Psychiatry
Lecture 23: The Physician-Patient Relationship
MEDICAL PRACTICE
Seeking medical care
Patients' behavior when ill and their expectations of physicians are influenced by:
their culture
previous experiences with medical care
physical and mental conditions
personality styles (not necessarily personality disorders) (see table below)
coping skills
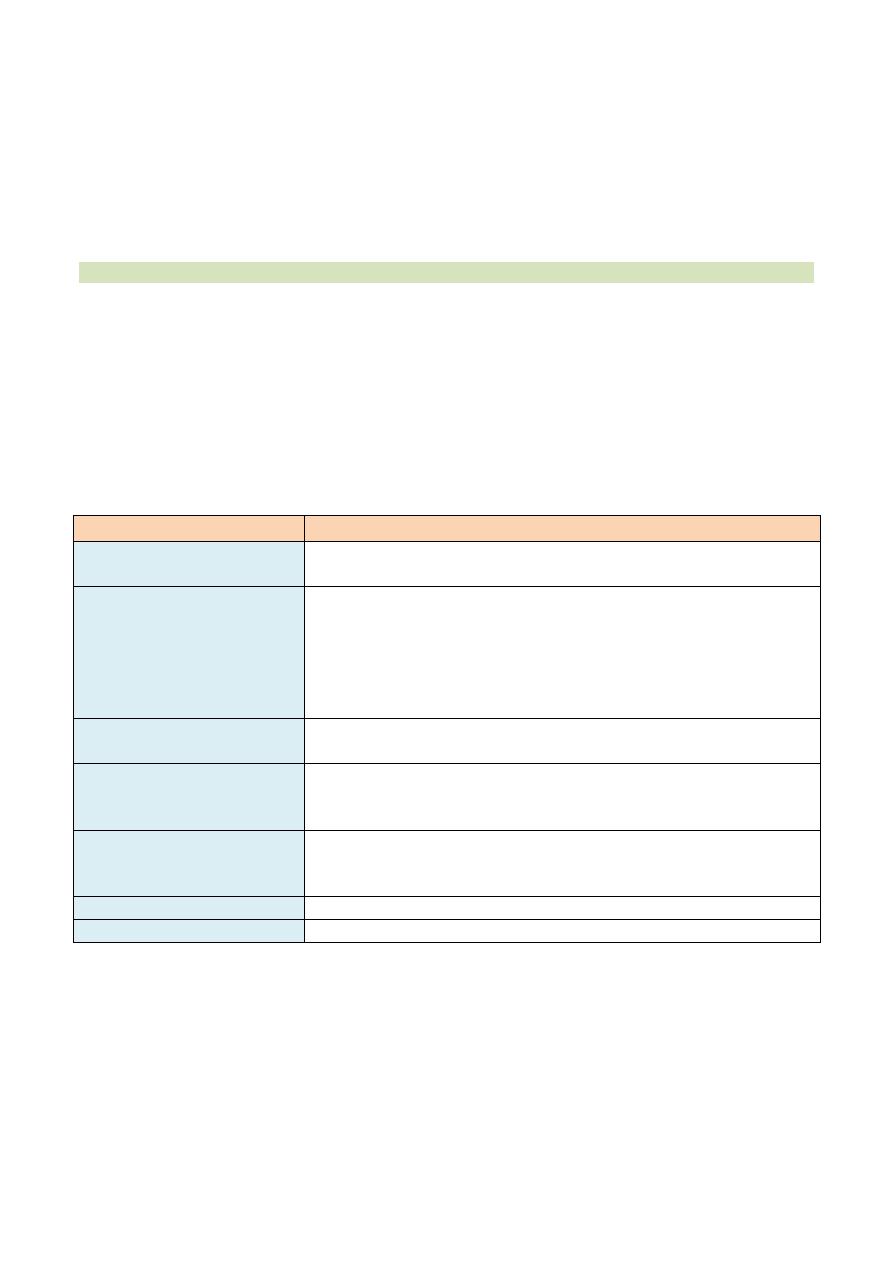
Patient Personality Style and Behavioral Characteristics During Illness
Behavioral Characteristics During Illness
Personality Style
Has a need to be cared for by others, resulting in the
desire for excessive attention from the physician during an illness
Dependent
Fears loss of control and may in turn become controlling
during illness
Characterized by time pressure (e.g., feels rushed most
of the time) and competitiveness
May also show hostility, which is associated specifically with the
development of coronary artery disease
Obsessive-compulsive and
type A
May be dramatic, emotionally changeable, and approach the
physician in an inappropriate sexual fashion during illness
Histrionic
Has a perfect self-image, which is threatened by illness
Often feels superior to others and therefore may request that only
the "top" physicians be involved in treatment
Narcissistic
Often blames the physician for the illness
Is overly sensitive to a perceived lack of attention or caring from the
physician
Paranoid
Asks for help but then does not comply with the physician's advice
Passive-aggressive
Becomes even more withdrawn during illness
Schizoid
Seeking psychiatric care
There are still attitudes within most societies that view symptoms of psychopathology as
threatening and uncomfortable, and these attitudes frequently foster stigma
and discrimination towards people with mental health problems.
It is important for patients to seek help since there is a strong correlation between
psychological illness and physical illness. Morbidity rates and mortality rates are much
higher in patients who need psychiatric attention.
The "sick role"
A person assumes a particular role in society and certain behavioral patterns when he
or she is ill (the "sick role," described by T. Parsons).
The sick role includes exemption from usual responsibilities and expectation of care by
others, as well as working toward becoming healthy and cooperating with health care
personnel in getting well.
Telling patients the truth
All adult patients should be told the complete truth about the diagnosis, the treatment
and its side effects, and the prognosis of their illness. Falsely reassuring or patronizing
statements in response to patient questions (e.g., "Do not worry, we will take good care
of you" or "You still have one child" [after a miscarriage]) are not appropriate.
Information about the illness must be given directly to the adult patient and not relayed
to the patient through relatives. Parents decide if, how, and when such information will
be given to an ill child.
With the patient's permission, the physician can tell relatives this information in
conjunction with, or after, telling the patient. Relieving the fears of close relatives of a
seriously ill patient can bolster the support system, and thus help the patient.
Special situations
Patients may be afraid to ask questions about issues that are embarrassing (e.g., sexual
problems) or fear-provoking (e.g., laboratory results).
A physician should not try to guess what is troubling a patient; it is the physician's
responsibility to ask about such issues in an open-ended fashion and address them
truthfully and fully with the patient.
Physicians have the primary responsibility for dealing with compliance issues, as well as
with angry , seductive , or complaining behavior by their patients (see Table below).
Referrals to other physicians should be reserved only for medical and psychiatric
problems outside of the treating physician's range of expertise.
COMPLIANCE (ADHERENCE)
Patient characteristics associated with compliance
Compliance or adherence refers to the extent to which a patient follows the instructions
of the physician, such as taking medications on schedule , having a ne e de d medical test
or surgical procedure, and following directions for change s in lifesty le , such as diet or
exercise.
Patients' unconscious transference reactions to their physicians, which are based in
childhood parent-child relationships, can increase or decrease compliance.
Only about one third of patients comply fully with treatment, one third comply some of
the time, and one third do not comply with treatment.
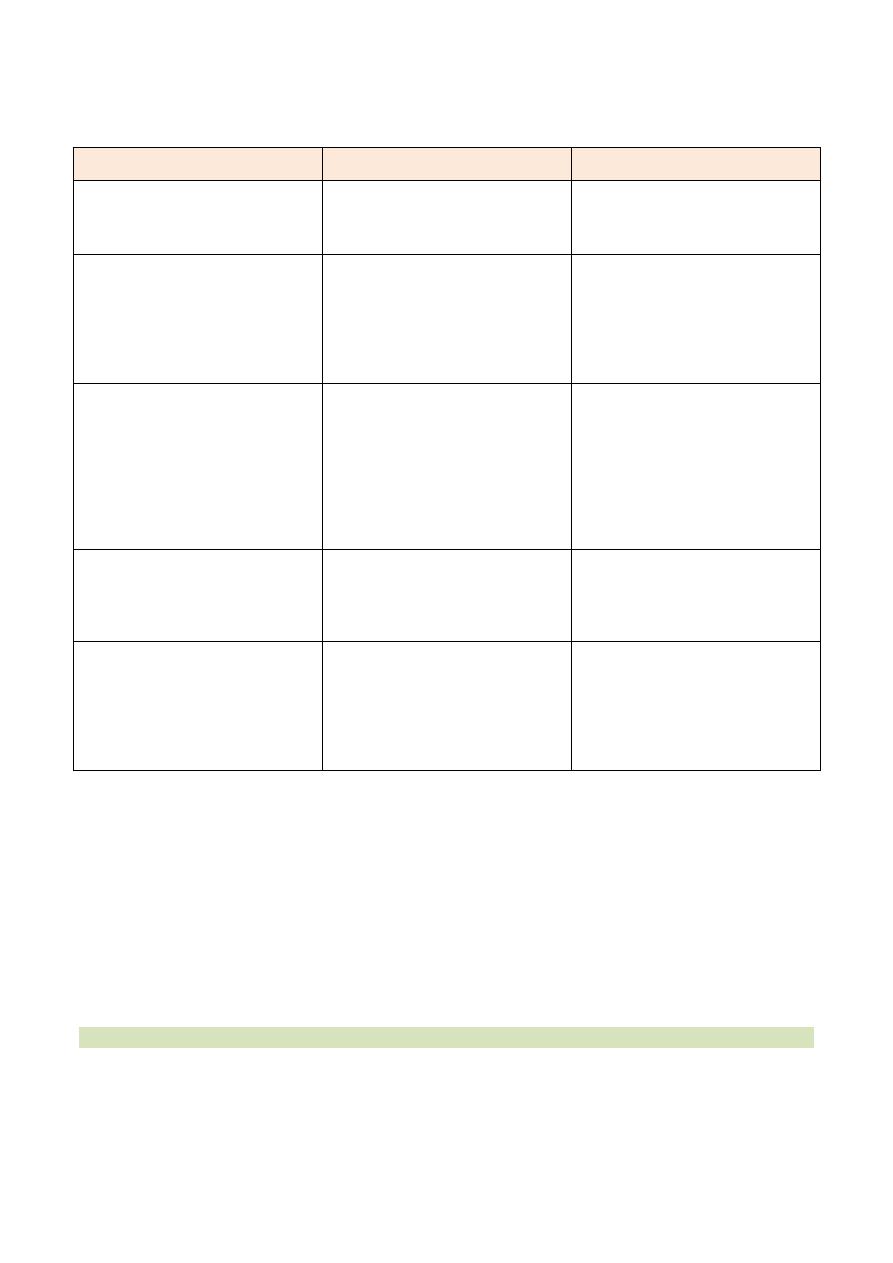
Common Problems in the Physician-Patient Relationship
لالطالع
Problem
Do
Do not
Angry patient
Do acknowledge the patient's
anger
Do not take the patient's anger
Personally (the patient is probably
fearful about becoming dependent as
well as of being ill)
Seductive patient
Do call in a chaperone when
you are with the patient
Do gather information using
direct rather than open-ended
questions
Do set limits on the behavior
that you will tolerate
Do not refuse to see the
patient
Do not refer the patient to
another physician
Non-compliant patient
Do examine the patient's
Willingness to change his or her
health threatening behavior (e.g.,
smoking); if he or she is not willing,
you must address that issue
Do identify the real reason for
The patient's refusal to comply
or to consent to a needed
intervention and address it (e.g., fear)
Do not attempt to scare the
patient into
complying (e.g., showing
frightening photographs of untreated
illness)
Do not refer the patient to
Another physician
Suicidal patient
Do assess the seriousness of
the threat
Do suggest that the patient
remain in the hospital voluntarily if
the threat is serious
Do not release a hospitalized
patient who is a threat to himself or
herself (patients who are a threat to
self or others can be
held involuntarily
Complaining patient
Do encourage the patient to
speak to the other physician directly if
the patient complains about a
relationship with another physician
Do speak to your own office staff if
the patient has a complaint
about one of them
Do not intervene in the patient's
relationship with another physician
unless there is a medical reason to do
so
Do not blame the patient for
problems with office staff
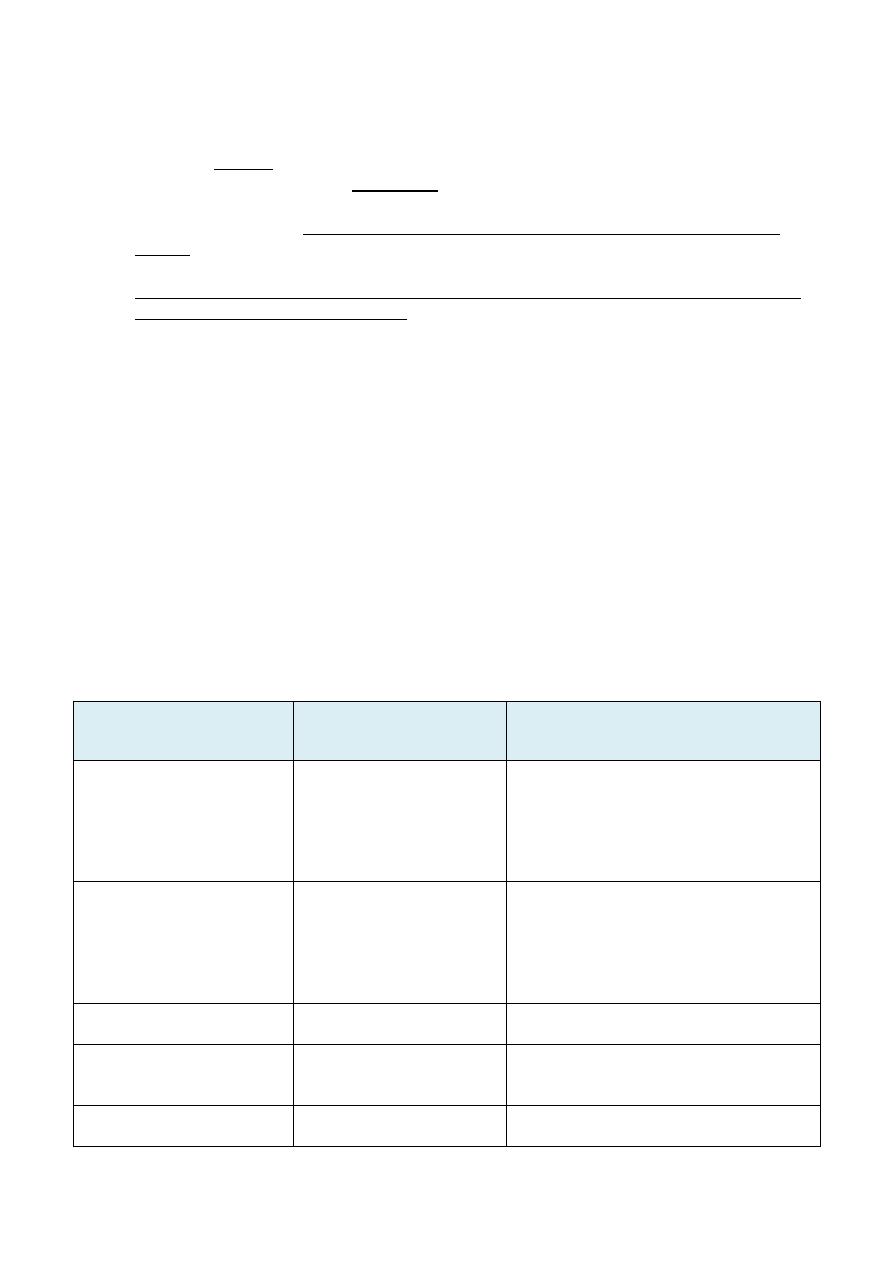
Factors that increase and decrease compliance
Compliance is not related to patient intelligence , education, sex, religion, race,
socioeconomic status, or marital status.
Compliance is most closely related to how well the patient likes the doctor. The strength
of the doctor-patient relationship is also the most important factor in whether or not
patients sue their doctors when an error or omission is made or when there is a poor
outcome.
Some factors associated with compliance are listed in Table below.
THE CLINICAL INTERVIEW
Communication skills
Patient compliance with medical advice, detection of both physical and psychological
problems, and patient satisfaction with the physician are improved by good physician-
patient communication.
One of the most important skills for a physician to have is how to interview patients.
The physical setting for the interview should be as private as possible. Ideally, there
should be no desk or other obstacle between the physician and patient, and the
participants should interact at eye level (e.g., both seated).
During the interview, the physician must first establish trust in and rapport with the
patient and then gather physical, psychological, and social information to identify the
patient's problem.
The physician should obtain backup (e.g., hospital security) as soon as it appears that a
patient is dangerous or threatening.
The interview serves to obtain the patient's psychiatric history , including information
about prior mental problems, drug and alcohol use, sexual activity, current living
situation, and sources of stress
.
Specific interviewing techniques
Direct questions: Direct questions are used to elicit specific information quickly from a patient
in an emergency situation (e.g., "Have you been shot?") or when the patient is seductive or
overly talkative.
Open-ended questions
Although direct questions c
a
n elicit information quickly, open-ended types of questions are
more likely to aid in obtaining information about the patient, and not close off potential
areas of pertinent information.
Using open-ended questions (e.g., "What brings you in today?"), the interviewer gives little
structure to the patient and encourages the patient to speak freely.
Factors Associated with Compliance with Medical Advice
Factors Associated
with Increased
Compliance
Factors Associated with
Decreased Compliance
Comments
Good physician-patient
relationship
Poor physician-patient
relationship
Liking the physician is the most important
factor in compliance; it is even more
important than the physician's technical
skill
Physicians perceived as unapproachable
have low compliance from patients
Patient feels ill and usual
activities are disrupted
by the illness
Patient experiences few
Symptoms and little
disruption of usual activities
In asymptomatic illnesses, such
as hypertension, only about half
of patients initially comply with treatment
Many asymptomatic patients who
initially complied have stopped complying
within 1 year of diagnosis
Short time spent in the
waiting room
Long time spent in the
waiting room
Patients kept waiting get
angry and then fail to comply
Belief that the benefits of
care outweigh its financial
and time costs
Belief that financial and
time costs of care outweigh
its benefits
The "Health Belief Model"
of health care
Written diagnosis and
Instructions for treatment
Verbal diagnosis and
Instructions for treatment
Patients often forget what is said during a
visit to the physician because they are
anxious
asking the patient to repeat your verbal
instructions can improve understanding and
thus increase compliance
Acute illness
Chronic illness
Chronically ill people see physicians more
often but are more critical of them than
acutely ill people
Recommending only one
behavioral change at a
time
Recommending multiple
behavioral
changes at once
To increase compliance, instruct the patient
to make one change (e.g., stop smoking)
this month, and make another
Change (e.g., go on a diet) next month
Recommending too many changes
at once will reduce the likelihood
that the patient will make any changes
Simple treatment
schedule
Complex treatment
schedule
Compliance is higher with medications that
require once daily dosing, preferably
With a meal
Patients are more likely to forget to
take medications requiring frequent or
between-meal dosing
Older physician
Younger physician
Usually young physician age is only
an issue for patients in the initial
stages of treatment
Peer support
Little peer support
Membership in a group of People with a
similar problem (e.g.,smoking) can
increase compliance
The End
