Psychiatry
Lecture 25: Child psychiatry
Intellectual disability
The term
intellectual disability (ID) is increasingly being used instead of mental retardation.
ID or mental retardation is defined as
a condition of arrested or incomplete development of the
mind, which is especially characterized by impairment of skills manifested during the
developmental period, which contribute to the overall level of intelligence, i.e., cognitive,
language, motor, and social abilities.
EPIDEMIOLOGY
There have been many surveys to ascertain the prevalence of ID across the world with
estimates ranging from 1% to 3%. Prevalence is higher in males in both adult and child and
adolescent populations.
ETIOLOGY AND RISK FACTORS
Etiology of ID is heterogeneous. Injury, infections and toxins have become less prevalent
causes because of improved antenatal care, while genetic factors have become more
prominent.
No specific etiology can be found in up to 40% of cases, particularly in mild ID.
Environmental influences (e.g., malnutrition, emotional and social deprivation
experienced, for example, in poorly run orphanages) can also cause or aggravate ID.
Trisomy 21 and fragile X are the commonest diagnosable genetic causes of intellectual
disability.
COMMON CONDITIONS ASSOCIATED WITH INTELLECTUAL DISABILITY
Down syndrome
Fragile-X syndrome
Phenylketonuria
Congenital hypothyroidism
Prader-Willi syndrome
Angelman Syndrome
Galactosemia
Fetal alcohol syndrome
Intelligence quotient (IQ)
IQ is a score derived from one of several tests. There are many types of IQ tests that
seek to measure general or specific abilities: reading, arithmetic, vocabulary, memory,
general knowledge, visual, verbal, abstract-reasoning etc.
Well-known IQ tests include the Wechsler Intelligence Scale for Children, Stanford-
Binet, Kaufman Assessment Battery for Children, and Raven’s Progressive Matrices.
Traditionally, an IQ score was obtained by dividing the mental age of the person taking
the test by the chronological age multiplied by 100.
DIAGNOSING INTELLECTUAL DISABILITY
According to both the DSM and ICD, three basic criteria should be met for
a diagnosis of intellectual disability (or mental retardation):
• Significantly sub average intellectual functioning (IQ of 70 or below).
• Concurrent deficits or impairments in adaptive functioning in at least two of the following
areas:
communication, self-care, home living, social/interpersonal skills, use of community
resources, self-direction, functional academic skills, work, leisure, health, and safety.
• Onset is before age 18 years.
MANIFESTATIONS AND SUBTYPES
The manifestations of ID are mainly developmental delay in intellectual functioning and
deficits in social adaptive functioning. According to the severity of the delay in intellectual
functioning, deficits in social adaptive function and IQ, the psychiatric classifications describe
four levels of severity:
Profound
IQ is usually below 20; profound intellectual disability accounts for 1% to 2% of all cases.
Severe
IQ is usually between 20 and 34; severe intellectual disability accounts for 3% to 4% of all
cases.
Moderate
IQ is usually between 35 and 49, accounting for about 12% of all cases.
Mild
IQ is usually between 50 and 69 and account for about 80% of all cases.
MANAGEMENT
In all cases of ID, the vital part of treatment is early detection and early intervention.
As no specific etiology can be found in up to 40% of cases and many known causes
cannot be cured, in the majority of cases, the aim of treatment is not a "cure" but to
minimize symptoms and disability through reducing risk (e.g., helping individuals to be
safe at home or school), teaching life skills, improve life quality and support families and
carers.
Detailed goals and modalities of treatment for each individual will largely depend on the
cause and severity of ID and co morbid conditions.

Attention Deficit Hyperactivity Disorder and Disruptive Behavior Disorders of
Childhood
Overview
1. Attention deficit hyperactivity disorder (ADHD) and the disruptive behavior disorders (e.g.,
conduct disorder and oppositional defiant disorder) are characterized by inappropriate
behavior that causes problems in social relationships and school performance.
2. There is no frank intellectual disability (mental retardation).
3. These disorders are not uncommon and are seen more often in boys.
4. Differential diagnosis includes mood disorders and anxiety disorders.
5. Characteristics and prognoses of these disorders can be found in the table below.
Epidemiology
Attention deficit hyperactivity disorder (ADHD) is one of the most common childhood onset
psychiatric disorders, affecting 12% of children worldwide. ADHD is a costly public health
concern since it can cause significant impairment in functioning that interferes with normal
development and all areas of functioning in patients of all ages.
Etiology
1. Genetic factors are involved. Relatives of children with conduct disorder and ADHD have an
increased incidence of these disorders and of antisocial personality disorder and substance
abuse.
2. Although evidence of serious structural problems in the brain is not present, children with
conduct disorder and ADHD may have minor brain dysfunction.
3. Substance abuse, serious parental discord, mood disorders, and child abuse are seen in some
parents of children with these disorders; these children are also more likely to be abused by
caretakers.
4. There is no scientific basis for claims of an association between ADHD and either improper
diet (e.g., excessive sugar intake) or food allergy (e.g., artificial colors or flavors).
Treatment
1. Pharmacologic treatment for ADHD consists of use of central nervous system (CNS)
stimulants including:
methylphenidate (Ritalin, Concerta), dextroamphetamine sulfate (Dexedrine), a combination
of amphetamine/dextroamphetamine, atomoxetine (Strattera), and dexmethylphenidate.
a. For ADHD, CNS stimulants apparently help to reduce activity level and increase attention
span and the ability to concentrate; antidepressants also may be useful.
b. Since stimulant drugs decrease appetite , they may inhibit growth and lead to failure to gain
weight; both growth and weight usually return to normal once the child stops taking the
medication.
2. Family therapy is the most effective treatment for conduct disorder and oppositional defiant
disorder
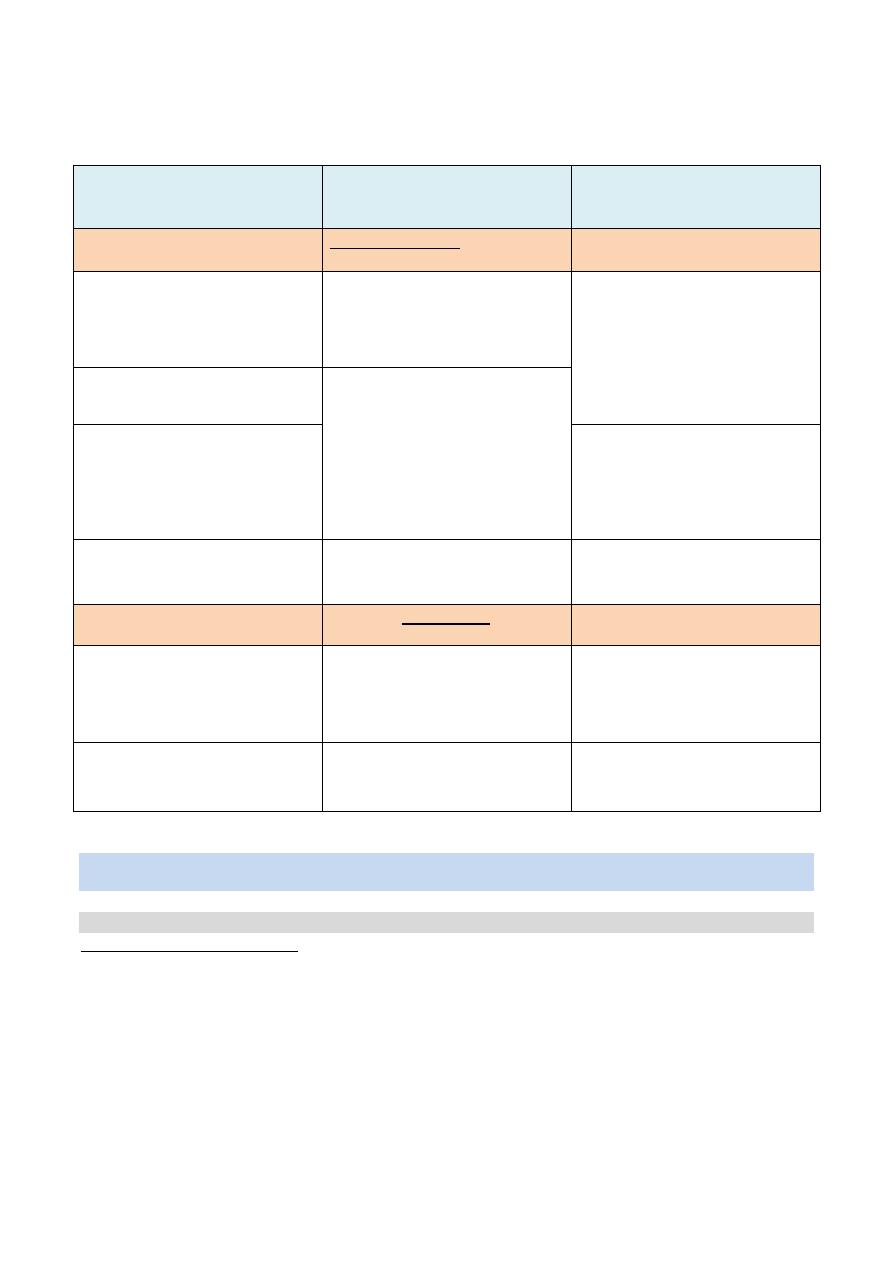
Table: Characteristics and Prognosis of Attention Deficit Hyperactivity Disorder, Conduct
Disorder, and Oppositional Defiant Disorder
Attention Deficit
Hyperactivity
Disorder (ADHD)
Conduct Disorder
Oppositional Defiant
Disorder
Characteristics
Hyperactivity
Inattention
Impulsivity
Carelessness
Behavior that grossly violates
social norms (e.g.,
torturing animals, stealing,
truancy, fire setting)
Behavior that, while defiant,
negative, and noncompliant,
does not grossly violate social
norms (e.g., anger,
argumentativeness,
resentment
toward authority
figures)
Propensity for accidents
History of excessive crying,
high
sensitivity to stimuli, and
Irregular sleep patterns in
infancy
Symptoms present before age
12 and in at least two settings
(e.g., home and school)
Can begin in childhood
(ages 6
–10) or adolescence
(no symptoms prior to age 10)
Gradual onset, usually before
age 8
Prognosis
Hyperactivity is the first
symptom to disappear as the
child reaches adolescence
Risk for criminal behavior,
antisocial personality
disorder, substance abuse, and
mood disorders in adulthood
A significant number of cases
progress to conduct disorder
Most children show remission
by adulthood
Most children show remission
by adulthood
Most children show remission
by adulthood
Autism spectrum disorders (ASD)
Characteristics
Severe form of ASD, include:
1. Significant problems with communication (despite normal hearing, significant lack of
social and language skills)
2. Significant problems forming social relationships (including those with caregivers, poor
eye contact, difficulty understanding facial expression)
3. Repetitive, purposeless behavior (e.g., spinning, self-injury)
Subnormal intelligence in many (26%–75%) autistic children
Unusual abilities in some children (e.g., exceptional memory or calculation skills). These
are referred to as savant skills.
Mild form of ASD (previously called Asperger disorder) involves:
1. Significant problems forming social relationships
2. Repetitive behavior and intense interest in obscure subjects (e.g., models of 1940s farm
tractors)
In contrast to autistic disorder, in Asperger disorder there is normal cognitive
development and little or no developmental language delay.
However, conversational language skills are impaired.
Occurrence of ASD
They occur in about 17 children per 10,000.
They begin before 3 years of age.
The disorders are four to five times more common in boys.
Abnormalities that give clues for the etiology of ASD
Cerebral dysfunction (no psychological causes have been identified)
A history of perinatal complications
A genetic component (e.g., the concordance rate for ASD is three times higher in
monozygotic than in dizygotic twins)
Immunologic incompatibility between mother and fetus
Smaller amygdala and hippocampus, fewer Purkinje cells in the cerebellum, and less
circulating oxytocin
Treatment of ASD
Early diagnosis and treatment helps young children with autism develop to their full potential. The
primary goal of treatment is to improve the overall ability of the child to function. The treatment
strategies may include:
Behavioral training and management: Behavioral training and management uses positive
reinforcement, self-help, and social skills training to improve behavior and communication.
Specialized therapies: These include speech, occupational, and physical therapy.
Medications:. Medications are most commonly used to treat related conditions and problem
behaviors, including depression, anxiety, hyperactivity, and obsessive-compulsive
behaviors.
Community support and parent training .
Case Example
A 4-year-old child who has never spoken voluntarily shows no interest in or connection to his parents,
other adults, or other children. His hearing is normal. His mother tells the doctor that he persistently
turns on the taps to watch the water running and that he screams and struggles fiercely when she tries
to dress him.
This child, who has never spoken voluntarily and who shows no interest in or connection to his parents,
other adults, or other children despite normal hearing, has autistic disorder, a pervasive developmental
disorder of childhood. He turns on the tap to watch the water running because, as with many autistic
children, repetitive motion calms him. Any change in his environment, such as being dressed, leads to
intense discomfort, struggling, and screaming.
Tourette disorder
Tourette disorder is characterized by involuntary movements and vocalizations (tics),
that may include the involuntary use of profanity (coprolalia). While these behaviors
can be controlled briefly, they must ultimately be expressed.
The disorder, which is lifelong and chronic, begins before age 18. It usually starts with a
motor tic (e.g., facial grimacing) that appears between ages 7 and 8.
While the manifestations are behavioral, the etiology of Tourette disorder is neurologic.
It is believed to involve dysfunctional regulation of dopamine in the caudate nucleus.
The disorder is three times more common in males and has a strong genetic component.
There is a genetic relationship between Tourette disorder and both ADHD and
obsessive-compulsive disorder.
Atypical antipsychotic agents (e.g., risperidone [Risperdal]) and typical agents (e.g.,
haloperidol) are the most effective treatments for Tourette disorder. In milder cases,
agents such as clonidine also are helpful.
Separation anxiety disorder
Often incorrectly called school phobia, because the child refuses to go to school, this
disorder is characterized by an overwhelming fear of loss of a major attachment figure,
particularly the mother.
The child often complains of physical symptoms (e.g., stomach pain or headache) to
avoid going to school and leaving the mother.
The most effective management of a child with this disorder is to have the mother
accompany the child to school and then, when the child is more comfortable, gradually
decrease her time spent at school.
Individuals with a history of separation anxiety disorder in childhood are at greater risk
for anxiety disorders in adulthood, particularly agoraphobia.
Selective mutism
Children (more commonly girls) with this rare disorder speak in some social situations
(e.g., at home) but not in others (e.g., at school); the child may whisper or communicate
with hand gestures.
Selective mutism must be distinguished from normal shyness.
The End
