
Psychiatry
Lecture 27: Psychosomatic Medicine
STRESS AND HEALTH
Psychological factors affecting health
Psychological factors may initiate or exacerbate symptoms of medical disorders
(psychosomatic symptoms) involving almost all body systems. These factors include:
1.
Poor health behavior (e.g., smoking, failure to exercise).
2.
Maladaptive personality style (e.g., type A personality).
3. Chronic or acute life stress caused by emotional (e.g., depression), social (e.g., divorce), or
economic (e.g., job loss) problems.
Mechanisms of the physiologic effects of stress
Acute or chronic life stress leads to activation of the autonomic nervous system , which
in turn affects cardiovascular and respiratory systems.
Stress also leads to altered levels of neurotransmitters (e.g., serotonin, norepinephrine),
which result in changes in mood and behavior.
Stress can increase the release of adrenocorticotropic hormone (ACTH), which leads to
the release of cortisol, ultimately resulting in depression of the immune system as
measured by decreased lymphocyte response to mitogens and antigens and impaired
function of natural killer cells.
Stressful life events
High levels of stress in a patient's life may be related to an increase d likelihood of
medical and psychiatric illness.
The Social Re adjustment Rating Scale by Holmes and Rahe (which also includes
"positive" events like holidays) ranks the effects of life events (see the table below).
Events with the highest scores require people to make the most social readjustment in
their lives.
The need for social readjustment is directly correlated with increased risk of medical
and psychiatric illness; in studies by Holmes and Rahe, 80% of patients with a score of
300 points in a given year became ill during the next year.
Other psychosomatic relationships
Medical conditions that can present with psychiatric symptoms, such as depression,
include neurologic illnesses (e.g., dementia), neoplasm (particularly pancreatic or other
gastrointestinal cancers), endocrine disturbances (e.g., hypothyroidism, diabetes), and
viral illnesses (e.g., AIDS).
Non-psychotropic medications can produce psychiatric symptom s such as confusion
(e.g., antiasthmatics), anxiety (e.g., antiparkinson agents), depression (e.g.,
antihypertensives), sedation (e.g., antihistamines), agitation (e.g., steroid hormones),
and even psychotic symptoms (e.g., analgesics, antibiotics, antihistamines).
Medical conditions such as diabetes and medications such as antihypertensives also
commonly produce sexual symptom s such as erectile dysfunction. These symptoms in
turn can lead to depression or other psychiatric problems in patients.
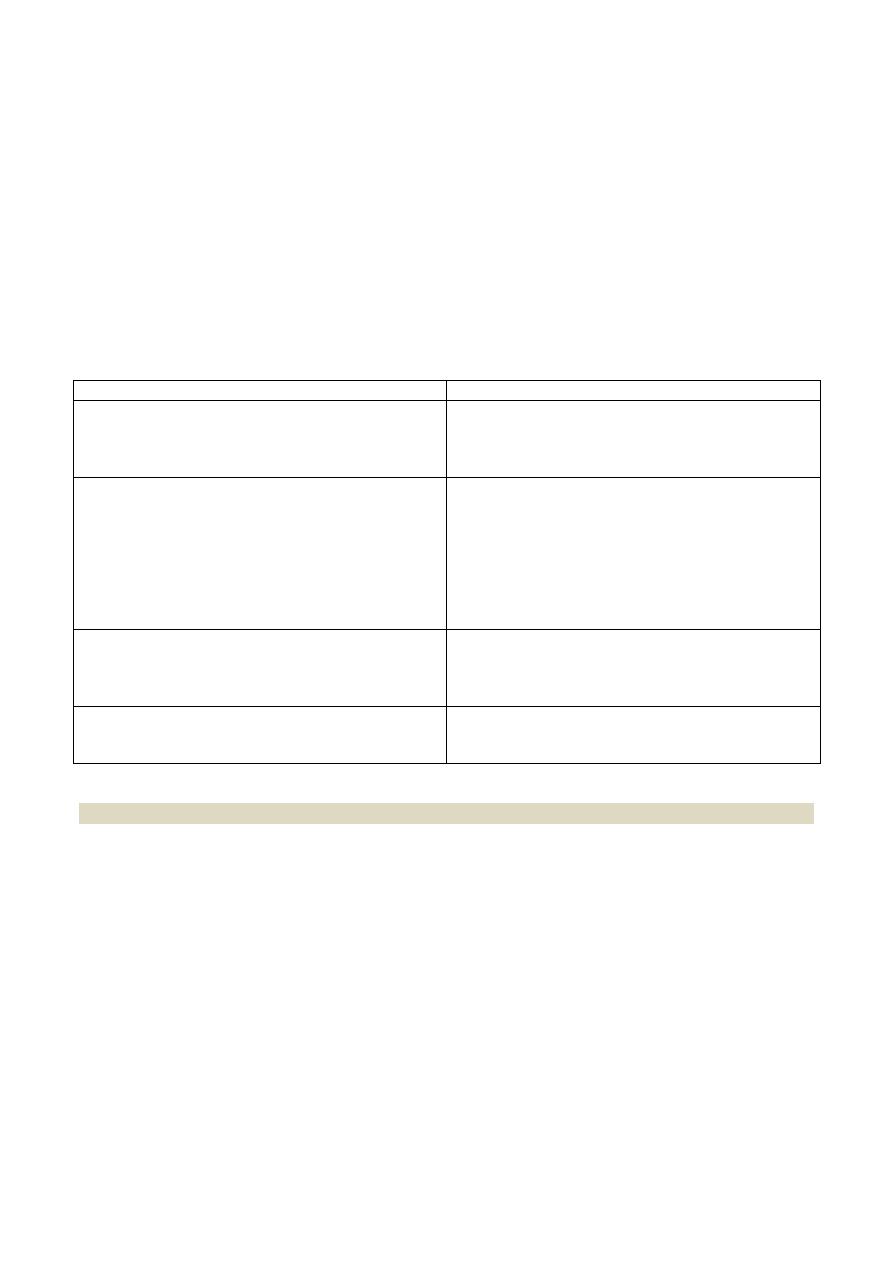
MAGNITUDE OF STRESS ASSOCIATED WITH SELECTED LIFE EVENTS ACCORDING TO
THE HOLMES AND RAHE SOCIAL READJUSTME
N
T RATING SCALE
لالطالع
Relative Stressfulness
Life Event (Exact Point Value of Stressor)
Very high
Death of a spouse (100)
Divorce (73)
Marital separation (65)
Death of a close family member (63)
High
Major personal loss of health because of illness
or injury (53)
Marriage (50)
Job loss (47)
Retirement (45)
Major loss of health of a close family member
(44)
Birth or adoption of a child (39)
Moderate
Assuming major debt (e.g., taking out a
mortgage) (31)
Promotion or demotion at work (29)
Child leaving home (29)
Low
Changing residence (20)
Vacation (15)
Major holiday (12)
PSYCHOLOGICAL STRESS IN SPECIFIC PATIENTS
Overview
Not uncommonly, medical and surgical patients have concurrent psychological
problems. These problems cause psychological stress, which can exacerbate the
patient's physical disorder.
Usually, the treating physician handles these problems by helping to organize the
patient's social support system s and by using specific psychotropic medications.
For severe psychiatric problems (e.g., psychotic symptoms) in hospitalized patients,
consultation–liaison (CL) psychiatrists may be needed.
Hospitalized patients
Common psychological complaints in hospitalized patients include anxiety, sleep
disorders, and disorientation, often as a result of delirium.
Patients who are at the greatest risk for such problems include those undergoing
surgery,
or renal dialysis, or those being treated in the intensive care unit (ICU) or
coronary care unit (CCU).
Patients undergoing surgery who are at greatest psychological and medical risk are
those who believe that the y will not survive surgery as well as those who do not admit
that they are worried before surgery.
Patients treated in the ICU or CCU because their illnesses are often life threatening are
at increased risk for depression and delirium (ICU psychosis).
Psychological and medical risk can be reduced by enhancing sensory and social input
(e.g., placing the patient's bed near a window, encouraging him or her to talk), providing
information on what the patient can expect during and after a procedure, and allowing
the patient to control the environment (e.g., lighting, pain medication) as much as
possible.
Patients undergoing renal dialysis
Patients on renal dialysis are at increased risk for psychological problems (e.g.,
depression, suicide, and sexual dysfunction) in part because their lives depend on other
people and on machines.
Psychological and medical risk can be reduced through the use of in-home dialysis units,
which cause less disruption of the patient's life.
Patients with sensory deficits
Patients with sensory deficits such as blindness or deafness are also at increased psychological
risk in part because they can become more easily disoriented when ill.
Permitting such patients to use their support technology or helper animals, e.g., hearing aid,
seeing-eye dog, can increase a patient's sense of control and thus reduce his or her stress
during illness.
PATIENTS WITH CHRONIC PAIN
Psychosocial factors
Chronic pain (pain lasting at least 6 months) is a commonly encountered complaint of
patients. It may be associated with physical factors, psychological factors, or a
combination of both.
Decreased tolerance for pain is associated with depression, anxiety, and life stress in
adulthood and physical and sexual abuse in childhood. Pain tolerance can be increased
through biofeedback, physical therapy, hypnosis, psychotherapy, meditation, and
relaxation training.
Chronic pain often leads to a loss of independence, which can lead to depression.
Practical suggestions for self care as well as pain relief can be helpful for such patients.
Depression may predispose a person to develop chronic pain. More commonly, chronic
pain results in depression.
People who experience pain after a procedure have a higher risk of morbidity and
mortality and a slower recovery from the procedure.
Religious, cultural, and ethnic factors may influence the patient's expression of pain and
the responses of the patient's support system s to the pain.
Treating pain
Relief of pain caused by physical illness is best achieved by analgesics (e.g., opioids),
using patient controlled analgesia (PCA), or nerve-blocking surgical procedures.
Antidepressants, particularly tricyclics, are useful in the management of pain.
Antidepressants are most useful for patients with arthritis, facial pain, and headache.
Their analgesic effect may be the result of stimulation of efferent inhibitory pain
pathways. Although they have direct analgesic effects, antidepressants may also
decrease pain indirectly by improving symptom s of depression.
According to the gate control theory, the perception of pain can be blocked by electric
stimulation of large-diameter afferent nerves. Some patients are helped by this
treatment.
Patients with pain caused by physical illness also benefit from behavioral, cognitive ,
and other psychological therapies, by needing less pain medication, becoming more
active, and showing increased attempts to return to a normal lifestyle.
Programs of pain treatment
Scheduled administration of an analgesic before the patient requests it (e.g., every 3
hours) and PCA are more effective than medication administered when the patient
requests it (on demand). Scheduled administration separates the experience of pain
from the receipt of medication.
Many patients with chronic pain are under medicated because the physician fears that
the patient will become addicted to opioids. However, recent evidence shows that
patients with chronic pain easily discontinue the use of opioids as the pain remits.
Pain patients are at higher risk for depression than they are for drug addiction.
Pain in children
Children feel pain and remember pain as much as adults do.
Because children are afraid of injections, the most useful ways of administering pain
medications to them are orally (e.g., a fentanyl "lollipop"), transdermally (e.g., a skin cream to
prevent pain from injections or spinal taps), or, in older children and adolescents, via PCA.
PATIENTS WITH ACQUIRED IMMUNE DEFICIENCY SYNDROME
Psychological stressors
Acquired immune deficiency syndrome (AIDS) and HIV-positive patients must deal with
particular psychological stressors not seen together in other disorders.
These stressors include having a fatal illness, feeling guilty about how they contracted
the illness (e.g., sex with multiple partners, intravenous drug use) and about possibly
infecting others, and being met with fear of contagion from medical personnel, family,
and friends.
HIV-positive homosexual patients may be compelled (because of their illness) to "come
out" (i.e., reveal their sexual orientation) to others.
Medical and psychological counseling can reduce medical and psychological risk for
HIV-positive patients.
It is important to note that psychiatric symptoms such as depression or psychosis in
AIDS patients may also result from infection of the brain with HIV or with an
opportunistic infection such as group B streptococcus.
Contagion
If they comply with methods of infection control, HIV -positive physicians do not risk
transmitting the virus to their patients.
Few health care workers have contracted HIV from patients. The main risk of
transmission is through accidental contamination from needles and other sharps,
although this risk is very low. Physicians can identify their HIV-positive patients to
those they put at imminent risk (e.g., sexual partners).
The End
