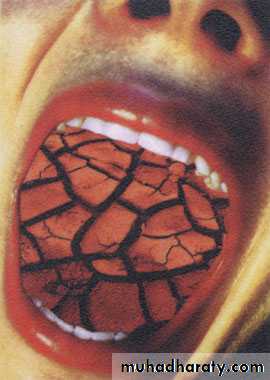
Xerostomia
Etiology
AgingFoods & drugs
Systemic factors
Radiotherapy (>4000rad)
Sjogren’s syndrome
Other salivary gland diseases
irreversible change
reversible change
Clinical picture
Dry mouth
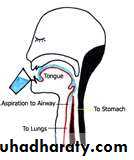
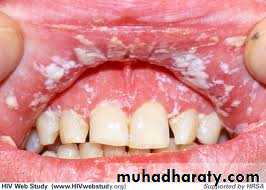
difficulty in normal oral and oropharyngeal functionsIncrease susceptibility to infection
Caries
Halitosis
Medications that cause xerostomiaAnti(anxiety,depressants,seizures,diarrheal,his-taminics,nausea,parkinsonian).
Diuretics, heart medications, muscles relaxants &NSAIDs
ManagementsOf
Xerostomia
Dietary & environmental considerations
• Avoid drugs that may produce xerostomia• Avoid dry & bulky foods
• High fluid intake & rinsing with water
• Avoid alcohol and smoking
• Take protein and vitamin supplements
Preventive Dental Care Measures
Smooth (sharp cusps, occlusal grooves or fissures, and irregular fillings).
Check and adjust the denture.
OHI.
Topical fluoride .
Fluoride rinses & chlorhexidine rinses.
Antifungal medications:
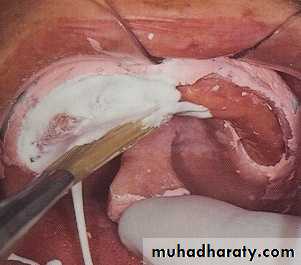
Denture: Miconazole gel,amphotericin or nystatin ointment
Topical: Nystatin, amphotercin suspension or fluconazole
Salivary Stimulants &Substitutes
Chewing gumsDiabetic sweets
Sialagogues (Pilocarpine)Prosthetic options for management of Xerostomia
• Split- reservoir complete dentures containing salivary substitutes.• 2. Complete dentures with metal palatal portion.
Psychological Manifestations
High incidence of depression and feelings of insecurity and may experience vague and pain and fear from unknown.Also nervous habits may develop, manifested by parafunctional habits exerting extra stress on the supporting structures.
Psychological Manifestations
Medical conditions that reflected on the dental management
ArthritisDental considerations
• Difficulty in denture care procedure.
• TMJ may show difficulty in performing different movements during steps of denture construction.
Avoid prolonged procedure to avoid patient fatigue.
Cardiac problems:Neurological disorders: Parkinson's disease
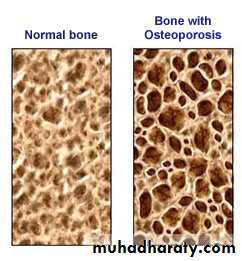
The movements and spasmodic head positioning associated with the disease may compromise the dentist’s ability to carry out restorative care. These patients’ involuntary movements can make the use of sharp and rotating instruments hazardous.Osteoporosis.
May be caused by hormones or drugs assteroids and anticonvulsants
Antiepileptic drugs
This is not a disease entity but may be a manifestation of a diverse group of diseases ,it is characterized by a reduction in the mass of bone / unit volume.
Osteoporosis can be caused by certain hormonal disturbances as:
HyperparathyroidismHypothyroidism
DM
Adrenal insufficiency
Menopause in females
Dental considerations for Osteoporosis
Fragility Fractures resulting from minimal trauma can result in significant morbidity and mortality in older adults who are functionally independent.
Diabetes Mellitus (DM)
HypoglycemiaDental Considerations for DM
Short appointments at morning.
Treatments sh. be with minimum trauma & stress .
Maintains good oral hygiene regarding using topical agents , such: chlorhexidine.
Using Prophylactics & fluoride gel found to be effective
Management of related xerostomia & other endocrines signs.
Dentist sh. Learn about diagnosis & treatment of Hypoglycemia shock.
Nutritional deficiency
a) 1ry: which is due to lack of nutrients in diet
b) 2ry: due to failure to absorb ,utilize or increase nutrients due to illness or excessive exertion.Vit.B12 angular chelitis
Vit.B2 pellagra
Vit.C
General weakness, retarded wound healing, petechial patches due fragility of capillary walls, gingival bleeding and marked bone resorption.The geriatric prosthetic patient
Geriatric patients (as well as all dental patients) should not be promised too much. Patients tend to remember every claim the dentist has made and will hold him to it.Esthetics is important in fabricating dentures for the aged. An esthetic denture may be the turning point in patient acceptance.
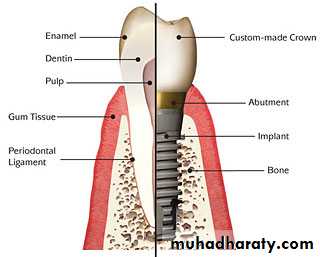
Replacement options
Conventional optionsTemporary RPD
Complete denturesPermanent RPD
RPD for Geriatrics
The design should be as simple as possibleSo as to decrease the trapping areas predisposing to increase the caries susceptibility
• Design should consider future addition of questionable teeth.• The design should consider deleting rests from compromised teeth to avoid overloading.
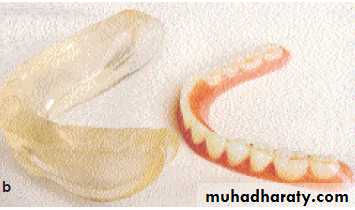
Complete dentures
considerations
benefitsContributes further bone loss
Tissue support sore spots
Nerve exposure painOn going expenses to maintain by relining, denture adhesives &cleansers.
Loose fitting diff. in eating and speaking.
Palatal coverage interferes with normal sensation of food.
Least costly approach
fast
Implant as a prosthetic optionOver denture supported with implants
Benefits:Next least costly approach
Better fixation of denture
Improve chewing ability
Benefits: Best fit mostly like natural teethNo dietary limitationsMaximize nutritional intakeNo interference with taste due to minimal coveragePreserve bone
Implant retained fixed bridge
• Considerations:• Cost
• Longer treatment time
• Multiple visits
Masticatory Performance
All Natural teeth 100%Implant retained bridge 90%
Implant with over denture 60%
Conventional complete denture 10%
No teeth or denture 0%
What is the best choice?
Several factors are considered to choose the best treatment modality:
Amount of bone available
Quality of bone
Patient systemic conditions
Amount of force applied
Patient financial conditions
Implants for irradiated patients
Problems of irradiated bone:Decrease number of osteoblasts and osteocytes
Fatty degeneration in marrow spacesBlood vessels undergo progressive degeneration, hyalinization and fibrosis, resulting in regional ischemia.
Recommendations for using irradiated bone for implant insertion
Minimal one year elapsing before implant insertion.Using hyperbaric oxygen
Complete denture construction
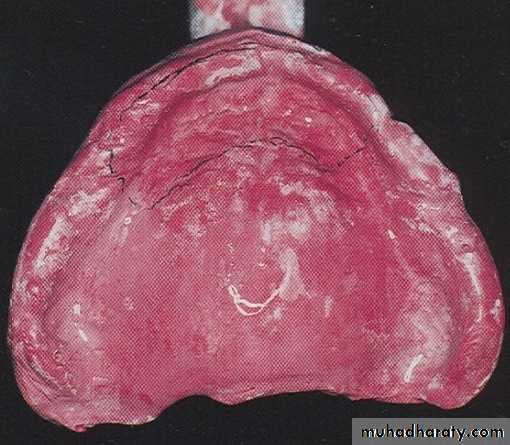
Prior to making edentulous impressions for geriatric patients, the denture-bearing tissues must be carefully examined.
If ill-fitting dentures have abused them, the use of tissue conditioner is a necessity until their return to normal physiologic color and tone.
The final steps of impressions are made according to the condition of residual alveolar ridge
Impressions:
Flat ridge
• Muco-compressive impression technique
• Called closed mouth technique, it requires;• A well fitting record base.
• An accurate occluding rims
• An acceptable vertical dimension
• Final impression made using zinc oxide impression paste or viscous elastomeric material while the patient closing on the occlusal rims
• Selective pressure impression techniques
Dynamic impression technique (Functional impressions)
• These techniques may be used where problems of stability exist :• Three materials are commonly used for functional impressions.
• Alginate materials
• Elastomeric materials
• Tissue conditioning materials
• Used to record the range of muscle action, spaces into which the dentures can extend without displacement.
Final impression making
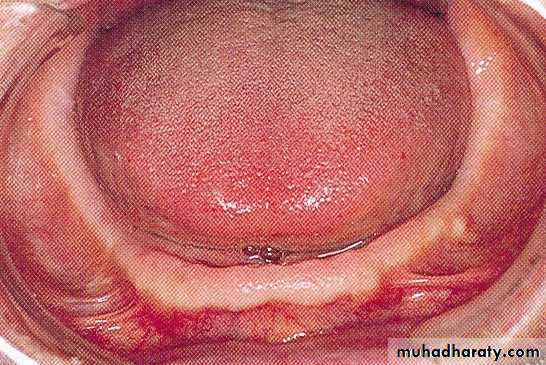
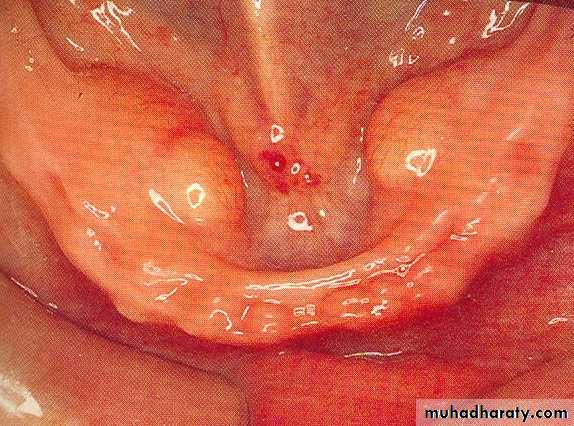
Butterfly impression technique
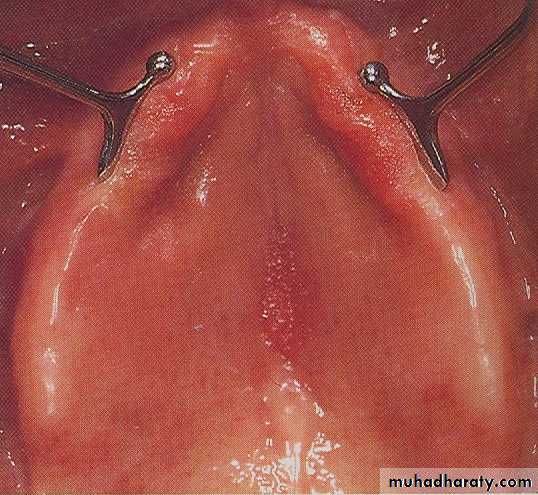
Indicated with advanced ridge resorption with projecting sublingual gland and with presence large mandibular toriProjecting sublingual gland
Mandibular tori
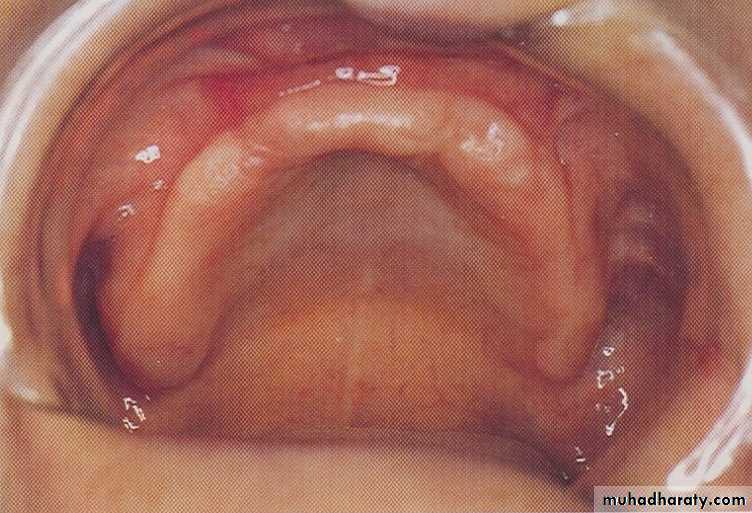
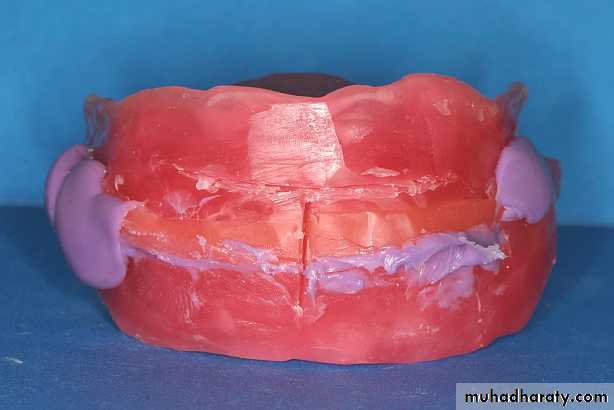
Flabby Tissue
A selective pressure impression technique
Sufficient relief and escape hole drilled in special tray opposite to flabby tissue to ensure relief of pressure over this area and proper load distribution.A sectional impression technique (Two part impression technique)
Vertical dimension:
Certain acts must be taken into consideration during determining the vertical dimension.The interocclusal distance increases with age. Excessive restoration of the vertical dimension to achieve a more youthful appearance is contraindicated.
Properly constructed bite blocks support the lips and improve the facial appearance are necessary.
In severe cases of over closure of patient’s old dentures it must be done over a period of time gradual elevations.
The vertical dimension should be opened no more than 5 mm at any one time. After a period of a few years, the dentures can be remade and the interocclusal distance increases another 3 to 4 mm.
• An interocclusal distance of 5 to 10 mm may be indicated because of physiologic changes in the facial musculature, alveolar bone, skin, and sensory perception.
Centric relation:
The determination of centric relation must be precise and accurate and not left to chance• Posterior tooth selection:
• The arrangement of posterior teeth plays a significant part in the retention and stability of the dentures.• Many Prosthodontist recommend zero degree posterior teeth according to zones be as follows:
• More adaptable for class II and III
• More easily for width variation of jaws
• Eliminate the horizontal forces
• Less time consuming technique and offer greater comfort and efficiency for a longer period.
• If anatomic teeth are used for an aged person, balanced occlusion is necessary to ensure no interference with jaw movements.
Selection and setting up of teeth:
Cross-linked cusp-less acrylic teeth to decrease lateral force to increase stability
Set up the teeth in neutral zone to increase denture stability.
Non anatomic or cross linked zero degree teeth with curves or ramps.
Zero degree teeth with reverse lateral curve (curve of Pleasure)
Adjustment
The insertion usually followed by irritation and trauma in varying degrees. The geriatric patient should be seen the day after insertion or at least the second day, depending upon the condition the patient can remove one or both dentures during the day if their mouth feels tired after adjustment period.Home care of complete denture should be stressed throughout the adjustment period.