Fetal assessment in the antenatal period &during labor18
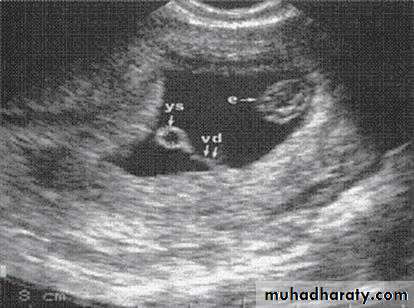
1.Diagnosis and confirmation of viability in early pregnancyThe gestational sac can be visualized from as early as 4–5 weeks of gestation and the yolk sac at about5 weeks .
The embryo can be observed and
measured at 5–6 weeks gestation.
A visible heartbeat can be visualized by about 6 weeks.
2.determination of gestational age andassessment of fetal size and growth
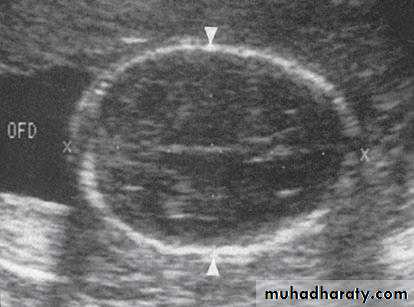
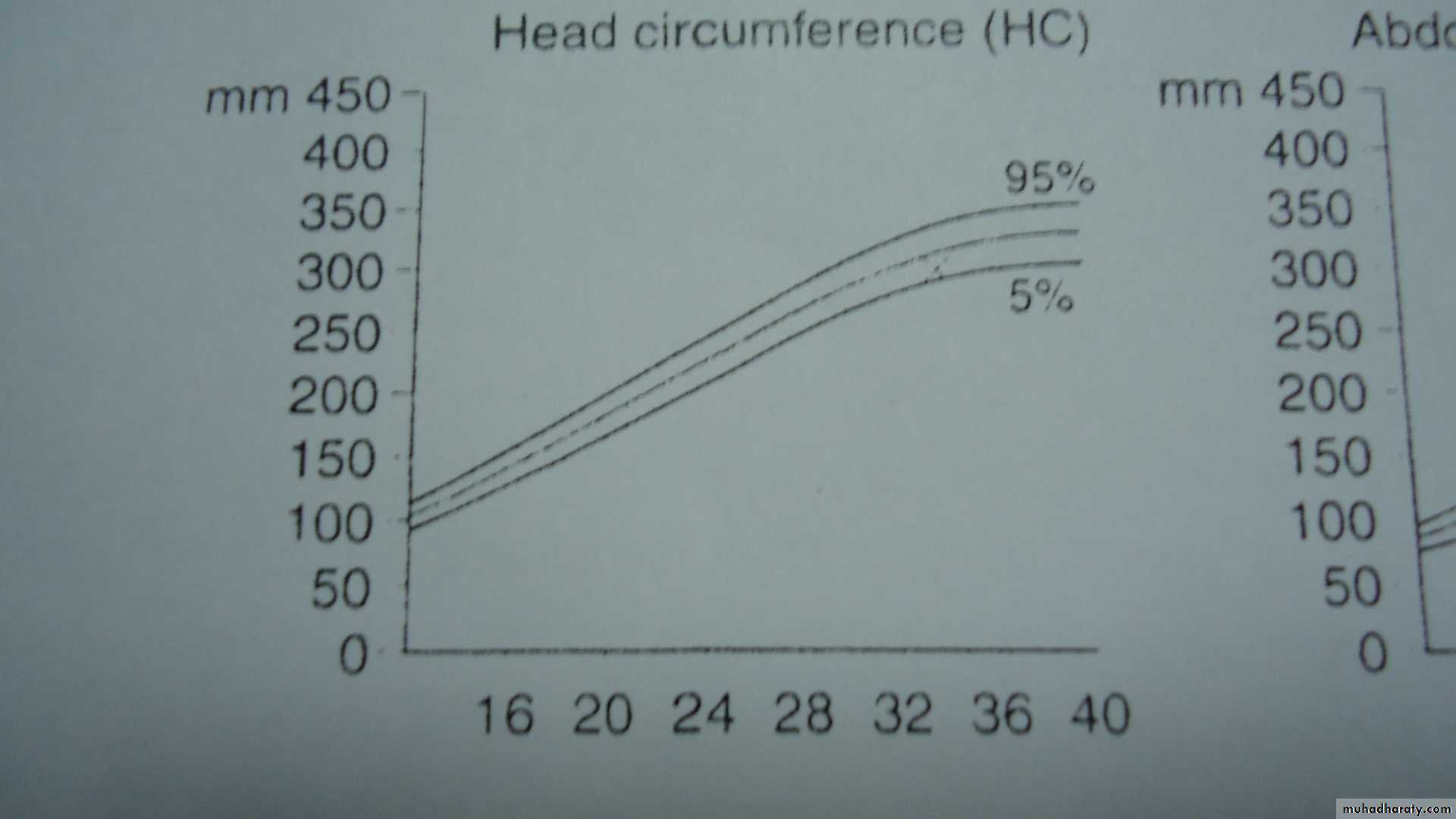
The crown-rump length (CRL)the head circumference (HC) from 14 to 20 weeks gestation.
The biparietal diameter (BPD)
femur length (FL)
Gestational age estimation
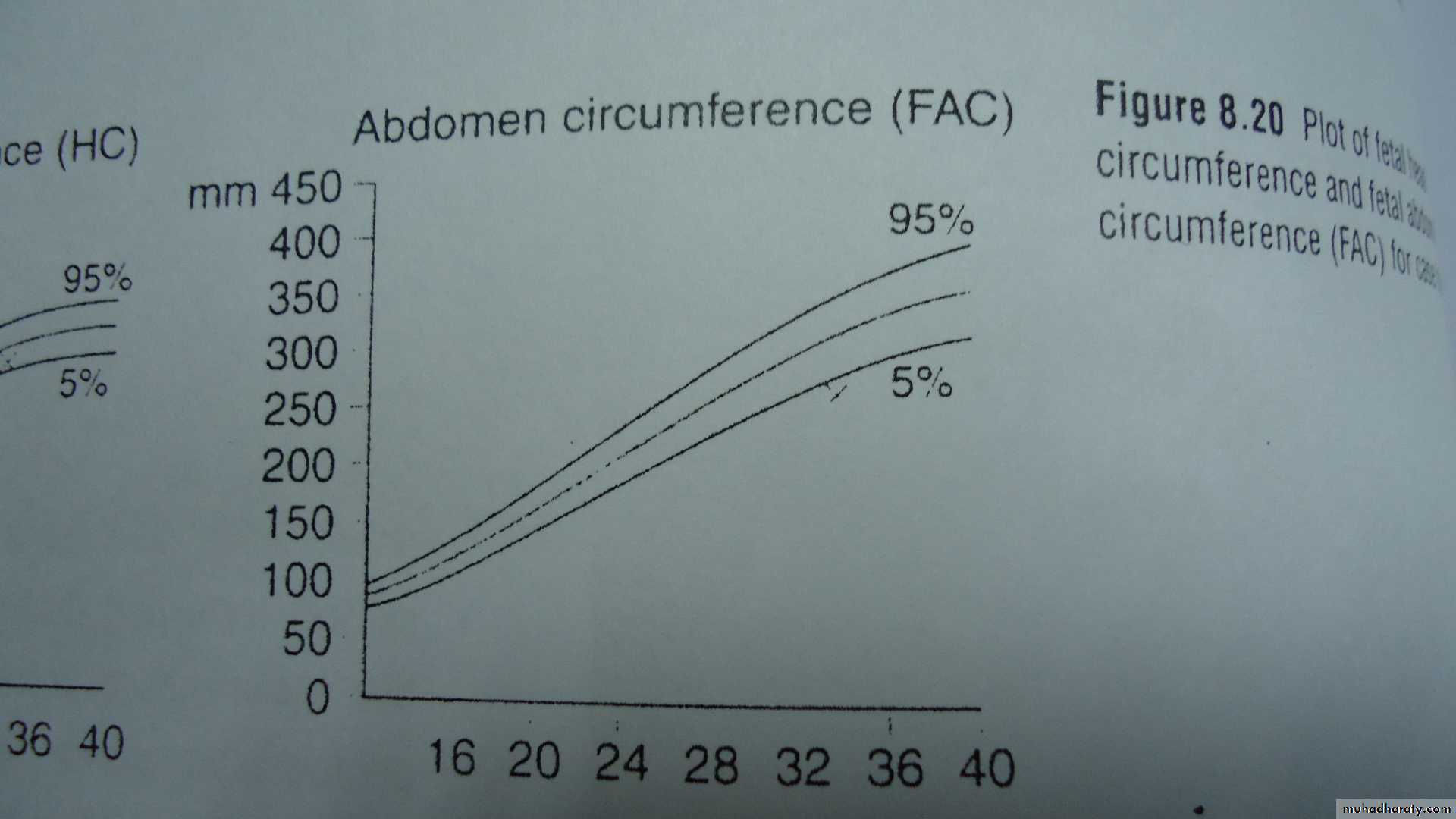
It is more accurate than prediction from the last menstrual period(LMP),even if the woman is certain of her datesIn the latter part of pregnancy, measuring fetal abdominal circumference (AC) and HC will allow assessment of the size and growth of the fetus and will assist in the diagnosis and management of fetal growth restriction. In addition to AC and HC,BPD and FL, when combined in an equation, provide a more accurate estimate of fetal weight (EFW) than any of the parameters taken singly
In pregnancies at high risk of fetal growth restriction (FGR) , serial measurements are plotted on the normal reference range. Growth patterns are helpful in distinguishing between different types of growth restriction (symmetrical and asymmetrical).
Asymmetry between head measures (BPD, HC) and AC can be identifi ed in FGR, where a brain-sparing effect will result in a relatively large HC compared with the AC
3.Multiple pregnancy
addition to identifying the presence of more than one fetus, it can also be used to determine the chorionicity of the pregnancy.Monochorionic twin pregnancies (i.e. those who‘share’ a placenta) are associated with an increased risk of pregnancy complications
In dichorionic twin there is thick inter-twin separating membrane.
In contrast to a monochorionic twin have very thin inter-twin septum
other method is by visualizing a tongue of placental tissue within the base of dichorionic membrane which is termed the twin peak or lambda sign.
.
4.Detection of chromosomal abnormality
In normal pregnancy during the first trimester ,a fluid filled area may be seen in the posterior surface of the fetal neck.There is a relation between the measurement of this nucal translucency(NT) &chromosomal &cardiac defect
At any given maternal age ,NT measurement, can be used to modify the age-related risk of fetal trisomy.
5.Placental localization
ultrasonographic identification
of the lower edge of the placenta to exclude or confirm placenta praevia as a cause for antepartum haemorrhage is now a part of routine clinical practice.
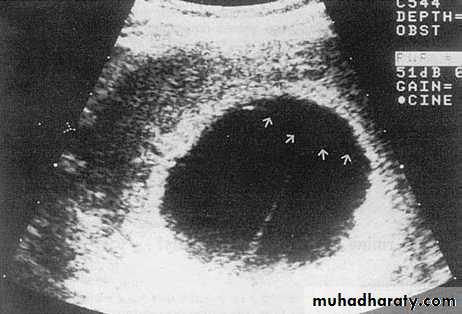
6.Amniotic fluid volume assessment
Ultrasound can be used to identify both increasedand decreased amniotic fluid volumes. The fetus has a role in the control of the volume of amniotic fluid.Fetal growth restriction can be associated with reduced amniotic
Amniotic fluid assessment
1-The maximum vertical pool of less than 2 cm suggest oligohydramnios, and measurements of greater than 8 cm suggest polyhydramnios.2-The Amniotic Fluid Index (AFI)
The AFI alters throughout gestation, but in the third
trimester it should be between 10 and 25 cm; values
below 10 cm indicate a reduced volume and those
below 5 cm indicate oligohydramnios, while values
above 25 cm indicate polyhydramnios.
7.Measurement of cervical length
Evidence suggests that approximately 50 per cent ofwomen who deliver before 34 weeks gestation will
have a short cervix. The length of the cervix can be
assessed using transvaginal scanning.
8.Other uses
Ultrasonography is also of value in other obstetric conditions such as:
• confi rmation of intrauterine death;
• confi rmation of fetal presentation in uncertain cases;
• diagnosis of uterine and pelvic abnormalities
during pregnancy, for example fi bromyomata and ovarian cysts.
U/S in 3rd trimester
The aims areTo assess fetal growth
To assess fetal well-being
U/Sin3rd trimester
To assess fetal growthTo assess fetal well-being
Assessing fetal well-being in 3rd trimester
The cardiotocograph CTGIs an indirect method of monitoring fetal heart rate.
The mother should be comfortable &in left lateral or semi-recumbent position .an external ultrasound transducer for monitoring fetal heart &a tocodynometer for recording uterine activity are secured overlying the uterus for at least 30 min
It is used to study:fetal heart rate,variability, accelerations,decelerations &maternal uterine contractions
• 1 Baseline fetal heart rate
It falls with advancing gestational age as a result of maturing fetal parasympathetic (vagal) toneNormal fetal heart at term is110-150 while prior to term 160 is normal
Fetal tachycardia can be due to
Cogenital tachycardia,maternal or fetal infection,acute fetal hypoxia,fetal anemia,drugs like?
2 Fetal heart rate variability
Other longer-term fluctuation in heart rate occuring 2-6 times per min this is termed [baseline variabilty] which reflects normal fetal autonomic nervous system3 Fetal heart rate accelerations
These are increase in baseline fetal heart rate of at least 15bpm, lasting for at least15 sec.The presence of 2 or more accelerations on a 20-30 min CTG, defines a reactive trace.
The normal ante partum fetal CTG:-
Baesline of 110-150,with baseline variability exceeding 10bpm,&with more than one acceleration seen in a 20-30min tracing4 Fetal heart rate decelerations
These are transient reductions in fetal heart of 15 bpm or more,lasting for more than15 secDecelerations that occur in the presence of other abnormal features e.g. reduced variability or baseline tachycardia are more likely to reflect fetal hypoxia
Stress & non stress CTG
An antenatal CTG performed with the mother positioned comfortably is called a non stress test.sub optimal results of this test ,leads to do contraction stress test .
contracion indused by oxytocin or other ways
+ve test result is fetal cardiac decelerations in response to uterine contraction &is abnormal
Computerized CTG
Have been shown to be equal or superior to human interpretation in differentiating normal from abnormal outcome.Biophysical profile
u/s can be used for detailed fetal parameters to assess wellbeing & define fetus at riskFetal breathing movement
Gross body movementFetal tone
Reactive fetal heart rateQualitative amniotic fluid
>1 episode for 30s in 30 min>3body/limb movement in 30 min
>1episode body/limp extension then flectuion
>2accelerations with fetal movement in 30min>1pool of fluid, at least 1cmX1cm
Abscent /<30s jn 30 min<3body movement in 30min
Slow or absent extension-flection<2 accelerations or 1+deceleration in 30 min
Either no measurable pool or a pool <1cmX1cmBiophysical variable
Normal -score 2
Abnormal –score 0
Doppler u/s
Make use of the phenomenon of the doppler fequency shift ,where the reflected waves will be at a different frequency from the transmitted one if it interacte with moving structures.color doppler the Doppler signals can be displayed as a color map blood flowing towards the trasducer shown in sheds of red;&if away its color is blue.
Diastolic flow in the umblical artery increases with gestation
Doppler of fatal vessels
Falling oxygen level in the fetus result in a redistribution of blood flow to protect the brain,heart,adrenals &spleen,&reditriution in all other vessels.
The middle cerebral artery will show increasing diastolic flow(falling pulsatility index)
Fetal monitoring during labor
The objective of fetal monitoring during labour is the prediction and diagnosis of fetal asphyxia before fetal/newborn morbidity with particular reference to brain damage has occurred.Fetal asphyxia is defined as ‘a condition of impaired blood gas exchange leading, if it persists, to progressive hypoxemia and hypercapnia’
Fetal monitoring
Insufficiant oxygen delivery to the fetus causes metabolic acidosis which,in the extrem can cause neuronal damage and permanent neurological injury.Hypoxia &acidosis cause characterstic chage in fetal heart rate pattern, which can be detected by CTG.
Fetal assessment in labor
Takes 4 forms1 observation of the color of the liquor-fresh meconium staining &heavy bleeding.
Mecoium is passed by a healthy fetus at or of after term as a result of gastrointestinal maturity;where it is thin&very dark green color.it also expelled from a fetus who exposed to marked intrauterine hpoxia or acidosis where it is thiker&much brighter green
Regular recording of liquior color&fetal heart should be recorded every 15 min if meconium found.during&after contraction
2 intermitent auscultation of the fetal heart using a pinard stethoscpe or a hand hold Dopler u/s
3cotiuous external fetal monitoring(EFM) usingCTG.
4fetal scalp blood sampling(FBS)
If the patient is a low-risk pregnancy, the FHR tracing should be reviewed every 30 minutes in the first stage of labor and every 15 minutes during the second stage.
The corresponding frequency for high risk parturients is 15 and 5 minutes.
Detection of either abnormal fetal heart baseline rate or decelerations by intermittent auscultation,is an indication for (EFM).
In 2nd stage of labor fetal heart should be listened to during &after every contraction.IF ANY RISK FACTOR, contiuous EFMis indicated which done by either abdominal transducer or fetal scalp electrode.
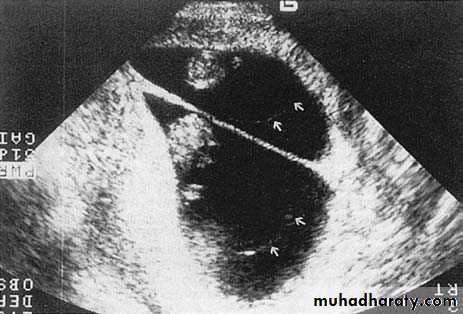
Ultrasound and invasive procedures
Ultrasound is used to guide invasive diagnostic procedures such as amniocentesis, chorion villus sampling and cordocentesis, and therapeutic procedures such as the insertion of fetal bladder shunts or chest drains.If fetoscopy is performed, the endoscope is inserted under ultrasound guidance.
precision to the appropriate place.
Summery
The early pregnancy scan (11–14 weeks)The principal aims of this scan are:
• to confi rm fetal viability;
• to provide an accurate estimation of gestational age;
• to diagnose multiple gestation, and in particular
to determine chorionicity;
• to identify markers which would indicate an
increased risk of fetal chromosome abnormality
such as Down’s syndrome;
• to identify fetuses with gross structural abnormalities
The 20 week scan (18–22 weeks)
The principal aims of this scan are:
• to provide an accurate estimation of gestationalage if an early scan has not been performed;
• to carry out a detailed fetal anatomical survey to detect any fetal structural abnormalities or
markers for chromosome abnormality;
to locate the placenta and identify the 5 per cent of
women who have a low-lying placenta for a repeatscan at 34 weeks to exclude placenta praevia;
• to estimate the amniotic fl uid volume.
Also, in some centres:
• to perform Doppler ultrasound examination of
maternal uterine arteries to screen for adverse
pregnancy outcome, for example pre-eclampsia;
• to measure cervical length to assess the risk of
preterm delivery.
Ultrasound in the third trimester
The principal aims of ultrasound in the thirdtrimester are:
• to assess fetal growth;