Cholera and other Vibrioses
Vibrio Cholerae Serogroups O1 and O139Key facts:
• Cholera is an acute diarrheal disease that can kill within hours if left untreated.
• There are an estimated 3–5 million cholera cases and 100 000–120 000 deaths due to cholera every year.
• Up to 80% of cases can be successfully treated with oral rehydration salts.
• Provision of safe water and sanitation is critical in reducing the impact of cholera and other waterborne diseases.
• Oral cholera vaccines are considered an additional means to control cholera, but should not replace conventional control measures.
• Identification:
• Cholera is an extremely virulent disease. It affects both children and adults. It characterized in its severe form by sudden onset, profuse painless watery stools (rice-water stool), nausea and profuse vomiting early in the disease. In untreated cases, rapid dehydration, acidosis, circulatory collapse, renal failure and rapid death.In most cases → asymptomatic or mild diarrhea [El Tor biotype]
Proper rehydration → CFR < 1%
Clinical
Asymptomatic (75%) Severe formPathogenesis
Not invasive mo → enterotoxin liberation → stimulate adenyl-cyclase in gut → massive fluid out put +poor absorption.
Dx
- Clinical
- Stool exam → transmitted by sea-water tubes
(alkaline peptone water) PH 9
Stool culture on TCBS media → yellow colony
- Dark field microscopy → vibrios moving like “shooting stars”
- Serological test
History
In 19th century → 6 pandemic waves from the gulf of Bengal to most of the world.Current seventh pandemic started in South Asia in 1961→ O1- El Tor biotype:
Started in Indonesia in 1961 → spread to the Asian mainland from 1963 to 1969 and reached Africa in 1970 and reached the Latin America in 1991 after a century of absence; where in 1994 → 1 million cases reported in different Latin American countries.
Cholera is now endemic in many countries.
2. Infectious agents:
V. cholerae O1 & O139Vibrio cholerae (O1) → 2 biotypes: Classical
El Toreach biotype → 3 serotypes Inaba
Ogawa
Hikojima
In 1992, new strain identified in Bangladesh
(O139 Bengal) caused epidemic in a population immune to V. cholerae O1.
O139 → new organism but same clinical pictures [same toxin]. This also spread to other Asian countries.
• Cholera due to El Tor differs from classical cholera in following aspects:
• Large number of mild & asymptomatic cases 1/100.• Hardier &remain viable for longer period in water.
• Longer period of shedding by patient & carriers (possibility of chronic carriers).
Survival of vibrios:
Temp 55 C˚ → kill in 15 minUV. → Kill bacteria stand freezing
cold climate → 1 Week
0 C˚ → several weeks
3. Occurrence:
Cholera is one of the oldest epidemic diseases. Epidemics and pandemics are strongly linked to the consumption of unsafe water, poor hygiene and crowded living conditions.The number of cholera cases reported to WHO continues to rise.
For 2008 alone, a total of 190 130 cases were notified from 56 countries, including 5143 deaths. Many more cases were unaccounted for due to limitations in surveillance systems and fear of trade and travel sanctions.
The true burden of the disease is estimated to be 3–5 million cases and 100 000–120 000 deaths annually.
In Zimbabwe epidemic 2008-2009 around 60 000 cases and 3100 deaths reported.
In Iraq:
Cholera is considered to be an endemic disease in many parts of Iraq since 1966 when the first cholera cases appeared.
Trends of cholera in the last 40 years show that each epidemic lasted several months followed by a second wave in the next year.
Recent outbreaks occurred in Iraq:
August 2007 – February 2008 ≈ 4500 casesAugust 2008 – December 2008 ≈ 1000 cases
2009 _ Only 6 sporadic cases
Laboratory-confirmed cholera cases—Iraq, 14/08/2007− 24/02/2008 (first outbreak)
• No. laboratory-confirmed• cholera cases
• No. deaths reported
• Date most recent case reported
• Date first case reported
• No. districts affected
• Province
• 3007
• 5
• 1/12/2007
• 14/08/2007
• 5
• Kirkuk
• 1238
• 14
• 17/11/2007
• 23/08/2007
• 13
• Sulaymaniyah
• 275
• 0
• 22/11/2007
• 5/9/2007
• 6
• Erbil
• 6
• 0
• 28/10/2007
• 7/9/2007
• 4
• Dahuk
• 5
• 0
• 7/10/2007
• 12/9/2007
• 3
• Tikrit
• 7
• 1
• 15/11/2007
• 15/9/2007
• 3
• Ninewa
• 138
• 3
• 13/12/2007
• 19/9/2007
• 5
• Baghdad
• 2
• 0
• 2/10/2007
• 19/9/2007
• 2
• Basra
• 3
• 0
• 20/9/2007
• 20/9/2007
• 1
• Wasit
• 2
• 1
• 3/10/2007
• 3/10/2007
• 1
• Anbar
• 15
• 0
• 3/10/2007
• 3/10/2007
• 3
• Diyala
• 4696
• CFR 0.5%
• 24
• 46
• Total
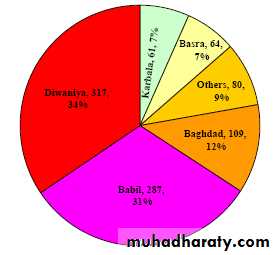
Second outbreak: % Distribution of confirmed cholera cases by province, up to 31/12/ 2008
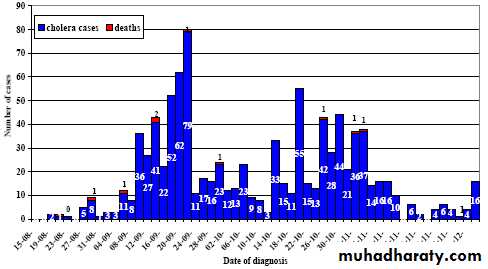
Confirmed cholera cases = 925Deaths = 11CFR = 1.2%Inaba serotypeReported cholera cases and deaths by date of diagnosis, Iraq, 14/08‐31/12/ 2008
Epidemic curveDistribution of confirmed cholera cases by age group up to 31/12/ 2008
Distribution of confirmed cholera cases by sex up to 31/12/ 20084. Reservoir:
Main reservoir is humansSick person
Convalescent patient
Carriers
5. Mode of transmission
Man 5-20% Man
Infected faeces
water &food
Man5. Mode of transmission
• Ingestion of an infective dose of contaminated food or water and can transmitted through many mechanisms.• Drinking water contaminated: at source, during transportation or during storage at home.
• Beverages, ice …etc.
6. Incubation period: few hours – 5 days, usually 2 – 3 days
7- Period of communicability:as long as stools are positive, usually only a few days after recovery. Occasionally the carrier state may persist for several months.
Tetracycline shorten the period of communicability.
8- Susceptibility: variable
Immunity: O1 classical biotype infection → protection against classical or El tor biotype long lasting or permanent; in contrast an initial clinical infection with El Tor → modest immunity limited to El Tor.Infection with O1 affords no protection against O139 infection and vice-versa.
Typical settings → periurban slums
Nutritional status → poor nutrition
Gastric acidity –(host factor) → protective
Normal person + 1011 M.O → infection
Normal person + antacid + 106 M.O → infection
Other clinical conditions (host factors)
cholecystitis
hook worms
Ascaris
Bd group O
Breast feeding → protective
• 9. Method of control:
• A- Preventive measures:• Educate the public …
• Personal hygiene particularly food handlers.
• Sanitary sewage disposal.
• Provide, protect, purify and chlorinate public water.
• Control flies.
• Use of sanitary practices for food preparation, handling and storage and pasteurization of milk.
• Vaccination
• Measures that inhibit the movement of people, foods or other goods are not provide effective to control cholera.
• Vaccination:
• Two oral cholera vaccines (OCV):
• Safe and provide significant protection (>50%) for 2 years against O1. Used by travelers to endemic areas.
• 1. live vaccine, single-dose.
• 2. killed vaccine, 2-dose regime.
• None is fully useful to be adopted as public health tool
• The use of the parenteral cholera vaccine has never been recommended by WHO due to its low protective efficacy and the high occurrence of severe adverse reactions.
B- Control of patients, contacts and environment:
• Reporting: obligatory (internationally), Class I reporting• Isolation: severely ill patients → Hospitalization + enteric precautions
• Less severe cases → out patient (oral rehydration + antimicrobial).
• Cholera wards can be operated.
• Disinfection of feces, vomit, linens and articles used by the patients by heat or carbonic acid.
• Quarantine: not applicable.
5. Management of contacts:
• Surveillance of persons who shared food and drink with a cholera patient for 5 days from last exposure.• Households contacts → chemoprophylaxis:
• Adults → tetracycline 500mg x 4/ day for 3 days
• or doxycycline 300 mg single dose.
• Children > 9 years → tetracycline 50mg/Kg/day for 3 days
• Children < 9 years → erythromycin 40mg/Kg/day for 3 days.
• Mass chemoprophylaxis of whole communities is never indicated (waste of resources and can lead to antibiotics resistance).
• Immunization of contacts is not indicated.
• Investigation of contacts and source of infection:
• - Investigate: polluted drinking water and contaminated food.
• - Stool culture is recommended only for household contacts.
7) Specific treatment:
• Objectives :Rapid fluid replacement [the cornerstone of cholera treatment is timely and adequate rehydration].
Antibiotic (tetracycline) — secondary to rehydration:
Shorten duration of diarrhea
Reduce the volume of rehydration fluids required
Shorten the duration of vibrio excretion
7) Specific treatment: cont.,
• - Mild to moderate dehydration → ORS• new formula of ORS [WHO-2002]:
• Nacl 75 mmol/L
• Trisodium citrate dihydrate 10 mmol/L
• Kcl 20 mmol/L
• glucose 75 mmol/L
• H2O 1 L
• Severe dehydration → rapid I.V. fluid
Types of fluid
Best Ringer-lactate (WHO IV formula)
“Dacca solution” can be prepared locally.
or what ever IV available
Antimicrobials:
• Adults → tetracycline 500 mg x 4/ day for 3 day or doxycycline 300 mg single dose.
• Children → tetracycline 12.5 mg/Kg/day for 3 days
• If resistant to tetracycline → erythromycin 250 mg x 4 for adults and 30mg/Kg/day for children, for 3 days.
• or ciprofloxacin 250 mg once daily for 3 days.
C- Epidemic measures:
• Educate the population at risk.• Provide effective treatment facilities and establishment of treatment centers (CTCs).
• Ensure a safe water supply. ↑ Chlorinate public water supplies (1.3 ppm) .Boil drinking; cooking water.
• Food sanitation.
• Discourage congregations and close swimming pools.
• Safe sewage disposal.
• Investigate to find source of infection (Time, place, person).
• OCV (optional) but if used in conjunction with the usual preventive and control measures.