REGIONAL SURVEY OF NERVE INJURIES
OBSTETRICAL BRACHIAL PLEXUSPALSYObstetrical palsy is caused by excessive traction on the
brachial plexus during childbirth, e.g. by pulling the
bay’s head away from the shoulder or by exerting traction
with the baby’s arm in abduction. Three patterns
are seen: (1) upper root injury (Erb’s palsy), typically in
overweight babies with shoulder dystocia at delivery;
(2) lower root injury (Klumpke’s palsy), usually after
breech delivery of smaller babies; and (3) total plexus
injury.
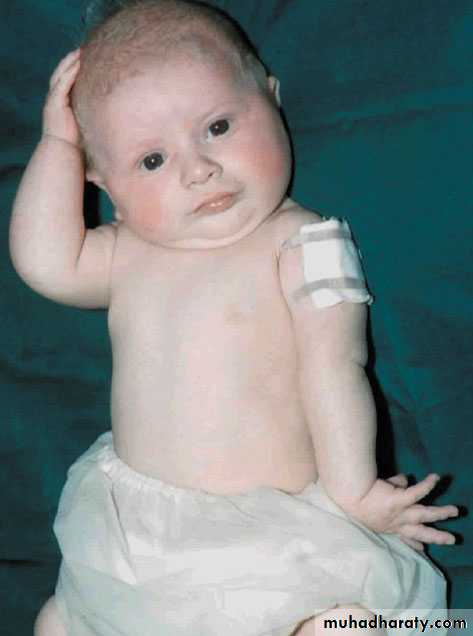
Clinical features
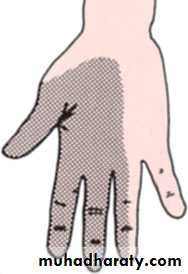
The diagnosis is usually obvious at birth: after a difficult delivery the baby has a floppy or flail arm. Further examination a day or two later will define the type of brachial plexus injury.Erb’s palsy is caused by injury of C5, C6 and (sometimes) C7.
The abductors and external rotators of the shoulder and the supinators are paralysed. The arm is held to the side, internally rotated and pronated.
There may also be loss of finger extension. Sensation cannot be tested in a baby.
Klumpke’s palsy is due to injury of C8 and T1. The baby lies with the arm supinated and the elbow flexed; there is loss of intrinsic muscle power in the hand.Reflexes are absent and there may be a unilateral Horner’s syndrome.
With a total plexus injury the baby’s arm is flail and pale; all finger muscles are parlysed and there may also be vasomotor impairment and a unilateral Horner’s syndrome.
X-rays should be obtained to exclude fractures of
the shoulder or clavicle (which are not uncommon
and which can be mistaken for obstetrical palsy.
ERB’S PALSY
Management
Over the next few weeks one of several things may happen.Paralysis may recover completely Many (perhaps most)
of the upper root lesions recover spontaneously. A
fairly reliable indicator is return of biceps activity by
the third month. However, absence of biceps activity
does not completely rule out later recovery.
Paralysis may improve A total lesion may partially
resolve, leaving the infant with a partial paralysis.
Paralysis may remain unaltered This is more likely with
complete lesions, especially in the presence of a
Horner’s syndrome. While waiting for recovery, physiotherapy is applied to keep the joints mobile.
OPERATIVE TREATMENT
If there is no biceps recovery by 3 months, operative intervention should be considered. Unless the roots are avulsed, it may be possible to excise the scar and bridge the gap with free sural nerve grafts; if the roots are avulsed, nerve transfer may give a worthwhile result.
The shoulder is prone to fixed internal rotation and adduction deformity. If diligent physiotherapy does not prevent this, then a subscapularis release will be needed, sometimes supplemented by a tendon transfer. In older children, the deformity can be treated by rotation osteotomy of the humerus.
RADIAL NERVE INJURY
The radial nerve may be injured at the elbow, in the upper arm or in the axilla.Clinical features
Low lesions are usually due to fractures or dislocations
at the elbow, or to a local wound. Iatrogenic lesions
of the posterior interosseous nerve where it winds
through the supinator muscle are sometimes seen
after operations on the proximal end of the radius
The patient complains of clumsiness and, on testing, cannot extend the metacarpophalangeal joints of the hand. In the thumb there is also weakness of extension
and retroposition. Wrist extension is preserved because the branch to the extensor carpi radialis longus arises proximal to the elbow.
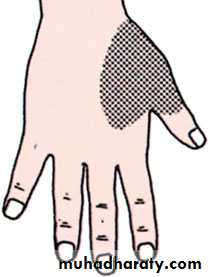
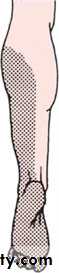
High lesions occur with fractures of the humerus or after prolonged tourniquet pressure.There is an obvious wrist drop, due to weakness of the radial extensors of the wrist, as well as inability to extend the metacarpophalangeal joints or elevate the thumb. Sensory loss is limited to a small patch on the dorsum around the anatomical snuffbox.
Very high lesions may be caused by trauma or operations around the shoulder. More often, though, they are due to chronic compression in the axilla; this is seen in drink and drug addicts who fall into a stupor with the arm dangling over the back of a chair (‘Saturday night palsy’) or in thin elderly patients using crutches (‘crutch palsy’). In addition to weakness of the wrist and hand, the triceps is paralysed and the triceps
reflex is absent.
Treatment
Open injuries should be explored and the nerverepaired or grafted as soon as possible.
Closed injuries are usually first or second degree
lesions, and function eventually returns. In patients
with fractures of the humerus it is important to examine
for a radial nerve injury on admission, before
treatment and again after manipulation or internal fixation.
If the palsy is present on admission, one can
afford to wait for 12 weeks to see if it starts to recover.
If it does not, then EMG should be performed; if this
shows denervation potentials and no active potentials
then a neurapraxia is excluded and the nerve should
be explored. The results, even with delayed surgery
and quite long grafts, can be gratifying as the radial
nerve has a straightforward motor function.
While recovery is awaited, the small joints of the hand must be put through a full range of passive movements. If recovery does not occur, the disability can be largely overcome by tendon transfers: pronator teres to the short radial extensor of the wrist, flexor carpi
radialis to the long finger extensors and palmaris longus to the long thumb abductor.
ULNAR NERVE
Injuries of the ulnar nerve are usually either near the wrist or near the elbow, although open wounds may damage it at any level.Clinical features
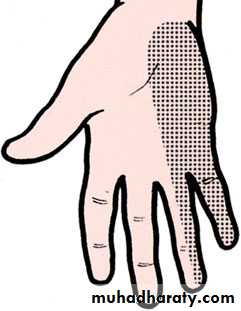
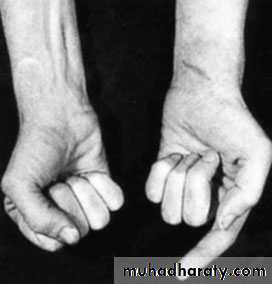
Low lesions are often caused by cuts on shattered glass.There is numbness of the ulnar one and a half fingers The hand assumes a typical posture in repose – the claw hand deformity – with hyperextension of the metacarpophalangeal joints of the ring and little fingers, due to weakness of the intrinsic muscles Hypothenar and interosseous wasting may be obvious by comparison with the normal hand.
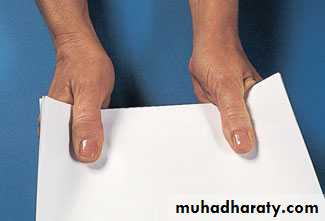
Finger abduction is weak and this, together with the loss of thumb adduction, makes pinch difficult The patient is asked to grip a sheet of paper forcefully between thumbs and index fingers while the examiner tries to pull it away; powerful flexion of the thumb interphalangeal
joint signals weakness of adductor pollicis and first dorsal interosseous with overcompensation by theflexor pollicis longus (Froment’s sign)
High lesions occur with elbow fractures or dislocations. The hand is not markedly deformed because the ulnar half of flexor digitorum profundus is paralysed and the fingers are therefore less ‘clawed’ (the ‘high
ulnar paradox’)
Treatment
Exploration and suture of a divided nerve are wellworthwhile, and anterior transposition at the elbow
permits closure of gaps up to 5 cm. While recovery is awaited, the skin should be protected from burns.
Hand physiotherapy keeps the hand supple and
Useful. If there is no recovery after nerve division, hand function is significantly impaired. Grip strength is diminished.and the second treatment by tendon transfer.
MEDIAN NERVE
The median nerve is most commonly injured near the wrist or high up in the forearm.
Clinical features
Low lesions may be caused by cuts in front of the wrist or by carpal dislocations. The patient is unable to abduct the thumb, and sensation is lost over the radial three and a half digits. In longstanding cases the thenar eminence is wasted and trophic changes may be seen.
High lesions are generally due to forearm fractures or elbow dislocation, but stabs and gunshot wounds may damage the nerve at any level. The signs are the same as those of low lesions but, in addition, the long flexors to the thumb, index and middle fingers. Typically the hand is held with the ulnar fingers flexed and the index straight (the ‘pointing sign’).
Treatment
If the nerve is divided, suture or nerve grafting should always be attempted. Postoperatively the wrist is splinted in flexion to avoid tension; when movements are commenced, wrist extension should be prevented.Late lesions are sometimes seen. If there has been no recovery, the disability is severe because of sensory loss and deficient opposition,the treaatment option is by tendon transfer.
SCIATIC NERVE
Division of the main sciatic nerve is rare except ingunshot wounds. Traction lesions may occur with
traumatic hip dislocations and with pelvic fractures.
Intraneural haemorrhage in patients receiving anticoagulants
is a rare cause of intense pain and partial loss of function.
Iatropathic lesions are sometimes discovered after
Total hip replacement – due either to inadvertent division, compression by bone levers or possibly thermal injury from extruded acrylic cement.
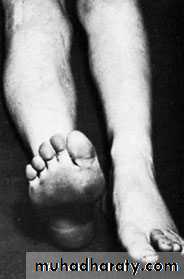
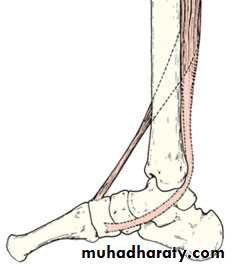
Clinical features
In a complete lesion the hamstrings and all muscles below the knee are paralysed; the ankle jerk is absent. Sensation is lost below the knee, except on the medialside of the leg which is supplied by the saphenous branch of the femoral nerve. The patient walks with a
drop foot and a high-stepping gait to avoid dragging the insensitive foot on the groundIn late cases the limb is wasted, with fixed deformities
of the foot and trophic ulcers on the sole.
Treatment
If the nerve is known to be divided, suture or nerve grafting should be attempted even though it may take more than a year for leg muscles to be re-innervated.While recovery is awaited, a below-knee drop-foot splint is fitted. The chances of recovery are generally poor, Partial lesions, in which there is protective sensation of the sole, can sometimes be managed by transferring tibialis posterior to the front in order to counteract the drop foot. If there is no recovery
whatever, amputation may be preferable to a flail,
deformed, insensitive limb.