Cardiac Lectures Dr. Ahmed Moyed Hussein
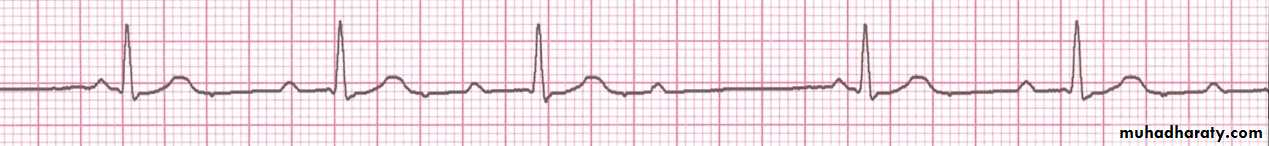
Atrioventricular block:First-degree atrioventricular block:
In this condition, AV conduction is delayed and so the PR interval is prolonged (> 0.20 s). It rarely causes symptoms.
Fig: first degree heart block, showing prolonged PR interval(0.38 s)
First degree AV block can be due to: inferior MI, digitalis toxicity, hyperkalemia, increased vagal tone, acute rheumatic fever or myocarditis.Second-degree atrioventricular block:
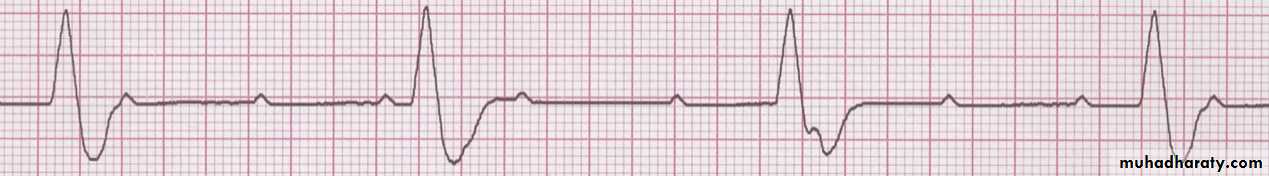
In this, dropped beats occur because some impulses from the atria fail to conduct to the ventricles. In Mobitz type I second-degree AV block there is progressive lengthening of successive PR intervals, culminating in a dropped beat. The cycle then repeats itself. This is known as the Wenckebach phenomenon and is usually due to impaired conduction in the AV node itself. The phenomenon may be physiologicaland is sometimes observed at rest or during sleep in athletic young adults with high vagal tone.
In Mobitz type II second-degree AV block the PR interval of the conducted impulses remains constant but some P waves are not conducted. This is usually caused by disease of the His–Purkinje system
and carries a risk of asystole.
Fig: 2nd degree Mobits type I heart block, show progressive prolongation of PR interval followed by nonconducted P wave (circle).
Fig: 2nd degree Mobits type II heart block with 3: 1 conduction
Third-degree (complete) atrioventricular block:When atrioventricular (AV) conduction fails completely, the atria and ventricles beat independently (AV dissociation). Ventricular activity is maintained by an escape rhythm arising in the AV node or bundle of His (narrow QRS complexes) or the distal Purkinje tissues (broad QRS complexes). Complete AV block produces a slow (25–50/min), regular pulse. Cannon waves may be visible in the neck during JVP examination and the intensity of the first heart sound varies due to the loss of AV synchrony.
Fig: complete heart block, show AV dissociation
Management:Patients with symptomatic bradyarrhythmias associated with AV block should receive a permanent pacemaker. Asymptomatic first-degree or Mobitz type I second-degree AV block (Wenckebach phenomenon) does not require treatment.
Temporary pacemakers:
Temporary pacing involves delivery of an electrical impulse into the heart to initiate tissue depolarization and to trigger cardiac contraction. This is achieved by inserting a bipolar pacing electrode via the internal jugular, subclavian or femoral vein and positioning it at the apex of the Right Ventricle, using fluoroscopic imaging. The electrode is connected to an external pacemaker with an adjustable energy output and pacing rate. The ECG of right ventricular pacing is characterized by regular broad QRS complexes with a left bundle branch block pattern. Each complex is immediately preceded by a ‘pacing spike’.
Temporary pacing may be indicated in the management of transient AV block and other arrhythmias complicating acute MI or cardiac surgery, to maintain the rhythm in other situations of reversible bradycardia (i.e. due to metabolic disturbance or drug overdose), or as a bridge to permanent pacing. temporary pacing system should ideally not be used for more than 7 days.
Transcutaneous pacing is administered by delivering an electrical stimulus through two large adhesive gel pad electrodes placed over the apex and upper right sternal edge, or over the anterior and posterior chest. It is easy and quick to set up, but causes discomfort because it induces forceful pectoral and intercostal muscle contraction.
Permanent pacemakers:
Permanent pacemakers are small, flat, metal devices that are implanted under the skin, usually in the pectoral area. Pacing electrodes (leads) can be placed via the subclavian or cephalic veins into the right ventricle (usually at the apex).A permanent pacemaker is usually indicated in patients with asymptomatic Mobitz type II second- or third-degree AV heart block because of the risk of asystole and sudden death. Pacing improves prognosis.
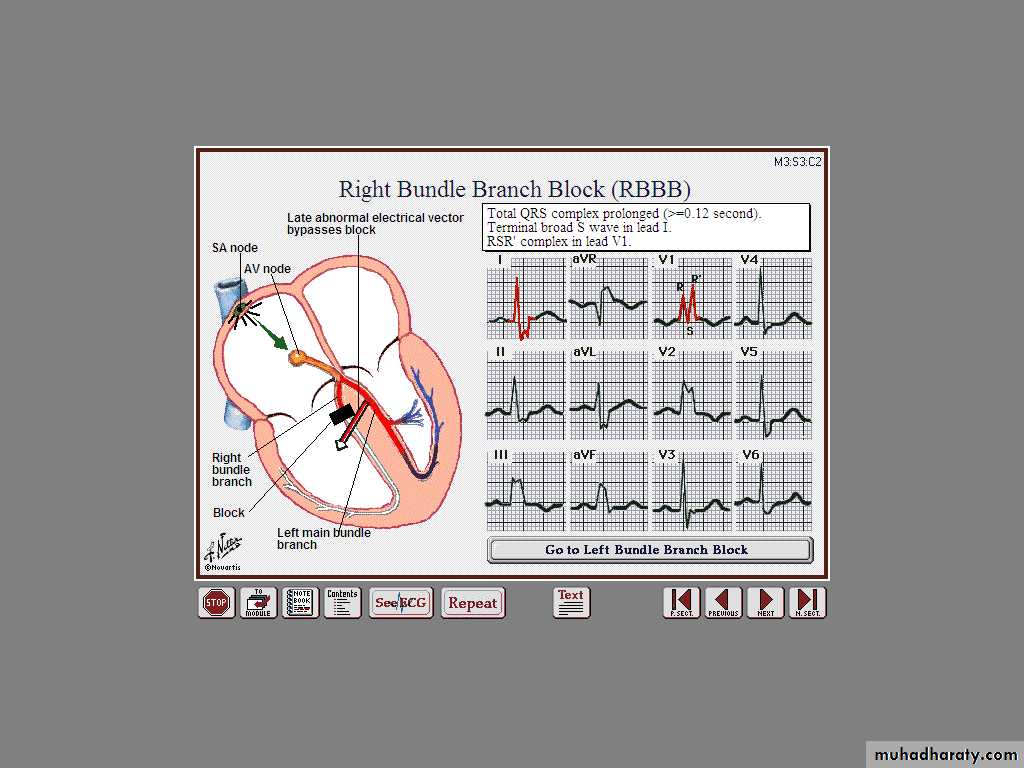
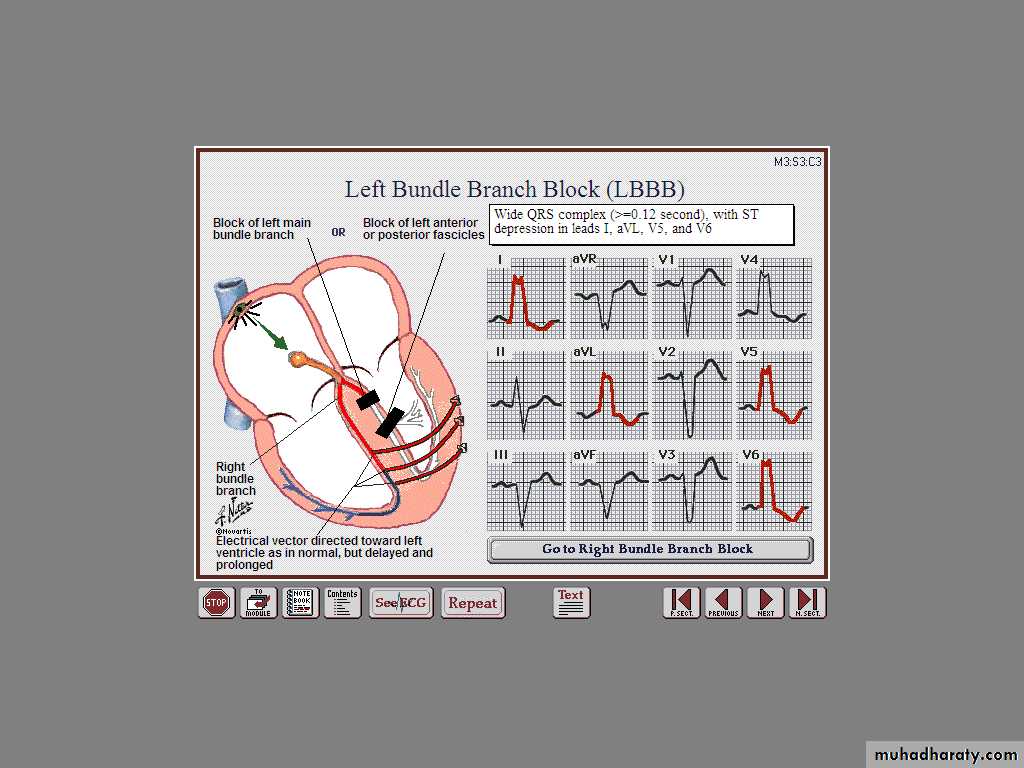
Bundle branch block and hemiblock:
Conduction block in the right or left bundle branch can occur as a result of many pathologies, including ischaemic or hypertensive heart disease or cardiomyopathies. Depolarisation proceeds through a slow myocardial route in the affected ventricle rather than through the rapidly conducting Purkinje tissues that constitute the bundle branches. This causes delayed conduction into the LV or RV, broadens the QRS complex (≥ 0.12 s) and produces the characteristic alterations in QRS morphology. Right bundle branch block (RBBB) can occur in healthy people but left bundle branch block (LBBB) often signifies important underlying heart disease.
The left bundle branch divides into an anterior and a posterior fascicle. Damage to the conducting tissue at this point (hemiblock) does not broaden the QRS complex but alters the mean direction of ventricular
depolarisation (mean QRS axis). The combination of right bundle branch block and left anterior or posterior hemiblock is known as bifascicular
block.