
Lecture 16 by Dr.Alaa F.Alwan
Clinical blood transfusion
Blood donation shall in all circumstances be voluntary. Financial profit
must never be a motive for the donor or for those collecting the donation.
Measures to protect the donor.
1. Age 17–70 years (60 at first donation)
2. Weight above 50 kg
3. Haemoglobin >13 g/dL for men, 12 g/dL for women
4. Minimum donation interval of 12 weeks (16 weeks advised) and three
donations per year maximum
5.Pregnant and lactating women excluded because of high iron
requirements
Exclusion of those with:
1.Known cardiovascular disease, including hypertension
2.Significant respiratory disorders
3.Epilepsy and other CNS disorders
4.Gastrointestinal disorders with impaired absorption
5.Insulin-dependent diabetes
6.Chronic renal disease
7.Ongoing medical investigation or clinical trials
8.Exclusion of any donor returning to occupations such as driving bus,
plane or train, heavy machine or crane operator, mining, scaffolding, etc.
because delayed faint would be hazardous
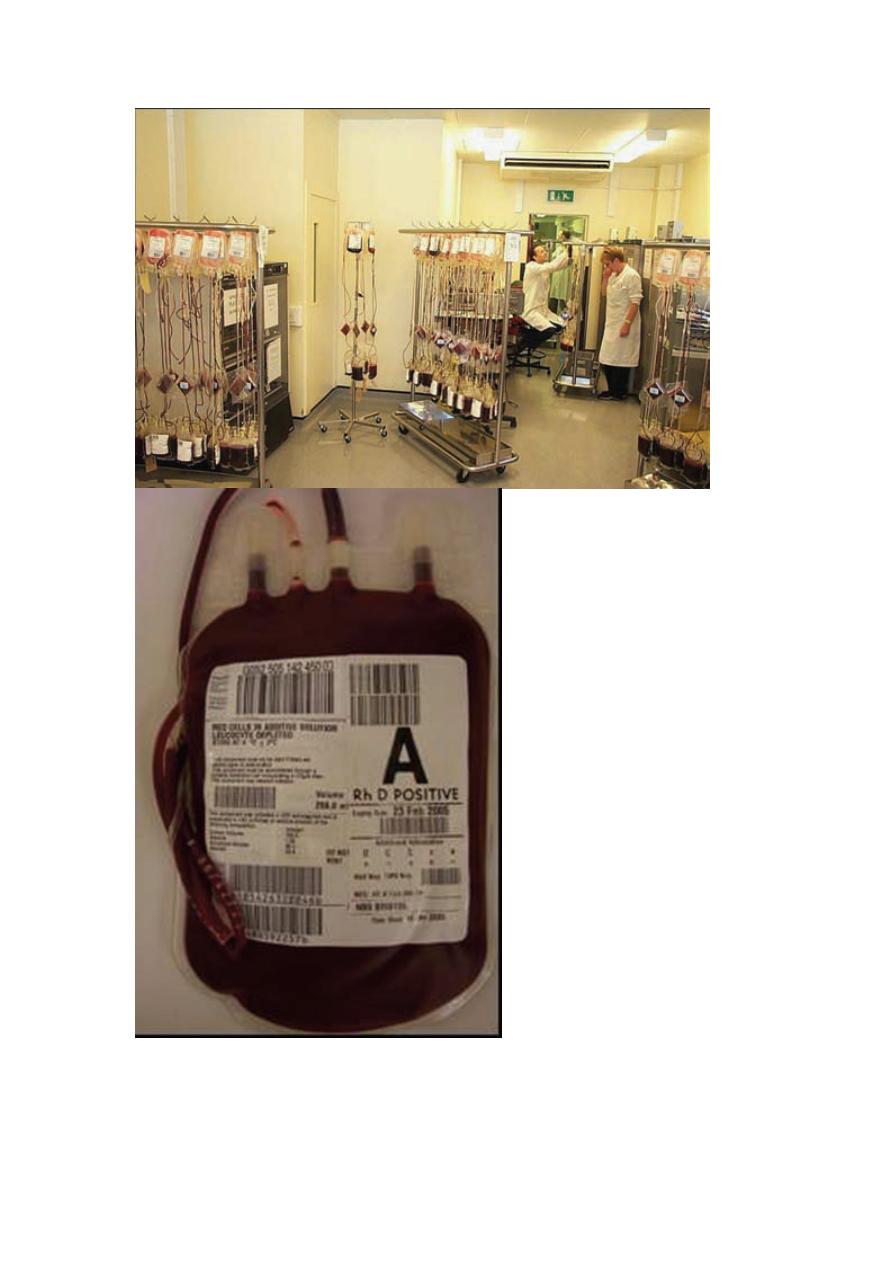
Volume of blood taken
Modern blood collection packs are designed to hold 450 mL of blood,
mixed with 63 mL of citrate–phosphate–dextrose–adenine (CPD-A)
anticoagulant
ABO system
The ABO system is a group of carbohydrate antigens in which the
individual alleles are defined by the terminal saccharide moiety.
Specifically, addition of N-acetylgalactosamine or galactose to the
subterminal galactose yields red cells of group A or group B,
respectively. Individuals who express neither of these sugars on the
subterminal galactose are group O, and individuals who express both
sugars are group AB.
Rh system
Clinically, the Rh blood group system is almost as important as the ABO
system. Unlike the ABO system, which comprises carbohydrate antigens,
Rh antigens are proteins. Also unlike the ABO system, antibodies to Rh
antigens are rarely present unless a person has been previously
immunized by transfusion or pregnancy, or has undergone an allogeneic
hematopoietic stem cell transplantation (HSCT) utilizing an Rh-
alloimmunized donor or an Rh-mismatched donor.
Other protein antigen systems
Outside the ABO and Rh systems, most clinically significant blood group
alloantibodies are directed against protein based antigens, particularly
antigens in the Kell, Kidd, Duffy, and MNSs systems. As is the case with
the Rh system, and unlike the ABO system, these systems are defined by
protein (as opposed to carbohydrate) antigenic determinants.
Blood product: Any therapeutic substance prepared from human blood
WHOLE BLOOD (CPD-Adenine-1):A 450 ml whole blood donation
contains: Up to 510 ml total volume (volume may vary in accordance
with local policies), 450 ml donor blood, 63 ml anticoagulant-
preservative solution, Haemoglobin approximately 12 g/ml, Haematocrit
35%–45%, No functional platelets, No labile coagulation factors (V and
VIII)
Infection risk: Not sterilized, so capable of transmitting any agent present
in cells or plasma which has not been detected by routine screening for
transfusion-transmissible infections, including HIV-1 and HIV-2,
hepatitis B and C, other hepatitis viruses, syphilis, malaria and Chagas
disease
Storage: Between +2C and +6C in approved blood bank refrigerator,
fitted with a temperature chart and alarm. Transfusion should be started
within 30 minutes of removal from refrigerator
Indications: Red cell replacement in acute blood loss with hypovolemia,
Exchange transfusion, Patients needing red cell transfusions where red
cell concentrates or suspensions are not available
Contraindications: Risk of volume overload in patients with: Chronic
anemia, incipient cardiac failure
Administration: Must be ABO and RhD compatible with the recipient,
never add medication to a unit of blood, Complete transfusion within 4
hours of commencement
RED CELL CONCENTRATE (‘Packed red cells’, ‘plasma-reduced
blood’
Description: 150–200 ml red cells from which most of the plasma has
been removed, Hemoglobin approximately 20 g/100 ml (not less than 45
g per unit), Hematocrit 55%–75%
Infection risk: Same as whole blood
Storage: Same as whole blood

Indications: Replacement of red cells in anemic patients, Use with
crystalloid replacement fluids or colloid solution in acute blood loss
Administration: Same as whole blood
LEUCOCYTE-DEPLETED RED CELLS
Description: A red cell suspension or concentrate containing <5 x 106
white cells per pack, prepared by filtration through a leucocyte-depleting
filter. Hemoglobin concentration and hematocrit depend on whether the
product is whole blood, red cell concentrate or red cell suspension
Leucocyte depletion significantly reduces the risk of transmission of
cytomegalovirus (CMV)
Infection risk: Same as whole blood for all other transfusion transmissible
infections
Storage: Depends on production method
Indications: Minimizes white cell immunization in patients receiving
repeated transfusions but, to achieve this, all blood components given to
the patient must be leucocyte-depleted. Reduces risk of CMV
transmission in special situations. Patients who have experienced two or
more previous febrile reactions to red cell transfusion
It will not prevent graft-vs-host disease so for this purpose, blood
components should be irradiated where facilities are available (radiation
dose: 25–30 Gy)
Administration: Same as whole blood
Alternative: Buffy coat-removed whole blood or red cell suspension is
usually effective in avoiding febrile non-hemolytic transfusion reactions
The blood bank should express the buffy coat in a sterile environment
immediately before transporting the blood to the bedside
Start the transfusion within 30 minutes of delivery and use a leucocyte
filter, where possible. Complete transfusion within 4 hours of
commencement

PLATELET CONCENTRATES (prepared from whole blood donations)
Description: Single donor unit in a volume of 50–60 ml of plasma should
contain: At least 55 x 109 platelets, <1.2 x 109 red cells, <0.12 x 109
leucocytes
Pooled unit: platelets prepared from 4 to 6 donor units ‘pooled’ into one
pack to contain an adult dose of at least 240 x 109 platelets
Infection risk: Same as whole blood, but a normal adult dose involves
between 4 and 6 donor exposures
Storage: Up to 72 hours at 20 C to 24 C (with agitation) unless collected
in specialized platelet packs validated for longer
Indications: Treatment of bleeding due to Thrombocytopenia, Platelet
function defects, Prevention of bleeding due to thrombocytopenia, such
as in bone marrow failure
Contraindications: Not generally indicated for prophylaxis of bleeding in
surgical patients, unless known to have significant pre-operative platelet
deficiency
Not indicated in: Thrombotic thrombocytopenic purpura (TTP)
Dosage: 1 unit of platelet concentrate/10 kg body weight: in a 60 or 70 kg
adult, 4–6 single donor units containing at least 240 x 109 platelets
should raise the platelet count by 20–40 x 109/L
Increment will be less if there is: Splenomegaly, Disseminated
intravascular coagulation, Septicemia
Administration: After pooling, platelet concentrates should be infused as
soon as possible, generally within 4 hours, because of the risk of bacterial
proliferation
Must not be refrigerated before infusion as this reduces platelet function
Should be infused over a period of about 30 minutes
Do not give platelet concentrates prepared from RhD positive donors to
an RhD negative female with childbearing potential
Give platelet concentrates that are ABO compatible, whenever possible
Complications: Febrile non-hemolytic and allergic urticarial reactions are
not uncommon, especially in patients receiving multiple transfusions

PLATELET CONCENTRATES (collected by plateletpheresis)
Description: Volume 150–300 ml, Platelet content 150–500 x 109,
equivalent to 3–10 single donations
Infection risk: Same as whole blood
Storage: Up to 72 hours at 20C to 24C (with agitation) unless collected in
specialized platelet packs validated for longer storage periods; do not
store at 2C to 6 C
Indications: Same above
FRESH FROZEN PLASMA
Description: Pack containing the plasma separated from one whole blood
donation within 6 hours of collection and then rapidly frozen to –25C or
colder
Contains normal plasma levels of stable clotting factors, albumin and
immunoglobulin
Usual volume of pack is 200–300 ml

Storage : At –25C or colder for up to 1 year, Before use, should be
thawed in the blood bank in water which is between 30C to 37C. Higher
temperatures will destroy clotting factors and proteins, once thawed,
should be stored in a refrigerator at +2C to +6C
Indications: Replacement of multiple coagulation factor deficiencies: e.g.
Liver disease, Warfarin (anticoagulant) overdose, Depletion of
coagulation factors in patients receiving large volume transfusions,
Disseminated intravascular coagulation (DIC), Thrombotic
thrombocytopenic purpura (TTP)
Precautions: Acute allergic reactions are not uncommon, especially with
rapid infusions
_ Severe life-threatening anaphylactic reactions occasionally occur
_ Hypovolemia alone is not an indication for use Dosage Initial dose of
15 ml/kg
Administration: Must normally be ABO compatible to avoid risk of
hemolysis in recipient
_ No compatibility testing required
_ Infuse using a standard blood administration set as soon as possible
after thawing
_ Labile coagulation factors rapidly degrade; use within 6 hours of
thawing
CRYOPRECIPITATE
Description: Prepared from fresh frozen plasma by collecting the
precipitate formed during controlled thawing at +4C and resuspending it
in 10–20 ml plasma. Contains about half of the Factor VIII and
fibrinogen in the donated whole blood: e.g. Factor VIII: 80–100 iu/pack;
fibrinogen: 150–300 mg/pack
Infection risk as for plasma, but a normal adult dose involves at least 6
donor exposures
Storage: At –25C or colder for up to 1 year
Indications: As an alternative to Factor VIII concentrate in the treatment
of inherited deficiencies of: von Willebrand Factor (von Willebrand’s
disease) Factor VIII (hemophilia A), Factor XIII, as a source of
fibrinogen in acquired coagulopathies: e.g. disseminated intravascular
coagulation (DIC)
Administration: If possible, use ABO-compatible product
_ No compatibility testing required
_ After thawing, infuse as soon as possible through a
standard blood administration set
_ Must be infused within 6 hours of thawing
Plasma derivatives
HUMAN ALBUMIN SOLUTIONS

Description: Prepared by fractionation of large pools of donated plasma
Preparations :Albumin 5%: contains 50 mg/ml of albumin
Infection risk: No risk of transmission of viral infections if correctly
manufactured
Indications: Replacement fluid in therapeutic plasma exchange: use
albumin 5%, Treatment of diuretic-resistant edema in hypoproteinemia
patients: e.g. nephrotic syndrome or ascites.
COAGULATION FACTORS
Factor VIII concentrate
Description: Partially purified Factor VIII prepared from large pools of
donor plasma. Factor VIII ranges from 0.5–20 iu/mg of protein.
Preparations with a higher activity are available
all heated and/or chemically treated to reduce the risk of transmission
of viruses
Storage: +2C to +6C up to stated expiry date,
Indications: Treatment of hemophilia A,
Alternatives: Cryoprecipitate, fresh frozen plasma
PLASMA DERIVATIVES CONTAINING FACTOR IX, Prothrombin
complex concentrate (PCC), Factor IX concentrate
Infection risk As Factor VIII
Storage as Factor VIII
Indications: Treatment of hemophilia B (Christmas disease)
IMMUNOGLOBULINS
Immunoglobulin for intravenous use
Description As for intramuscular preparation, but with subsequent
processing to render product safe for IV administration
Indications: Idiopathic autoimmune thrombocytopenic purpura and some
other immune disorders
_ Treatment of immune deficiency states
_ Hypogammaglobulinaemia
_ HIV-related disease
Red cell compatibility testing
It is essential that all blood is tested before transfusion in order to: Ensure
that transfused red cells are compatible with antibodies in the recipient’s
plasma
All pre-transfusion test procedures should provide the following
information about both the units of blood and the patient: ABO group,
RhD type, Presence of red cell antibodies that could cause hemolysis in
the recipient.
The ABO blood groups are the most important in clinical transfusion
practice. There are four main red cell types: O, A, B and AB.

All healthy normal adults of group A, group B and group O have
antibodies in their plasma against the red cell types (antigens) that they
have not inherited:
_ Group A individuals have antibody to group B
_ Group B individuals have antibody to group A
_ Group O individuals have antibody to group A and group B
_ Group AB individuals do not have antibody to group A or B.
These antibodies are usually of IgM and IgG class and are normally able
to hemolyze (destroy) transfused red cells.
RED CELL COMPONENTS
In red cell transfusion, there must be ABO and RhD compatibility
between the donor’s red cells and the recipient’s plasma.
1 Group O individuals can receive blood from group O donors only
2 Group A individuals can receive blood from group A and O donors
3 Group B individuals can receive blood from group B and O donors
4 Group AB individuals can receive blood from AB donors, and also
from group A, B and O donors
PLASMA AND COMPONENTS CONTAINING PLASMA
In plasma transfusion, group AB plasma can be given to a patient of any
ABO group because it contains neither anti-A nor anti-B antibody.
1 Group AB plasma (no antibodies) can be given to any ABO group
patients
2 Group A plasma (anti-B) can be given to group O and A patients
3 Group B plasma (anti-A) can be given to group O and B patients
4 Group O plasma (anti-A + anti-B) can be given to group O patients
only
A direct test of compatibility (crossmatch) is usually performed before
blood is infused. This detects a reaction between:
_ Patient’s serum
_ Donor red cells.
The laboratory performs:
_ Patient’s ABO and RhD type
_ Direct compatibility test or crossmatch.
These procedures normally take about 1 hour to complete. Shortened
procedures are possible, but may fail to detect some incompatibilities.

acute transfusion reactions
CATEGORY 1: MILD REACTIONS
Signs Symptoms Possible cause
Localized Pruritus Hypersensitivity
cutaneous reactions:
— Urticaria
— Rash
CATEGORY 2: MODERATELY SEVERE REACTIONS
Signs Symptoms Possible cause
_ Flushing Anxiety Hypersensitivity
_ Urticaria Pruritus Febrile non-hemolytic
_ Rigors Palpitations transfusion reactions
_ Fever Mild dyspnea possible contamination
_ Restlessness Headache pyrogens and/ or bacteria
_Tachycardia
CATEGORY 1: MILD REACTIONS
Immediate management
1 Slow the transfusion.
2 Administer antihistamines IM (e.g. chlorpheniramine 0.1 mg/kg or
equivalent).
3 If no clinical improvement within 30 minutes or if signs and symptoms
worsen, treat as Category 2.
CATEGORY 2: MODERATELY SEVERE REACTIONS
Immediate management
1 Stop the transfusion. Replace the infusion set and keep IV line open
with normal saline.
2 Send blood unit with infusion set, freshly collected urine and new blood
samples from vein opposite infusion site with appropriate request form to
blood bank for laboratory investigations.
3 Administer antihistamine IM (e.g. chlorpheniramine 0.1 mg/kg or
equivalent) and oral or rectal antipyretic (e.g. paracetamol 10 mg/kg:
500 mg – 1 g in adults). Avoid aspirin in thrombocytopenic patients.
4 Give IV corticosteroids and bronchodilators if there are anaphylactoid
features (e.g. bronchospasm, stridor).
5 Collect urine for next 24 hours for evidence of hemolysis and send to
laboratory.
8 If clinical improvement, restart transfusion slowly with new blood unit
and observe carefully.
9 If no clinical improvement within 15 minutes or if signs and symptoms
worsen, treat as Category 3.

CATEGORY 3: LIFE-THREATENING REACTIONS
Signs
_ Rigors
_ Fever
_ Restlessness
_ Hypotension (fall of >20% in systolic BP)
_ Tachycardia (rise of >20% in heart rate)
_ Hemoglobinuria(red urine)
_ Unexplained bleeding (DIC)
Symptoms
_ Anxiety
_ Chest pain
_ Pain near infusion site
_ Respiratory distress/ shortness of breath
_ Loin/back pain
_ Headache
_ Dyspnea
Possible causes
_ Acute intravascular hemolysis
_ Bacterial contamination and septic shock
_ Fluid overload
_ Anaphylaxis
_ Transfusion associated acute lung injury (TRALI)
CATEGORY 3: LIFE-THREATENING REACTIONS
Immediate management
1 Stop the transfusion. Replace the infusion set and keep IV line open
with normal saline.
2 Infuse normal saline (initially 20–30 ml/kg) to maintain systolic BP. If
hypotensive, give over 5 minutes and elevate patient’s legs.
3 Maintain airway and give high flow oxygen by mask.
4 Give adrenaline (as 1:1000 solutions) 0.01 mg/kg body weight by slow
intramuscular injection.
5 Give IV corticosteroids and bronchodilators if there are anaphylactic
features (e.g. bronchospasm, stridor).
6 Give diuretic: e.g. frusemide 1 mg/kg IV or equivalent.
7 Notify the doctor responsible for patient and blood bank immediately.
8 Send blood units with infusion set, fresh urine sample and new blood to
lab
9 Check a fresh urine specimen visually for signs of hemoglobinuria.
10 Start a 24-hour urine collection and fluid balance chart and record all
intake and output. Maintain fluid balance.
Acute intravascular hemolysis

Acute intravascular hemolysis
1 Acute intravascular hemolytic reaction is caused by the infusion of
incompatible red cells. Antibodies in the patient’s plasma hemolyzed the
incompatible transfused red cells.
2 Even a small volume (10–50 ml) of incompatible blood can cause a
severe reaction and larger volumes increase the risk.
3 The most common cause is an ABO incompatible transfusion.
This almost always arises from: Errors in the blood request form...
4 Antibodies in the patient’s plasma against other blood group antigens of
the transfused blood, such as Kidd, Kell or Duffy systems, can also cause
acute intravascular hemolysis.
Bacterial contamination and septic shock
1. Bacterial contamination affects up to 0.4% of red cells and 1–2% of
platelet concentrates.
2. Blood may become contaminated by:
_ Bacteria from the donor’s skin during blood collection (usually skin
staphylococci)
_ A bacteremia present in the blood of a donor at the time the blood is
collected (e.g. Yersinia)
_ Improper handling in blood processing
_ Defects or damage to the plastic blood pack
_ Thawing fresh frozen plasma or cryoprecipitate in a water bath (often
contaminated).
3. Some contaminants, particularly Pseudomonas species, grow at 2C to
6C and so can survive or multiply in refrigerated red cell units. The risk
therefore increases with the time out of refrigeration.
4. Staphylococci grow in warmer conditions and proliferate in platelet
concentrates at 20C to 24C, limiting their storage life.
5. Signs usually appear rapidly after starting infusion, but may be delayed
for a few hours.
6. A severe reaction may be characterized by sudden onset of high fever,
rigors and hypotension.
7. Urgent supportive care and high-dose intravenous antibiotics are
required.
Fluid overload
1 Fluid overload can result in heart failure and pulmonary edema.
2 May occur when:
_ Too much fluid is transfused
_ The transfusion is too rapid
_ Renal function is impaired.
Anaphylactic reaction
1 A rare complication of transfusion of blood components or plasma
derivatives.
2 The risk is increased by rapid infusion, typically when fresh frozen
plasma is used as an exchange fluid in therapeutic plasma exchange.
3 Cytokines in the plasma may be one cause of bronchoconstriction and
vasoconstriction in occasional recipients.
4 IgA deficiency in the recipient is a rare cause of very severe
anaphylaxis. This can be caused by any blood product since most contain
traces of IgA.
5 Occurs within minutes of starting the transfusion and is characterized
by:
_ Cardiovascular collapse
_ Respiratory distress
_ No fever.
6 Anaphylaxis is likely to be fatal if it is not managed rapidly and
aggressively.
Transfusion-associated acute lung injury (TRALI)
1 Usually caused by donor plasma that contains antibodies against the
patient’s leucocytes.
2 Rapid failure of pulmonary function usually presents within 1 to 4
hours of starting transfusion, with diffuse opacity on the chest X-ray.
3 There is no specific therapy. Intensive respiratory and general support
in an intensive care unit is required.
Delayed complications of transfusion
Delayed hemolytic transfusion reactions
Signs and symptoms
1 Signs appear 5–10 days after transfusion:
_ Fever
_ Anemia
_ Jaundice
_ Occasionally hemoglobinuria.
2 Severe, life-threatening delayed hemolytic transfusion reactions with
shock, renal failure and DIC are rare.
Post-transfusion purpura
1 A rare but potentially fatal complication of transfusion of red cells or
platelet concentrates, caused by antibodies directed against platelet-
specific antigens in the recipient.

2 Most commonly seen in female patients.
Graft-versus-host disease
1 A rare and potentially fatal complication of transfusion.
2 Occurs in such patients as:
_ Immunodeficient recipients of bone marrow transplants
_ Immunocompetent patients transfused with blood from
individuals with whom they have a compatible tissue type
(HLA: human leucocyte antigen), usually blood relatives.
Iron overload
There are no physiological mechanisms to eliminate excess iron and thus
transfusion-dependent patients can, over a long period of time,
accumulate iron in the body resulting in haemosiderosis.
transfusion-transmitted infections
The following infections may be transmitted by transfusion:
_ HIV-1 and HIV-2
_ HTLV-I and HTLV-II
_ Hepatitis B and C
_ Syphilis (Treponema pallidum)
_ Chagas disease (Trypanosoma cruzi)
_ Malaria
_ Cytomegalovirus (CMV)
Note:
Massive or large volume blood transfusions
‘Massive transfusion’ is the replacement of blood loss equivalent to or
greater than the patient’s total blood volume in less than 24 hours: 70
ml/kg in adults
