
Thyroid eye disease
Introduction
Thyrotoxicosis
Thyrotoxicosis (hyperthyroidism) is a condition involving excessive secretion of
thyroid hormones. Graves disease, the most common subtype of hyperthyroidism.
1 Presentation is in the 3–4th decades with weight loss despite good appetite,
increased bowel frequency, sweating, heat intolerance, nervousness, irritability,
palpitations, weakness and fatigue.
2 Signs
a External
• Diffuse thyroid enlargement fine hand tremor, palmar erythema, and
warm and sweaty skin.
• Finger clubbing (thyroid acropachy ).
• Pretibial myxoedema .
• Alopecia and vitiligo .
• .
b Cardiovascular
• Sinus tachycardia, atrial fibrillation and premature ventricular beats.
• High output heart failure.
3 Investigations. Thyroid function tests include serum T3, T4, TSH, thyroxine
binding globulin (TBG) and thyroid-stimulating immunoglobulin (TSI).
4 Treatment options include carbimazole, propylthiouracil, propranolol,
radioactive iodine and partial thyroidectomy.
Risk factors for ophthalmopathy
*The major clinical risk factor for developing thyroid eye disease (TED) is
smoking. The greater the number of cigarettes smoked per day, the greater the
risk, and giving up smoking seems to reduce the risk.
*Women are five times more likely to be affected by TED than men, but this
largely reflects the increased incidence of Graves disease in women.
*Radioactive iodine used to treat hyperthyroidism can worsen TED.
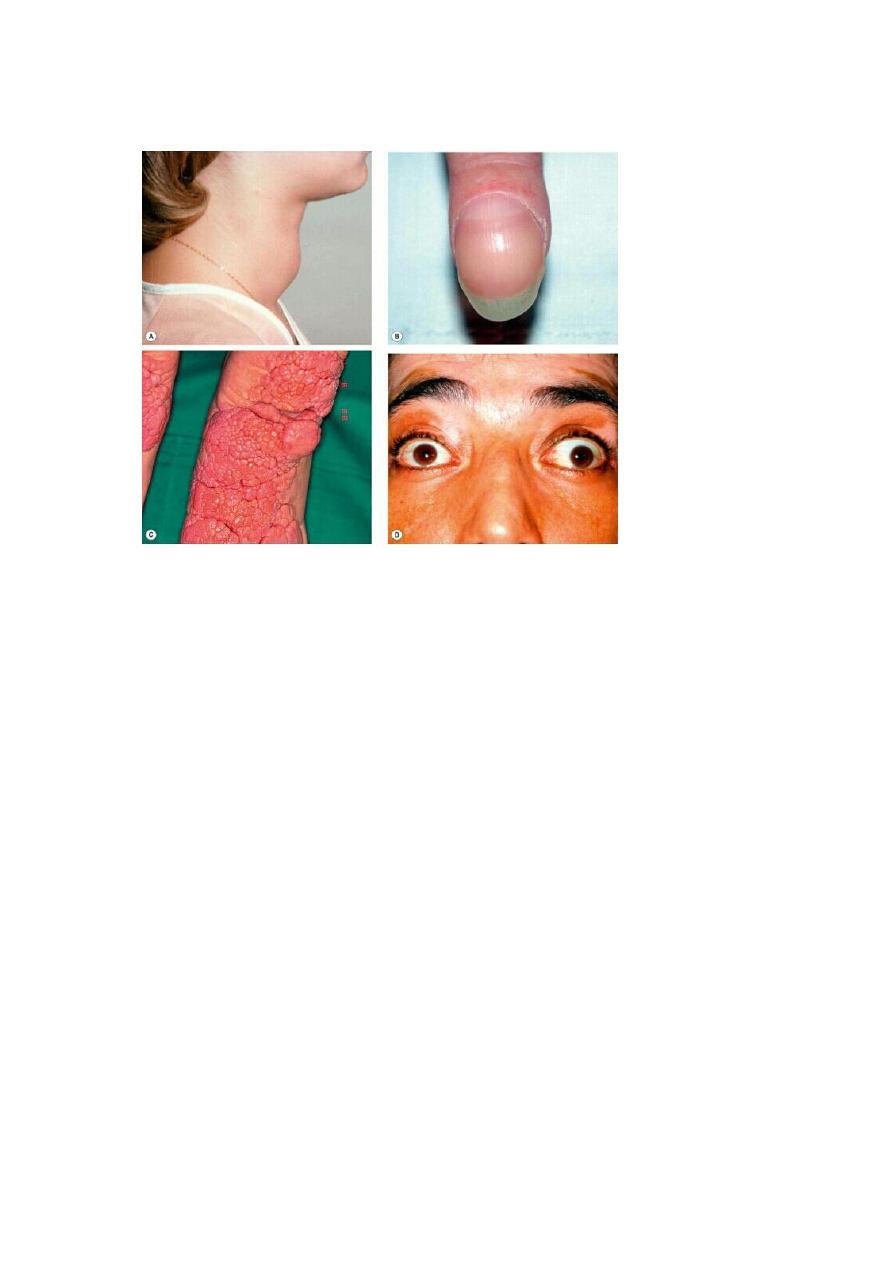
Systemic signs in thyrotoxicosis. (A) Goitre; (B) acropachy; (C) very severe pretibial
myxoedema; (D) vitiligo
Pathogenesis of ophthalmopathy
Thyroid ophthalmopathy involves an organ-specific autoimmune reaction in which a
humoral agent (IgG antibody) produces the following changes:
1
Inflammation of extraocular muscles characterized by pleomorphic cellular
infiltration , associated with increased secretion of glycosaminoglycans and osmotic
imbibition of water.
The muscles become enlarged, sometimes up to eight times their normal size, and
may compress the optic nerve.
2
Inflammatory cellular infiltration with lymphocytes, plasma cells, macrophages
and mast cells of interstitial tissues, orbital fat and lacrimal glands with
accumulation of glycosaminoglycans and retention of fluid.
Clinical manifestations
(a) soft tissue involvement
(b) lid retraction
(c) proptosis

(d) optic neuropathy
(e) restrictive myopathy.
Stages in the development of the disease:
1
Congestive (inflammatory) stage = the eyes are red and painful.
This tends to remit within 3 years
Only 10% of patients develop serious long-term ocular problems.
2
Fibrotic (quiescent) stage = the eyes are white
although a painless motility defect may be present.
A - Soft tissue involvement
1
Symptoms include grittiness, photophobia, lacrimation and retrobulbar
discomfort.
2
Signs
• Epibulbar hyperaemia is a sensitive sign of inflammatory activity.
Intense focal hyperaemia may outline the insertions of the horizontal
recti.
• Periorbital swelling is caused by oedema and infiltration behind the
orbital septum; this may be associated with chemosis and prolapse of
retroseptal fat into the eyelids.
• Superior limbic keratoconjunctivitis.
3
Treatment
a
Lubricants for superior limbic keratoconjunctivitis, corneal exposure and
dryness.
b
Topical anti-inflammatory agents (steroids, NSAIDs, ciclosporin).
c Head elevation with three pillows during sleep to reduce periorbital
oedema.
d
Eyelid taping during sleep may alleviate mild exposure keratopathy.
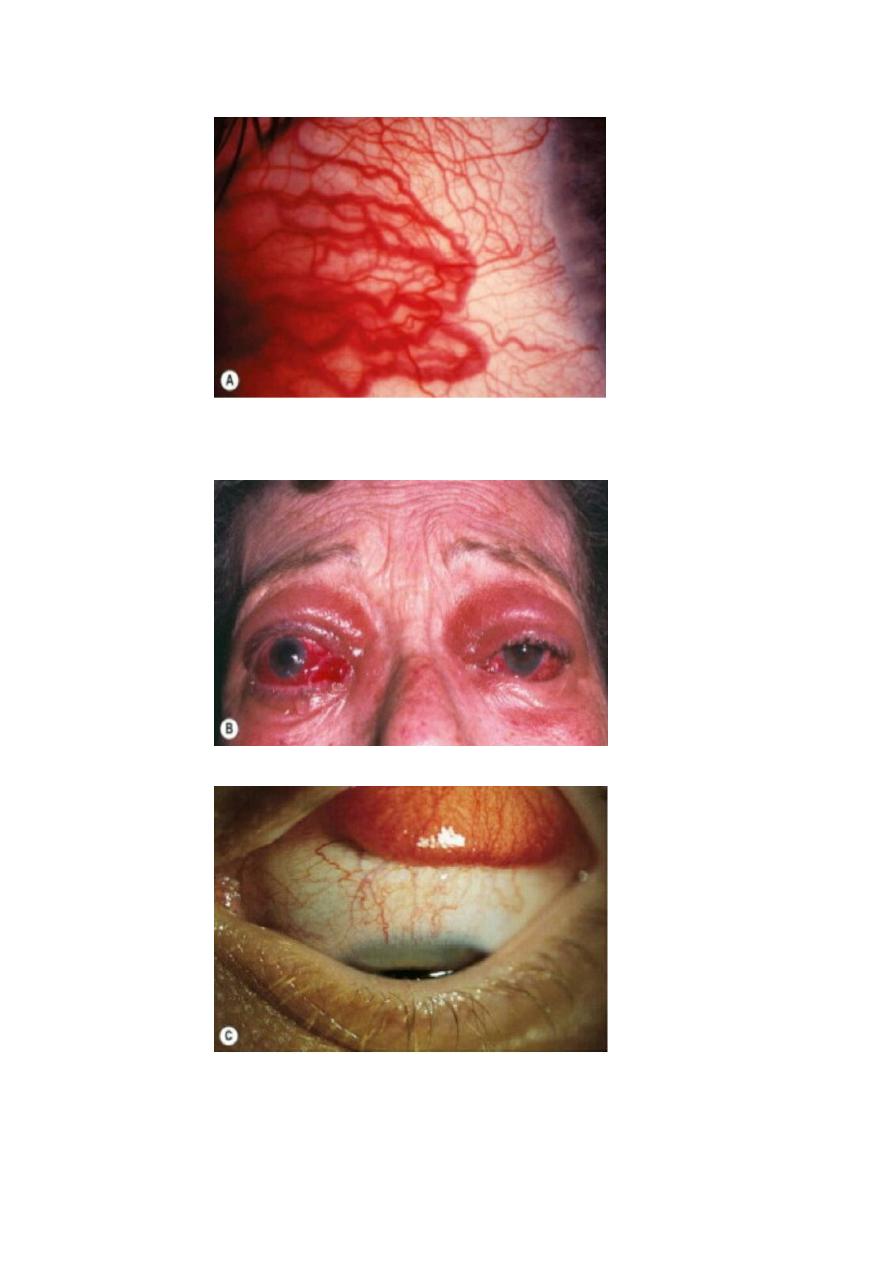
Epibulbar hyperaemia overlying a horizontal rectus muscle
periorbital oedema, chemosis ,prolapse of fat into the eyelids
superior limbic keratoconjunctivitis

Lid retraction
Pathogenesis
Retraction of upper and lower lids occurs in about 50% of patients with
Graves disease
Postulated mechanisms:
1 Fibrotic contracture of the levator associated with adhesions.
2 Secondary overaction of the levator-superior rectus complex in
response to hypotropia.
3 Humorally-induced overaction of Müller muscle as a result of
sympathetic overstimulation secondary to high levels of thyroid
hormones.
Signs
The upper lid margin normally rests 2 mm below the limbus
Lid retraction is suspected when the margin is either level with or above
the superior limbus, allowing sclera to be visible ('scleral show’
Likewise, the lower eyelid normally rests at the inferior limbus; retraction
is suspected when sclera shows below the limbus.
Lid retraction may occur in isolation or in association with proptosis
which exaggerates its severity.
1 Dalrymple sign is lid retraction in primary gaze .
2 Kocher sign describes a staring and frightened appearance of the
eyes which is particularly marked on attentive fixation .
3 Von Graefe sign signifies retarded descent of the upper lid on
downgaze .
Management
Mild lid retraction does not require treatment because it frequently
improves spontaneously.
Control of hyperthyroidism may also be beneficial.
Surgery to decrease the vertical dimensions of the palpebral fissures may
be considered in patients with significant but stable lid retraction, but
only after addressing proptosis and strabismus.
In general, therefore the sequence of surgical procedures in TED is: (a)
orbital, (b) strabismus and (c) eyelid.
The rationale for this sequence is that orbital decompression may affect
both ocular motility and eyelid position, and extraocular muscle surgery
may also influence eyelid position. The main surgical procedures for lid
retraction are:
1 Müllerotomy (disinsertion of Müller muscle) for mild lid retraction.
More severe cases may also require recession/disinsertion of the
levator aponeurosis and the suspensory ligament of the superior
conjunctival fornix.
2 Recession of the lower lid retractors, with or without a hard palate
graft, when retraction of the lower lid is 2 mm or more.
3 Botulinum toxin injection aimed at the levator aponeurosis and
Müller muscle may be used as a temporary measure in patients
awaiting definitive correction.
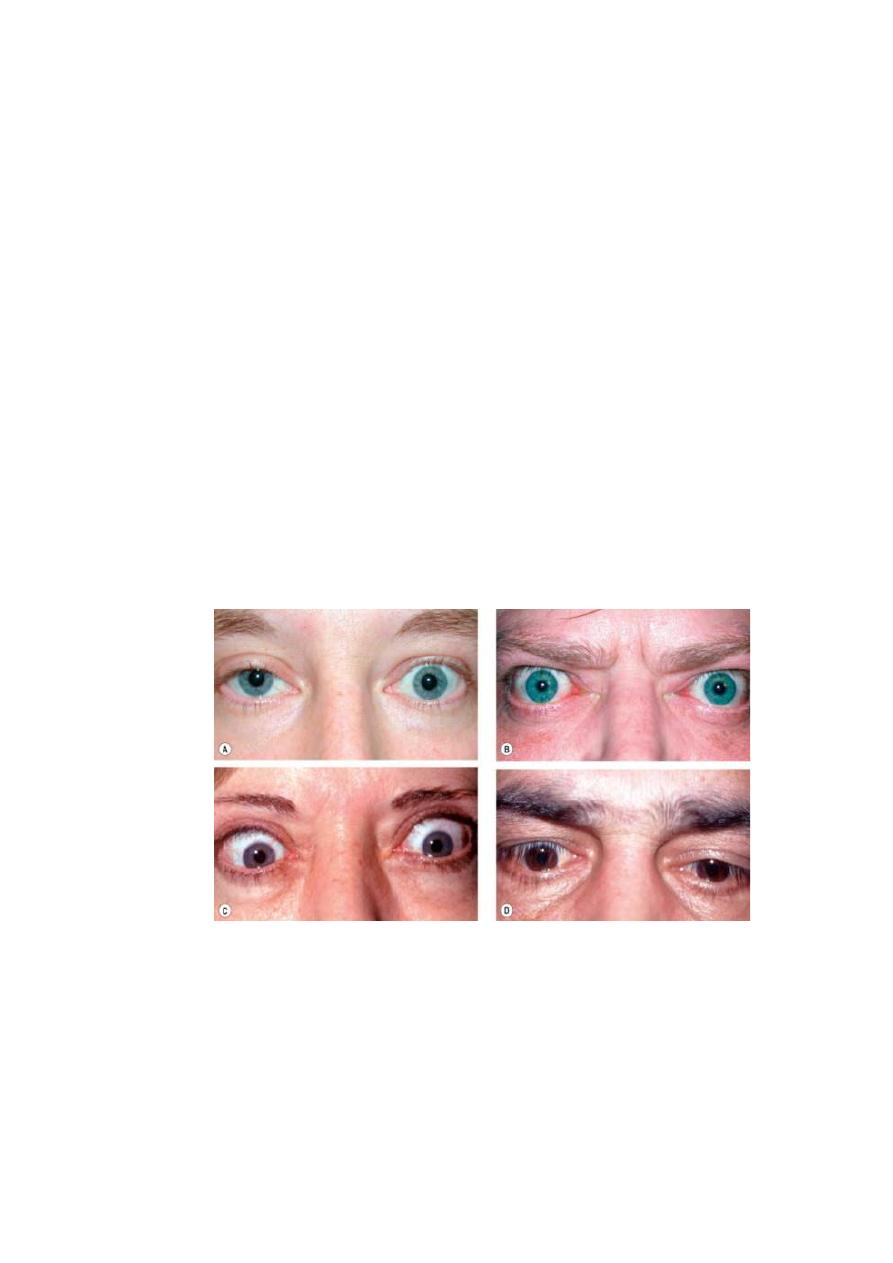
Fig. 3.8 Lid signs in thyroid eye disease. (A) Mild left lid retraction; (B)
moderate bilateral symmetrical lid retraction; (C) severe bilateral lid retraction;
(D) right lid lag on downgaze
Proptosis
is axial, unilateral or bilateral,
symmetrical or asymmetrical . frequently permanent.
Severe proptosis may compromise lid closure with resultant exposure
keratopathy, corneal ulceration and infection.
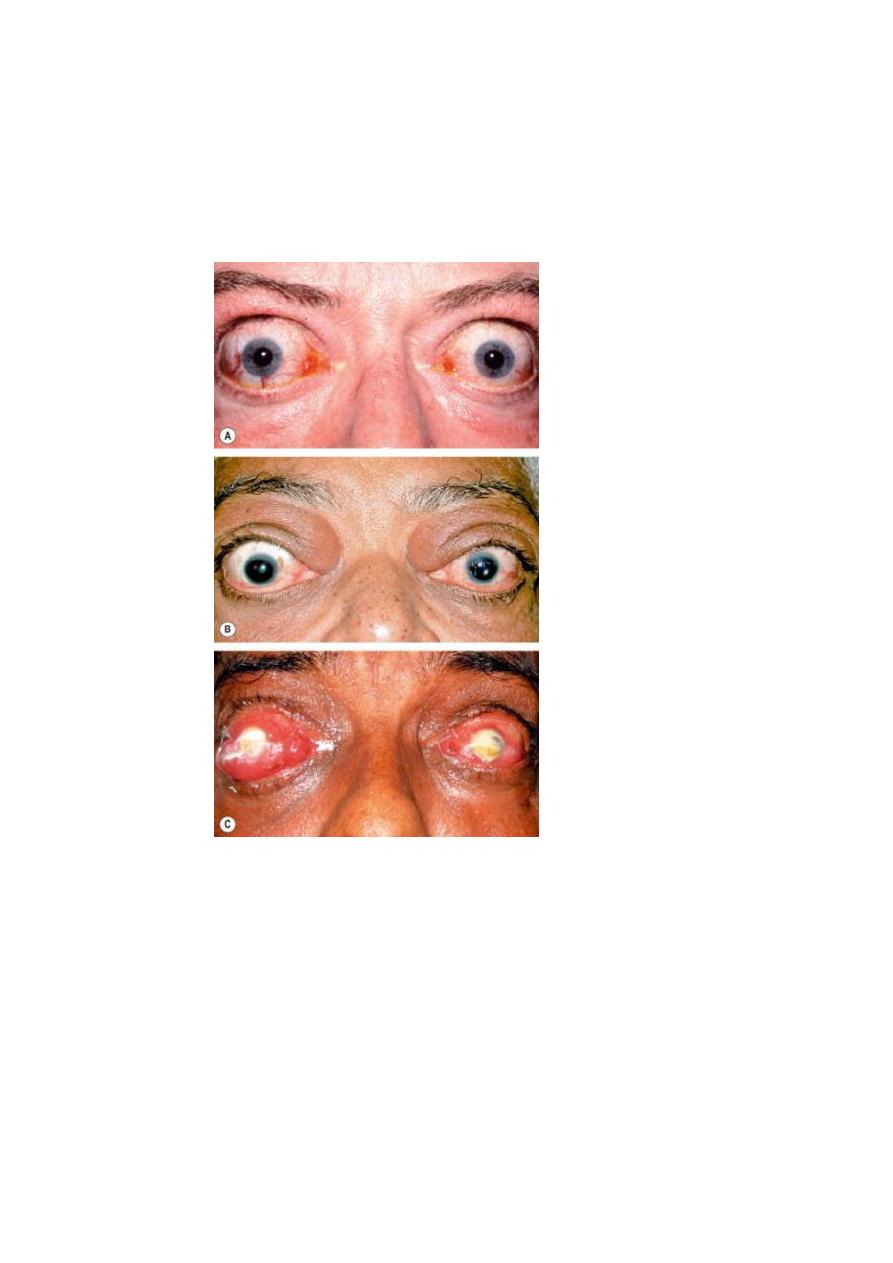
Proptosis in thyroid eye disease. (A) Symmetrical; (B) asymmetrical; (C)
bacterial keratitis due to exposure
Management
1 Systemic steroids may be used in rapidly progressive and painful
proptosis during the congestive phase, unless contraindicated (e.g.
tuberculosis or peptic ulceration).
a Oral prednisolone 60–80 mg/day is given initially. necessary.
b Intravenous methylprednisolone (e.g. 0.5 g in 200–500 mL
isotonic saline given over 30 minutes), mandate careful
supervision by a physician.
2 Radiotherapy may be used in addition to steroids or when steroids
are contraindicated or ineffective. A positive response is usually
evident within 6 weeks, with maximal improvement by 4 months.
3 Combined therapy with irradiation, azathioprine and low-dose
prednisolone may be more effective than steroids or radiotherapy
alone. Monoclonal antibody treatment with rituximab also shows
very good results.
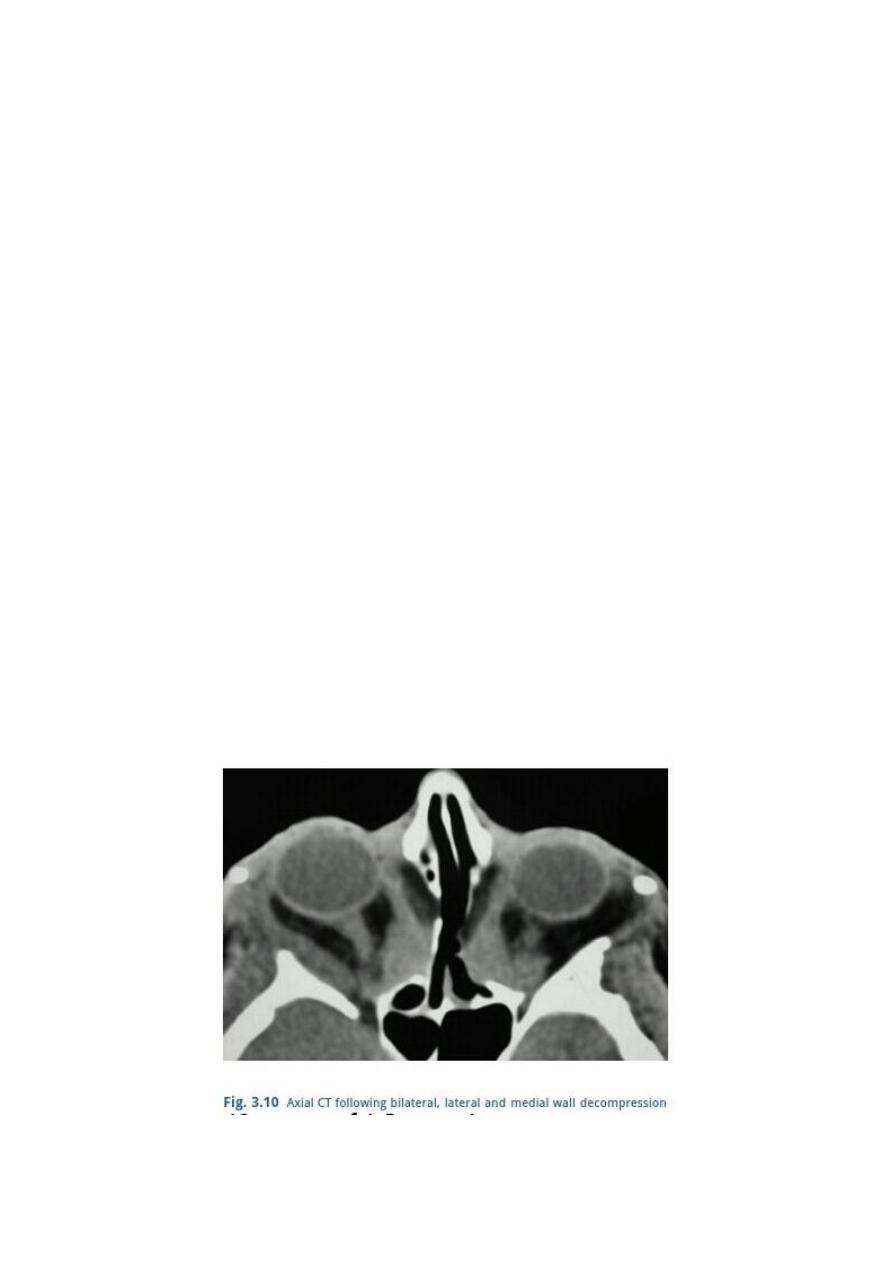
4 Surgical decompression may be considered either as the primary
treatment or when non-invasive methods are ineffective, such as for
cosmetically unacceptable proptosis in the quiescent phase.
Decompression aims to increase the volume of the orbit by removing
the bony walls and may be combined with removal of orbital fat to
increase the retroplacement of the globe.
• One-wall (deep lateral) decompression (approximately 4–5 mm
reduction in proptosis)
may reduce the risk of postoperative diplopia.
• Two-wall (balanced medial and lateral) decompression ,
significant risk of inducing diplopia.
• Three-wall decompression includes the floor
reduction in proptosis of 6–10 mm
may lead to hypoglobus
has a higher risk of infraorbital nerve damage and diplopia.
• Very severe proptosis may require additional removal of part of
the orbital roof (four-wall decompression).
• Most surgery is undertaken via an external approach
Sometimes surgery is done endoscopically.
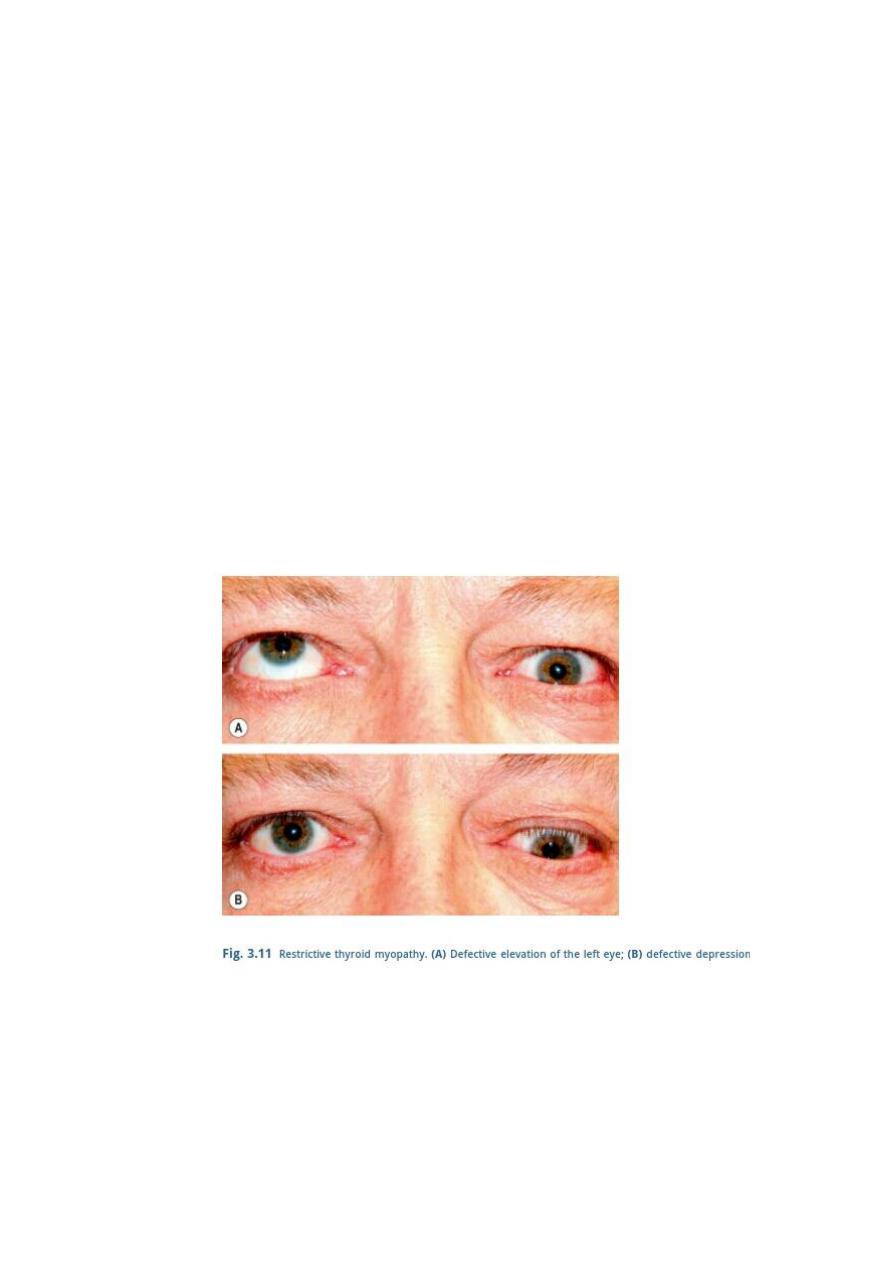
Restrictive myopathy
Diagnosis
Between 30% and 50% of patients with TED develop ophthalmoplegia
and this may be permanent.
Ocular motility is restricted initially by inflammatory oedema and later
by fibrosis.
Intraocular pressure may increase in upgaze due to ocular compression by
a fibrotic inferior rectus.
In order of frequency the four ocular motility defects are:
1 Elevation defect caused by fibrotic contracture of the inferior rectus,
which may mimic superior rectus palsy.
2 Abduction defect due to fibrosis of the medial rectus, which may
simulate 6th nerve palsy.
3 Depression defect secondary to fibrosis of the superior rectus.
4 Adduction defect caused by fibrosis of the lateral rectus.
Treatment
1 Surgery
a Indication is diplopia in the primary or reading positions of
gaze, provided the disease is quiescent and the angle of

deviation has been stable for at least 6 months.
Until these criteria are met diplopia may be alleviated, if
possible, with prisms.
b Goal is to achieve binocular single vision in the primary and
reading positions.
Restrictive myopathy, which causes incomitant strabismus,
often precludes binocularity in all positions of gaze. However,
with time the field of binocular single vision may enlarge as a
result of increasing vergences.
c Technique recession of the inferior and/or medial recti, using
adjustable sutures for best results.
The suture is adjusted later the same day or on the first
postoperative day to achieve optimal alignment, and the patient
is encouraged to practise achieving single vision with a distant
target such as a television.
It should be emphasized that a rectus muscle is never resected,
only recessed in TED.
2 Botulinum toxin injection into the involved muscle may be useful
in selected cases.
Optic neuropathy
Optic neuropathy is an uncommon but serious complication caused by
compression of the optic nerve or its blood supply at the orbital apex by
the congested and enlarged recti
Such compression, which may occur in the absence of significant
proptosis, may lead to severe but preventable visual impairment.
Diagnosis
1 Presentation is with impairment of central vision.
2 Signs
• Visual acuity is usually reduced, but not invariably, and is
associated with a relative afferent pupillary defect, colour
desaturation and diminished light brightness appreciation.
It is important not to attribute disproportionate visual loss to
minor corneal complications and miss optic neuropathy.
• Visual field defects may be central or paracentral and may be
combined with nerve fibre bundle defects.

These findings, combined with elevated intraocular pressure,
may be confused with primary open-angle glaucoma. (DDx)
• The optic disc is usually normal, occasionally swollen and
rarely atrophic.
Treatment
Initial treatment is usually with systemic steroids.
Orbital decompression may be considered if steroids are ineffective or
inappropriate.
CT shows muscle enlargement in thyroid eye disease. (A) Axial view; (B)
coronal view – note sparing of the right lateral rectus muscle; (C) coronal view
shows crowding at the orbital apex
Dr Yasser Ibraheem Abdullah C.A.B.Ophth F.I.C.O.

