Regional
Anaesthesia
Local Anaesthetic
Agents
Dr. Ali Hadi
Dr.Ali Hadi
1
Local Anesthetics- History
1860 - cocaine isolated from erythroxylum
coca
Koller - 1884 uses cocaine for topical
anesthesia
Halsted - 1885 performs peripheral nerve
block with local
Bier - 1899 first spinal anesthetic
Local Anesthetics - Definition
A substance which reversibly
inhibits nerve conduction when
applied directly to tissues at non-
toxic concentrations
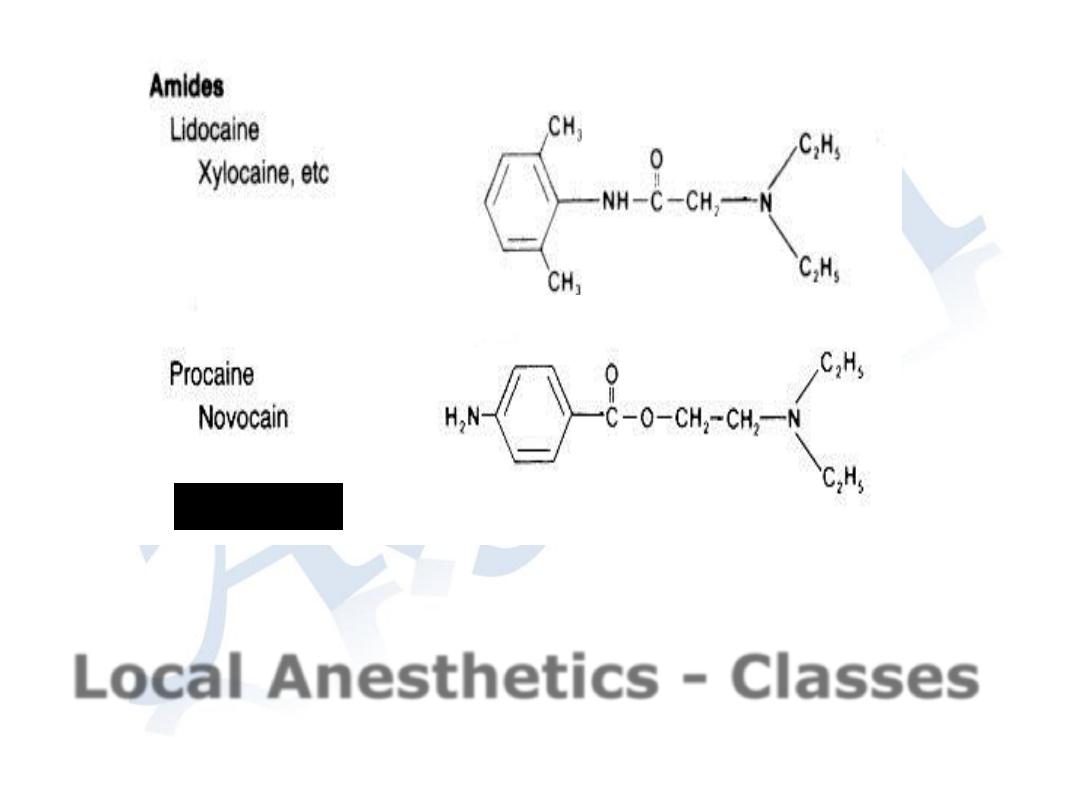
Local Anesthetics - Classes
Esters
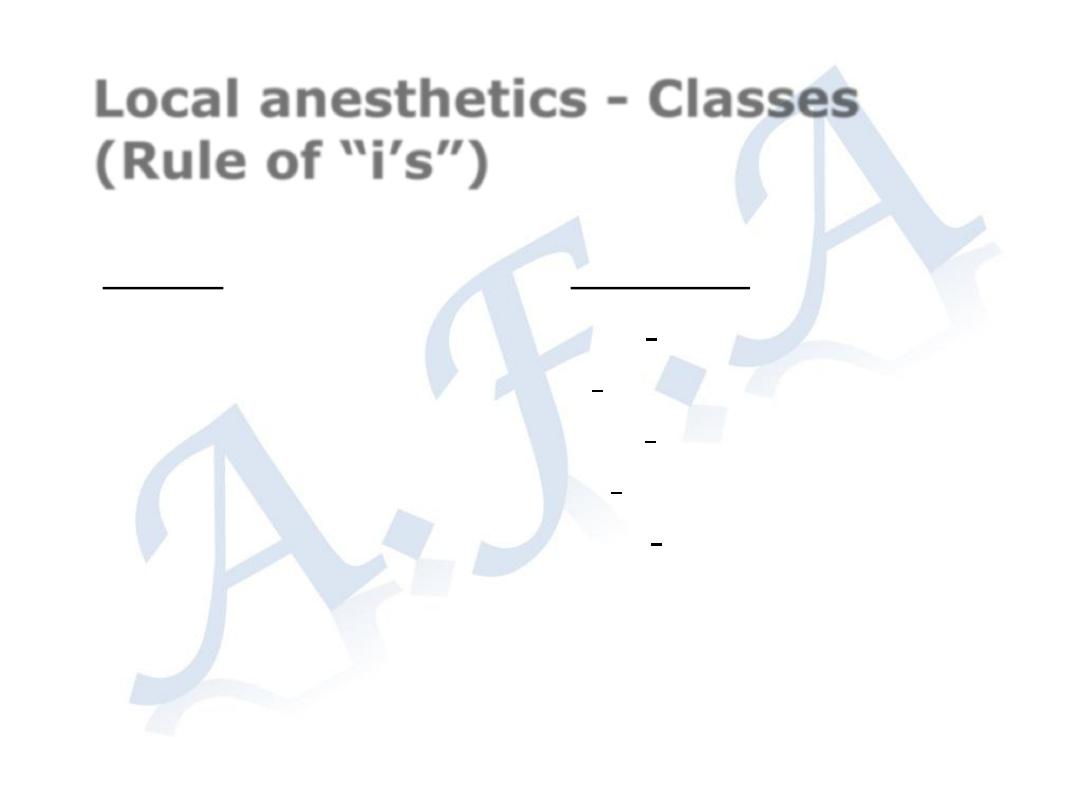
Local anesthetics - Classes
(Rule of “i’s”)
Esters
Cocaine
Chloroprocaine
Procaine
Tetracaine
Am”i”des
Bupivacaine
Lidocaine
Ropivacaine
Etidocaine
Mepivacaine
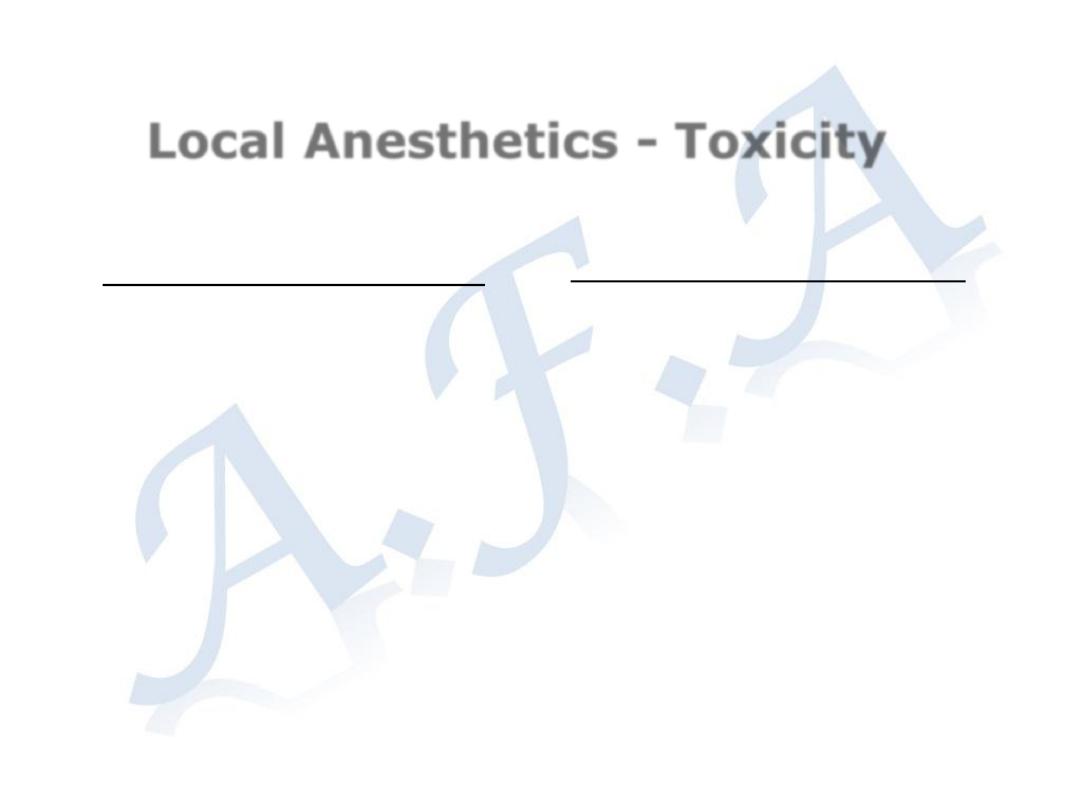
Local Anesthetics - Toxicity
Tissue toxicity - Rare
Can occur if
administered in high
enough
concentrations
(greater than those
used clinically)
Usually related to
preservatives added
to solution
Systemic toxicity - Rare
Related to blood level
of drug secondary to
absorption from site of
injection.
Range from
lightheadedness,
tinnitus to seizures
and
CNS/cardiovascular
collapse
Local anesthetics - Duration
Determined by rate of elimination
of agent from site injected
Factors include lipid solubility, dose
given, blood flow at site, addition
of vasoconstrictors (does not
reliably prolong all agents)
Some techniques allow multiple
injections over time to increase
duration, e.g. epidural catheter

Local anesthetics -
vasoconstrictors
Ratios
Epinephrine is added to local anesthetics
in extremely dilute concentrations, best
expressed as a ratio of grams of
drug:total cc’s of solution. Expressed
numerically, a 1:1000 preparation of
epinephrine would be
1 gram epi
1000 cc’s solution
1000 mg epi
1000cc’s solution
=
1 mg epi
1 cc
=
Local anesthetics -
vasoconstrictors
Therefore, a 1 : 200,000 solution of epinephrine would be
1 gram epi
200,000 cc’s solution
=
1000 mg epi
200,000 cc’s solution
or
5 mcg epi
1 cc solution
REGIONAL ANESTHESIA
Regional anesthesia -
Definition
Rendering a specific area of the
body, e.g. foot, arm, lower
extremities, insensate to
stimulus of surgery or other
instrumentation
Regional anesthesia - Uses
Provide anesthesia for a surgical
procedure
Provide analgesia post-operatively or
during labor and delivery
Diagnosis or therapy for patients with
chronic pain syndromes
Regional anesthesia - types
Topical
Local/Field
Intravenous block (“Bier” block)
Peripheral (named) nerve, e.g.
radial n.
Plexus - brachial, lumbar
Central neuraxial - epidural, spinal
Topical Anesthesia
Application of local anesthetic to
mucous membrane - cornea,
nasal/oral mucosa
Uses :
◦
awake oral, nasal intubation, superficial
surgical procedure
Advantages :
◦
technically easy
◦
minimal equipment
Disadvantages :
◦
potential for large doses leading to toxicity
Local/Field Anesthesia
Application of local subcutaneously to
anesthetize distal nerve endings
Uses:
◦
Suturing, minor superficial surgery, line
placement, more extensive surgery with
sedation
Advantages:
◦
minimal equipment, technically easy, rapid
onset
Disadvantages:
◦
potential for toxicity if large field
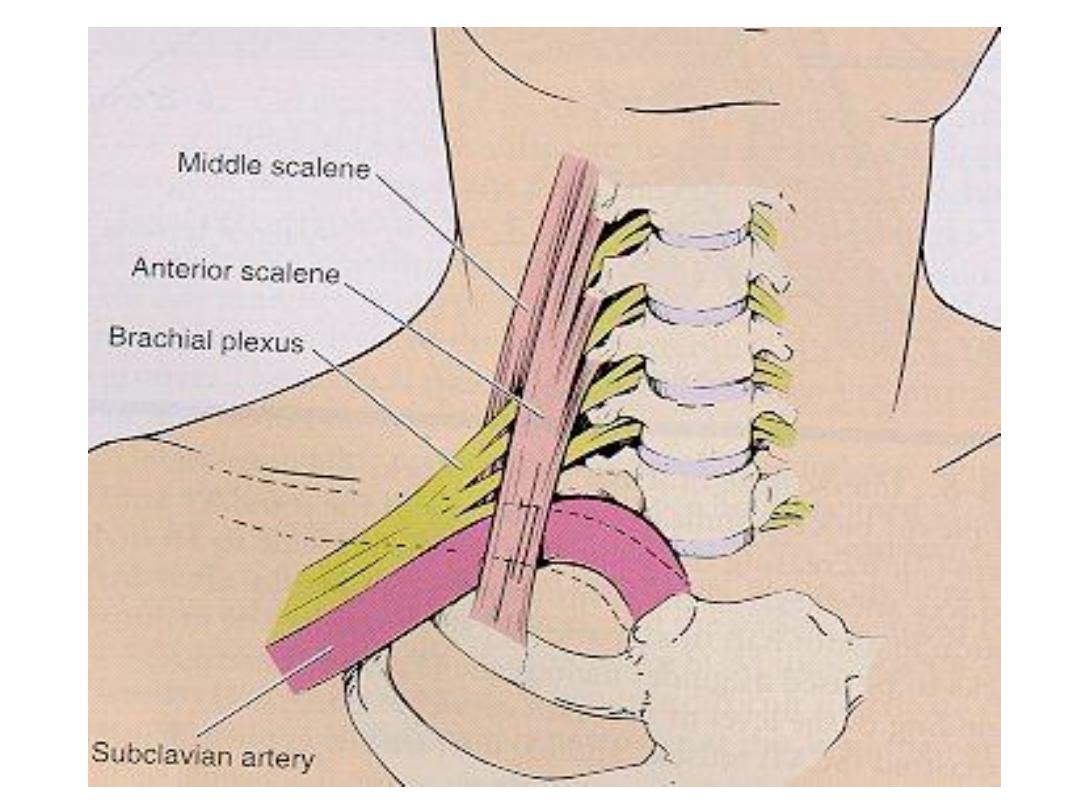
Plexus Blockade
Injection of local anesthetic adjacent to a
plexus, e.g cervical, brachial or lumbar
plexus
Uses :
◦
surgical anesthesia or post-operative analgesia
in the distribution of the plexus
Advantages:
◦
large area of anesthesia with relatively large
dose of agent
Disadvantages:
◦
technically complex, potential for toxicity and
neuropathy.
Central neuraxial blockade -
“Spinal”
Injection of local anesthetic into CSF
Uses:
◦
profound anesthesia of lower abdomen and
extremities
Advantages:
◦
technically easy (LP technique), high success
rate, rapid onset
Disadvantages:
◦
“high spinal”, hypotension due to sympathetic
block, post dural puncture headache.
Central Neuraxial Blockade -
“epidural”
Injection of local anesthetic in to the
epidural space at any level of the spinal
column
Uses:
◦
Anesthesia/analgesia of the thorax, abdomen,
lower extremities
Advantages:
◦
Controlled onset of blockade, long duration when
catheter is placed, post-operative analgesia.
Disadvantages:
◦
Technically complex, toxicity, “spinal headache”

Dr.Ali Hadi
Mechanism of action of spinal anaesthesia
Neural transmission of impulses in the nerve roots or possibly the
spinal cord itself is interrupted by the local anaesthetic ; progession
of the blockade may require10-15minutes.The nerve fibers vary in
function ,diameter ,and thickness of myelin sheath ,which affects
susceptibility to local anaesthetics. Preganglionic autonomic fibers (B
fibers)are small and more permeable to local anaesthetic than the
larger C fibers.Sympathetic blockage is found 1-2 segment above the
sensory block and motor blockage 1-2 segments below the sensory
block.
Advantages of spinal anaesthesia over general
anaesthesia
1.Less metabolic response to surgery
.
2.Reduction in blood loss 20-30%.
3.50% less thromboembolic complications.
4.Less pulmonary complications,no need for E.T.I. Less
risk of gastic aspiration.
5.Less risk of CVScomlications.
6.In obstetric anaesthesia and analgesia less effect of
drugs on mother and baby.
21

Dr.Ali Hadi
Indications for SAB anaesthesia
SAB is most suited to surgery below the umblicus and in this sit-
uation a patient may remain awake.
Uses
1.For prostatectomy where bloodless field is desired.
2.For open prostatectomy and gynaecological surgery.
3.For rapid onset of analgesia in obstetrics,forceps delivery
,removal of retained piece of placenta.
4.For patients with medical problems,a low SAB may be the
anaesthetic of choice,e.g.
a.Metabolic disease –DM .thyrotoxicosis.
b.Respiratory disease.
c.Cardiovascular disease.
5.For vaginal or operative obstetric delivery.
Contraindications to SAB and extradural anaesthesia
Absolute
1Patient refusal.
2.Sepsis with hemodynamic instability.
3.Uncorrected hypovolaemia.
4.Coagulopathy.
22

Dr.Ali Hadi
Relative contraindications
1.Elevated intracranial pressure.
2.Prior back ingury with neurologic deficit.
3.Progressive neurologic disease, such as multiple sclerosis.
4.Chronic back pain.
5.Localised infection near the site of ingection.
Complications
1.Hypotention.
2.Headache.
3.Urenary retention.
4.Bradycardia
5.Nausia and vomiting
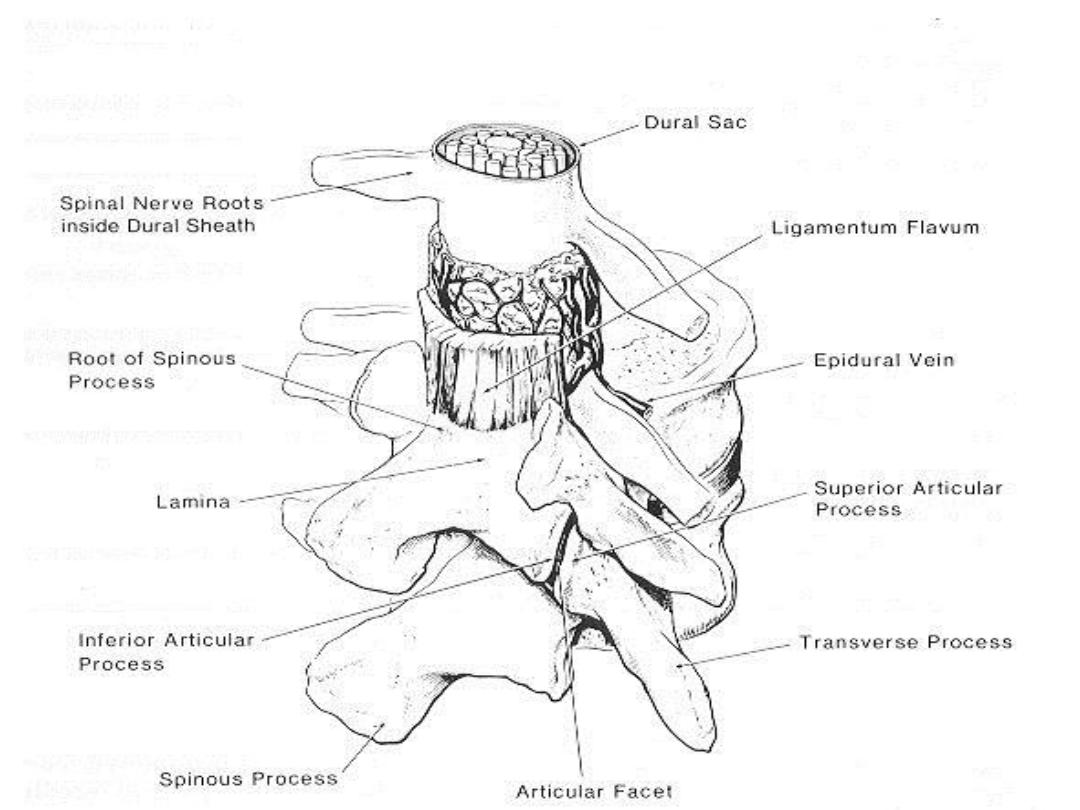
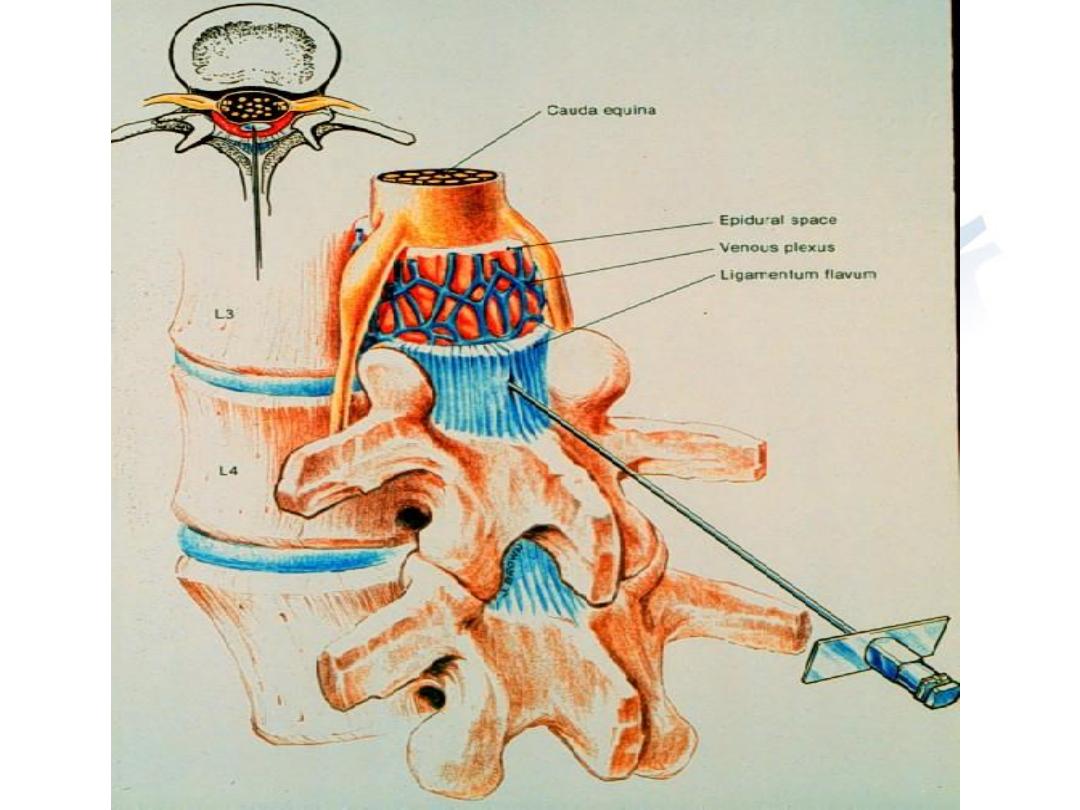
Epidural Anaesthesia
The epidural space lies just outside the dural sac containing the
Spinal cord and the CSF .The epidural needle pass through:
1.Skin.2.Subcutaneous fat.3.Supraspinous
ligament.4.Interspinous ligament.5. Ligamentum flavum
6.Epidural space.
23

Local anaesthesia may be used as an alternative or as an adjunct
to general anaesthesia .The use of long acting local anaesthetic
drugs produces useful analgesia in the immediate postoperative
period and this may be extended by the use of catheter
techniques(with epidural block)into the whole of the
postoperative period.
Spinal anaesthesia is produced by the injection of local
anaesthetic solution into the subarachnoid space where it mixes
with c.s.f.
Factors influencing spread hyperbaric spinal solutions
1.Position of the patient.
2.Spinal curvature.
3.Speed of injection.
4.Barbutage.
5.Interspace chosen.
6.Volume of local anaesthetic.
7.Dose of drug.
8.Sp.gr.of drug.
9.Fixation.
Dr.Ali Hadi
24

Dr.Ali Hadi
Advantages of Epidural over spinal anaesthesia
1.Epidural anaesthsia can produce a segmental block focused
on area of surgery or pain.
2.The gradual onset of sympathetic block allows time to
manage associated hypotention.
3.Duration of anaesthesia can be prolonged by using epidural
catheter.
4.There is more flxibility in the density of the block.
5.Decreased incidence of headache.
Brachial plexus block
Intravenous Regional Analgesia
27

Dr.Ali Hadi
Local anaesthetic agents
Local anaesthetic drugs act by producing a reversible block to
the transmission of periphral nerve impulses.
Structure of local anaesthetic drugs
Aromatic ---Intermediate ----Amine
Group chain
Amide or ester
Esters : are local anaesthetics whose intermediate chain forms an
ester link between the aromatic and amine group like
procaine,Cocaine,tetracaine.
Amide:
are local anaesthetics which an amide link between the
Aromatic and amine groups;like lidocain,bupivacaine.
Metaboliessim
Esters undergo hydrolysis by pseudocholinesterase .
Amide
undergo biotransformation in the liver through aromatic
Hydroxylation, N-dealkylation,and amide hydrolysis.
Mecmanism of action
1.Diffusion of the unionised (base)form across the nerve sheath and
membrane.
2.Re-equilibration between the base and cation forms in the
axoplasm
28

Dr.Ali Hadi
3.Binding of the cation to the receptor site inside the Na ion channel
Resulting in its blockade and inhibition of Na ion conductance.
Toxicity
CNS :Lightheadness , perioral numbness.tinnitus,confusion.
Muscle twitching,auditory and visual hallucination.
Tonic-clonic seizure,unconciosness,respiratoy arrest.
Cardiac
Hypertention,tachycardia
Hypotention,decrease contractility and COP.
Sinus bradycardia,ventricular dysryhthmias,circulatory arrest.
29
