Management of patients receiving Chemotherapy and Radiotherapy
Medically compromised patientManagement of patients receiving Chemotherapy and Radiotherapy
Chemotherapy and Radiotherapy are used in the treatment of Cancer which is a disease characterized by uncontrolled neoplastic cells.Carcinogenesis is a multistep process that involves the accumulation of mutations that are either hereditary or acquired as a result of exposure to environmental factors such as chemicals and pathogens.
Signs and symptoms
They depend on the anatomical site involved (e.g. breast, uterine cervix, colorectal, lung, prostate, skin or oral cavity) and the cell type of origin.Oral Cancer
90% are squamous cell carcinoma (SCC). 9% arise from salivary gland tissues or other types of tissues e.g. Sarcoma and Lymphoma. The remaining 1 % are metastatic tumors from elsewhere in the body.• Oral SCC appears as:
• Leukoplakia.• Erythroplakia.
• Exophytic mass.
• Ulceration.
• A combination of the above.
When it involves the bone it causes destruction.
Oral SCC spread by local infiltration into surrounding
• tissues or by metastasis to regional lymph nodes. Distant metastasis is uncommon
Treatment of oral SCC
• Surgical resection.• Radiotherapy.
• Chemotherapy.
• Genetic and Immunotherapy (recent).
Dental management
1. Obtaining thorough history from the patient.2. Clinical examination for the head and neck region and the oral cavity is mandatory for every patient since the dentist may be the first one to recognize the disease, remembering two important points:
• In early stages, Cancer is either asymptomatic or shows few signs and symptoms.
• Cancer is most amenable to treatment when it is in early stages.
3. Lesions clinically suspicious for Carcinoma and those that fail to heal within 14 days biopsy should be taken.
4. Screening tests can be ordered including RBC count, WBC count with differential count, Hb, PCV and platelet count, abnormal results should be discussed with the physician.
5. planning involves:
• Pretreatment evaluation and preparation.
• Oral health care during therapy.
• Post-treatment management of patients.
Pretreatment evaluation and preparation
• Oral hygiene instructions and encouragement of non cariogenic diet.• Elimination of all sources of irritation and infection.
• Teeth that are non- restorable, infected or affected by severe periodontitis should be extracted 2-3 weeks prior to chemotherapy or radiotherapy.
• After completing the extraction any sharp edges should be trimmed.
• primary closure of the socket is recommended.
• Any hemostatic packing agents should be avoided.
• if the platelet count is below 50.000 cells/ml transfusion may be required,
• when WBC count is below 2000 cell/ml we should either delay the extraction if possible or give prophylactic antibiotics.
• It is recommended that dental treatment (restorative and prosthodontic) is provided before Cancer treatment if possible, but prosthodontic treatment can be delayed when time is limited. If chemotherapy or radiation are to be given, removable appliances should be removed during treatment.
Oral health care during therapy
During chemo and radiotherapy many complications arise some of them have early onset while other are late complications:Mucositis: result from the direct cytotoxic effects of radiotherapy and chemotherapy on the rapidly dividing mucosal epithelial cells, it appear as red, raw and tender mucosa with epithelial sloughing, It is managed by antiseptic mouth rinses, topical anesthetics, anti-inflammatory agents like steroids, the patient should be kept well hydrated and nourished with avoidance of alcohol, tobacco and irritating foods.
Xerostomia:
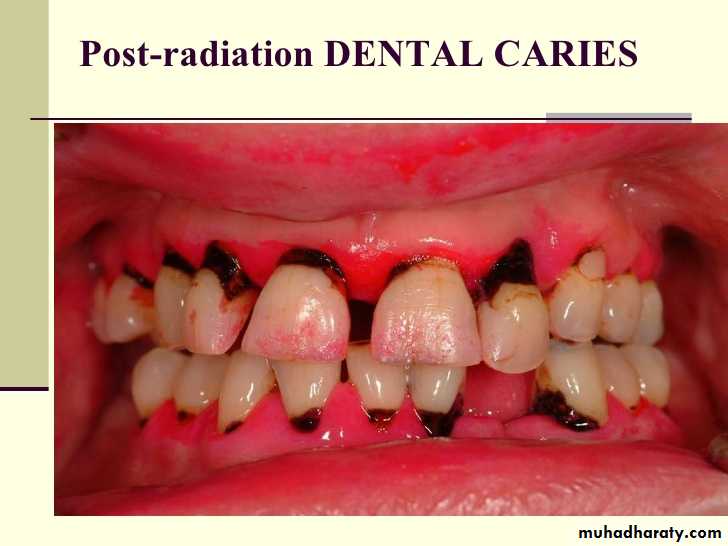
Results from salivary gland tissue damage (acinar atrophy, vascular changes and chronic inflammation) due to head and neck radiation. The degree of damage is directly related to the field and the dose of radiation. It is managed by frequent drinking of water, using salivary substitutes, sugarless chewing gum, lozenges and sialagogue drugs like Pilocarpine HCL (parasympathomimetic drug) to stimulate salivary flow.Radiation caries: arises mainly due to hypo-salivation in patient who received radiotherapy for the head and neck, it progresses rapidly leading to necrosis and periapical infection. Its management requires patient education, oral hygiene instructions, fluoride application, frequent dental visits and early restoration of teeth.
Secondary infections: occurs as a result of immunosuppression and reduced salivary flow, when the WBC count falls below 2000 cell/ml the immune system is less able to manage these infections
Opportunistic infections could be fungal (e.g. candidiasis), bacterial (E.g. gram negative bacterial infections) or viral (e.g. herpes simplex virus infections). These infections are managed by antifungal, antibacterial and antiviral agents, culture and sensitivity test is recommended
Bleeding: due to thrombocytopenia, when platelet count drops below 50.000/mm3, gingival bleeding and submucosal hemorrhage may occur, such patients are encouraged not to use tooth picks or dental floss. Management of bleeding is by local measures as applying pressure, using gelfoam and anti-fibrinolytic agents. Transfusion is recommended if local measures fail.
Sensitivity of the teeth: it can have an acute or delayed onset, due to hypo-salivation , it is managed by topical fluoride application.
Diminished sense of taste: as a result of damage to the microvilli of the taste cells, patients complain of a bitter or unpleasant taste, most of the patients will restore taste within 3-4 months after therapy. Zinc supplementation is reported to improve taste sensation.
Muscular dysfunction: it is a late complication of radiotherapy, it results from fibrosis and vascular damage of the muscles of mastication. Mouth opening should be maintained through physiotherapy.
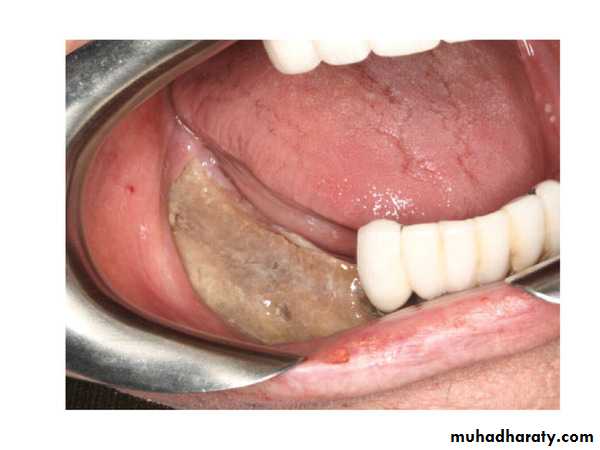
Osteoradionecrosis (ORN); it is a late complication that arise after radiotherapy, it is a state of hypocellularity, hypovascularity and hypoxia of the irradiated jaw bones, characterized by exposed bone that fails to heal. Factors that may increase the incidence of ORN:
1. Dentate patient.
2. Mandible, especially posterior region.
3. Dose of radiation, the risk of ORN is greater when the dose exceeds 6500 cGy.
4. Patients who continue smoking.
5. Trauma (like extraction).
6. Infection.
Prevention of ORN
1. Maintain good oral hygiene.2. Eliminate smoking.
3. Extraction of teeth should be done at least 2 weeks before radiotherapy.
4. Avoid extraction during or after radiotherapy if possible.
• 5. Minimize infection, use prophylactic antibiotics during extraction.
• 6. Minimize hypo-vascularity after radiotherapy through using non- Lidocain LA (e.g. Prilocain), minimize or avoid vasoconstrictors in LA, consider hyperbaric Oxygen.
• 7. Minimize trauma through atraumatic procedure, avoid periosteal elevation is possible, eliminate bony edges or spicules, irrigation and obtaining primary closure.
If ORN occurs, its management is:
1. Daily irrigation of the exposed bone by normal saline, antiseptic or antibiotic solutions.
2. Conservative local surgical debridement (trimming of the sharp edges of the sequestra) to avoid further trauma.
3. Broad spectrum antibiotics.
4. Severe cases may require hyperbaric Oxygen.
Bisphosphonate-associated Osteonecrosis (BON):
Bisphosphonates are used in treatment of osteoporosis, Paget's disease of bone and hypercalcemia of malignancy. They reduce skeletal events, associated with Multiple Myloma and metastatic solid tumors like breast, lung and prostate Cancer, in the bone.They inhibit osteoclastic activity and have antiangiogenic properties.
Factors that lead to BON
1. Bone metabolism.2. Local trauma (e.g. extraction).
3. Increased demand for bone repair.
4. Infection.
5. Hypovascularity.
The initial complaint is sudden presence of intraoral discomfort and roughness with traumatization of the soft tissues surrounding the area of necrotic bone.
Prevention of BON
1. Maintain good oral hygiene.
2. Eradication of infection by periodontal reatment and elimination of dental caries.
3. All un-restorable teeth should be extracted.
4. All procedures should be as atraumatic as possible.
Management of BON if it occurs
1. Medical consultation should be obtained.2. Local surgical debridement, only sharp edges of exposed bone should be removed.
3. Local irrigation.
4. Broad spectrum antibiotics.
5. Hyperbaric oxygen may be considered.
Carotid Atheroma: it develops in patients who have received irradiation more than 45 Gy. It represents a risk factor for stroke, it requires evaluation by a specialist.
Post treatment management
• 1. Consultation with the physician is recommended to determine if 2the patient is cured, in remission or in palliative car teri• 2. The patient should be on regular follow up to detect any additional lesions, latent metastases, recurrence and complications related to therapy and their management.
• 3. The patients should be instructed to continue oral hygiene measures.
• 4. Preventive oral care and dental procedures are provided.