Al-Mustansiriyah University
College of Medicine - Department of Medicine
Division of Radiology
HEPATOBILIARY IMAGING
DR. ABDULLATEEF AL-BAYATI
Teaching Board Member
CABMS-RAD
IMAGING TECHNIQUES:
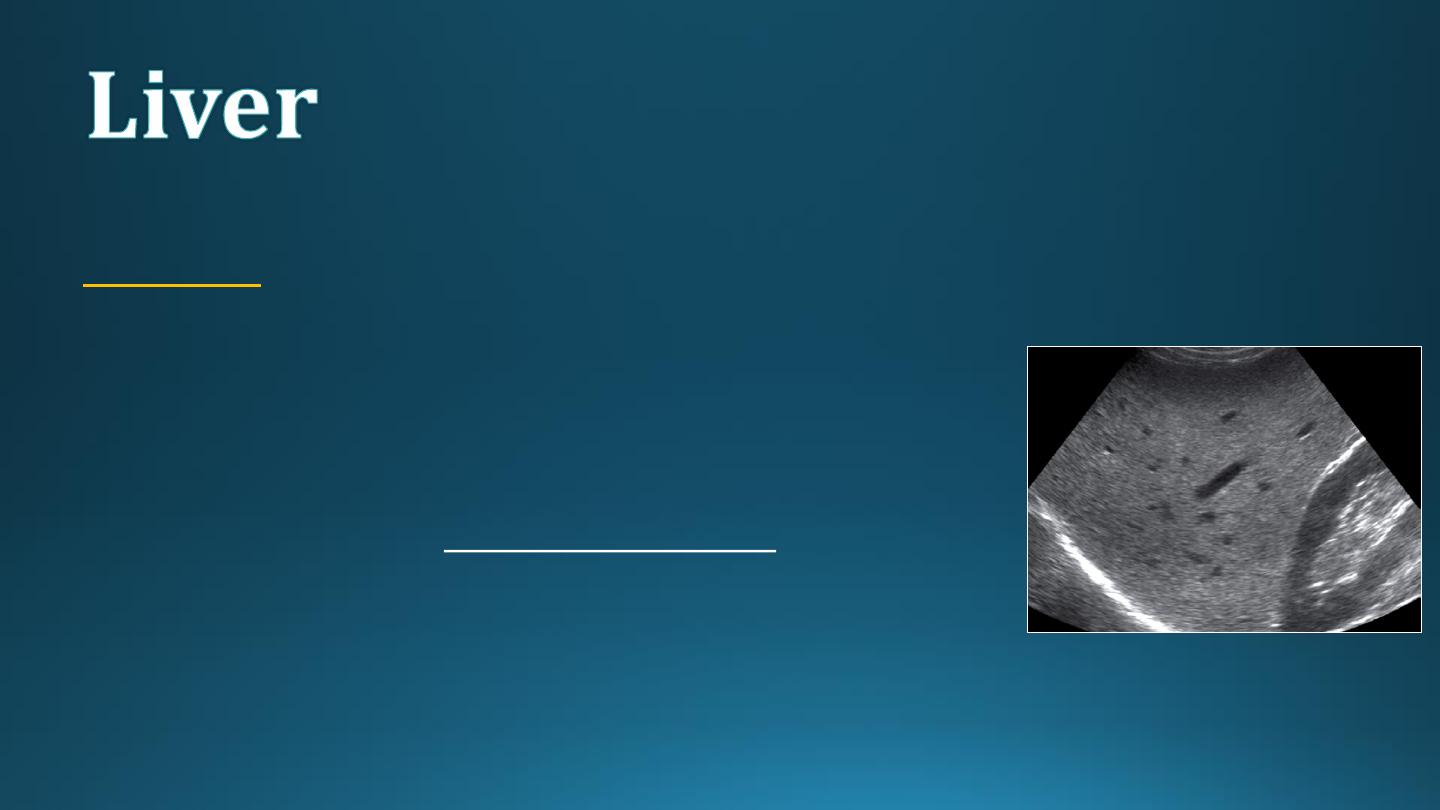
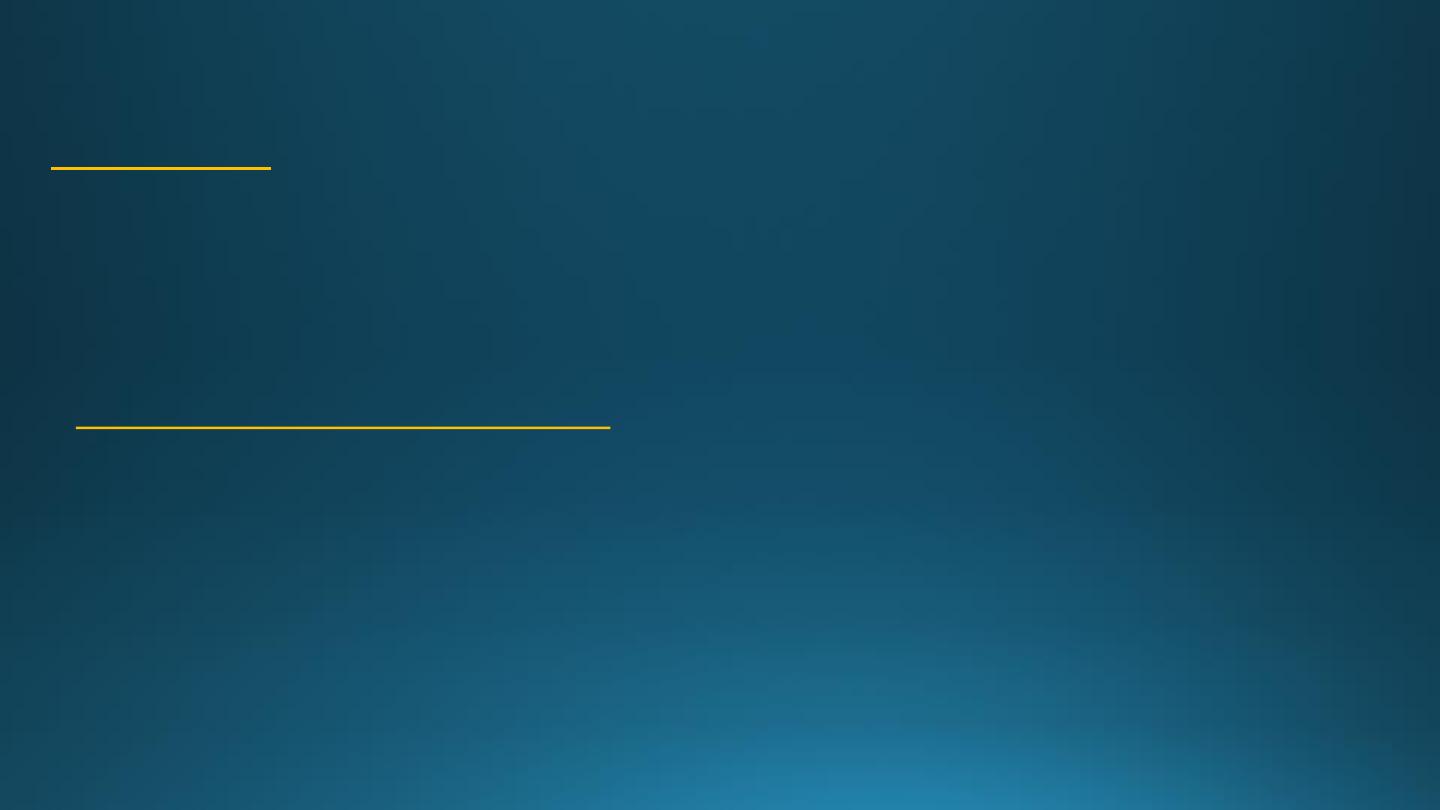
ULTRASOUND:
The normal liver parenchyma is of uniform echotexture with portal and
hepatic vessels.
The normal liver size and shape is variable.
Focal masses are noted as alteration of normal echo pattern.
They can be divided into cysts, solid or complex masses.
In practice, it is difficult to distinguish benign and malignant lesions unless
the mass is clearly a simple cyst.
When multiple masses are seen, metastatic disease is the likely diagnosis.
Other differential diagnosis include multiple abscesses and multiple
hemangiomas.
IMAGING TECHNIQUES:
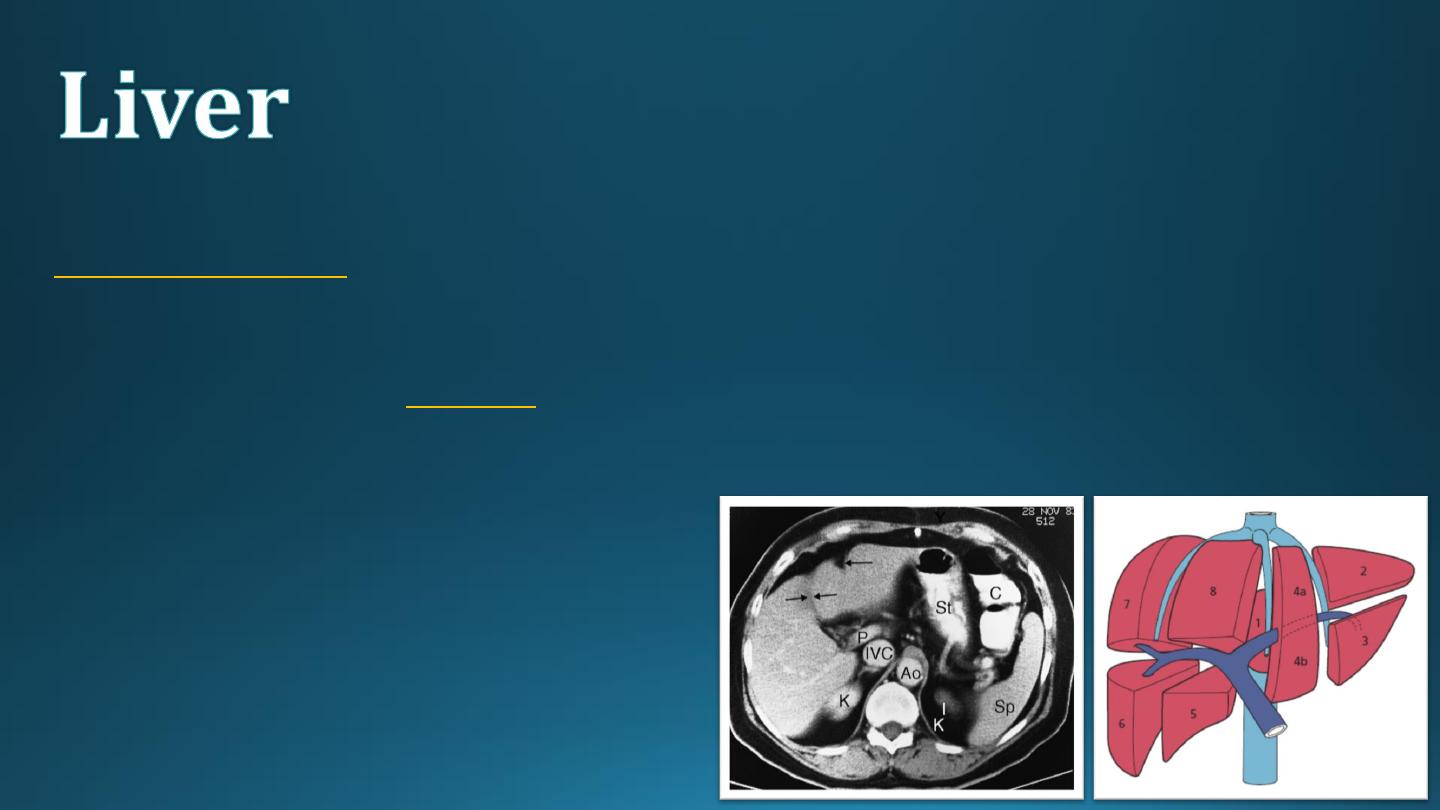
COMPUTED TOMOGRAPHY:
IV contrast is usually given to emphasize the density between normal parenchyma and pathological lesions.
The liver has dual blood supply from hepatic artery and portal vein.
The liver is divided into
8 segments
determined by hepatic and portal veins.
The normal liver is higher or equal in density to the spleen.
The normal intrahepatic bile ducts are not visible.
IMAGING TECHNIQUES:
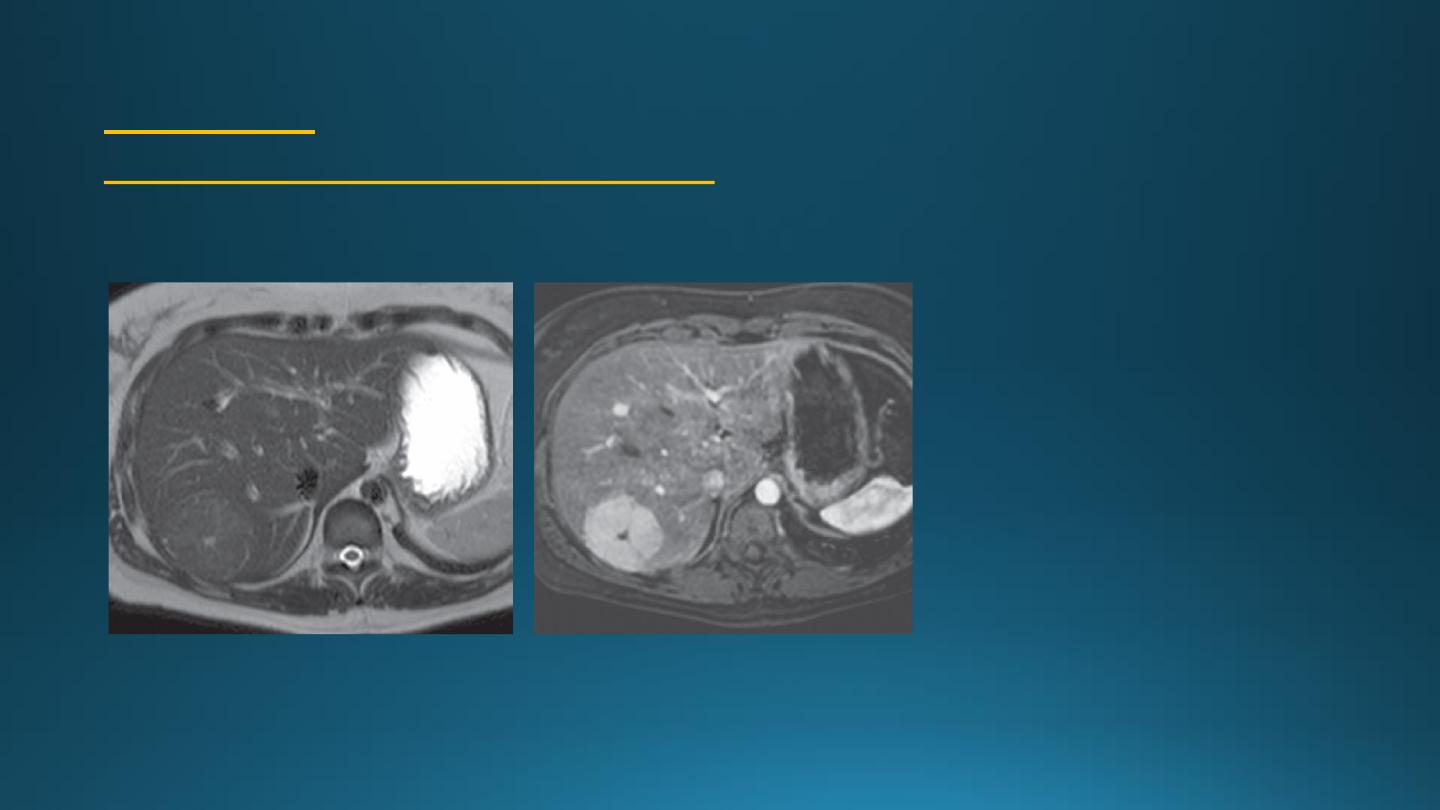
MAGNETIC RESONANCE IMAGING:
It is used as a problem-solving technique to give additional
information to US and CT scan.
It is a good technique for demonstrating primary and
secondary tumors.
IV contrast is used to improve visualization and help
characterize lesions.
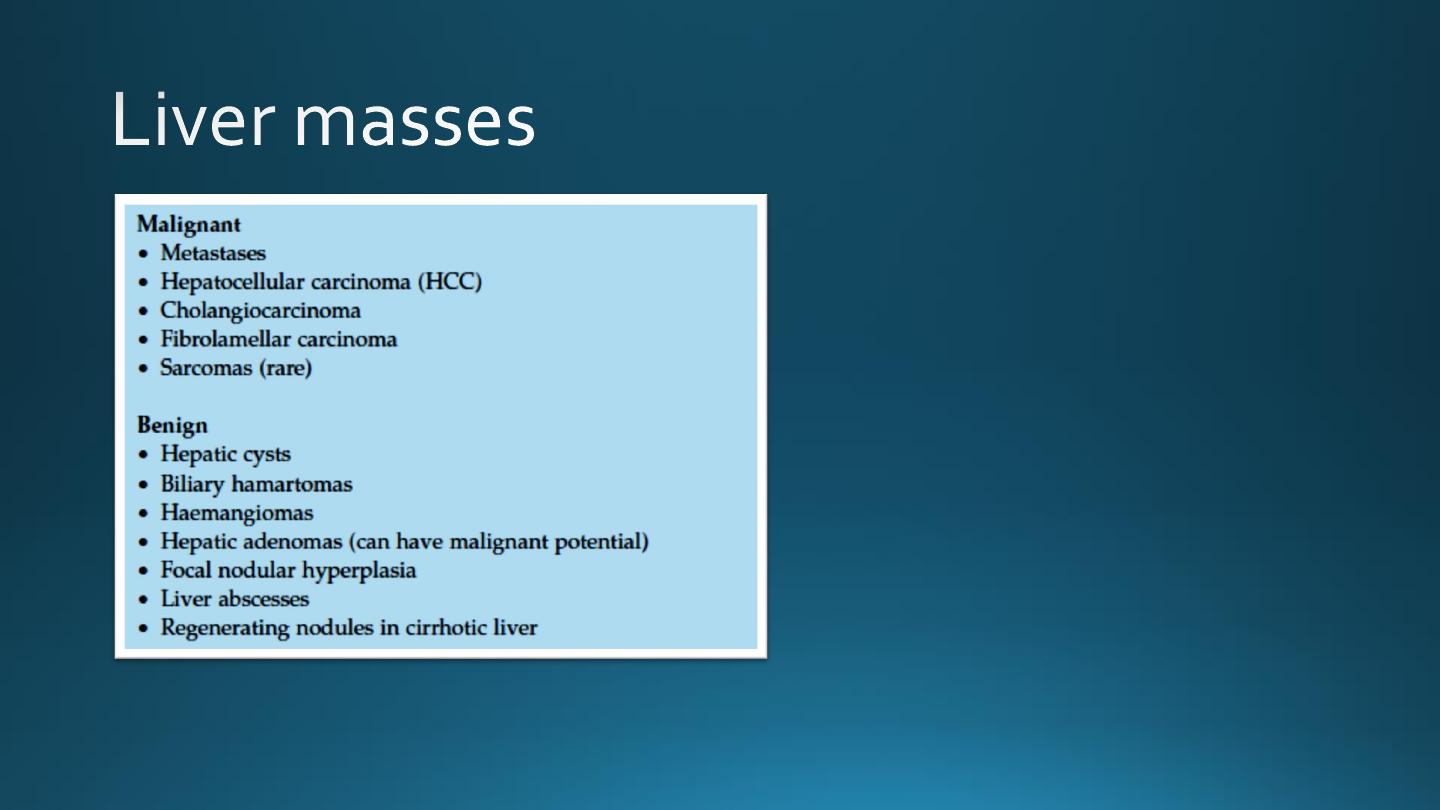

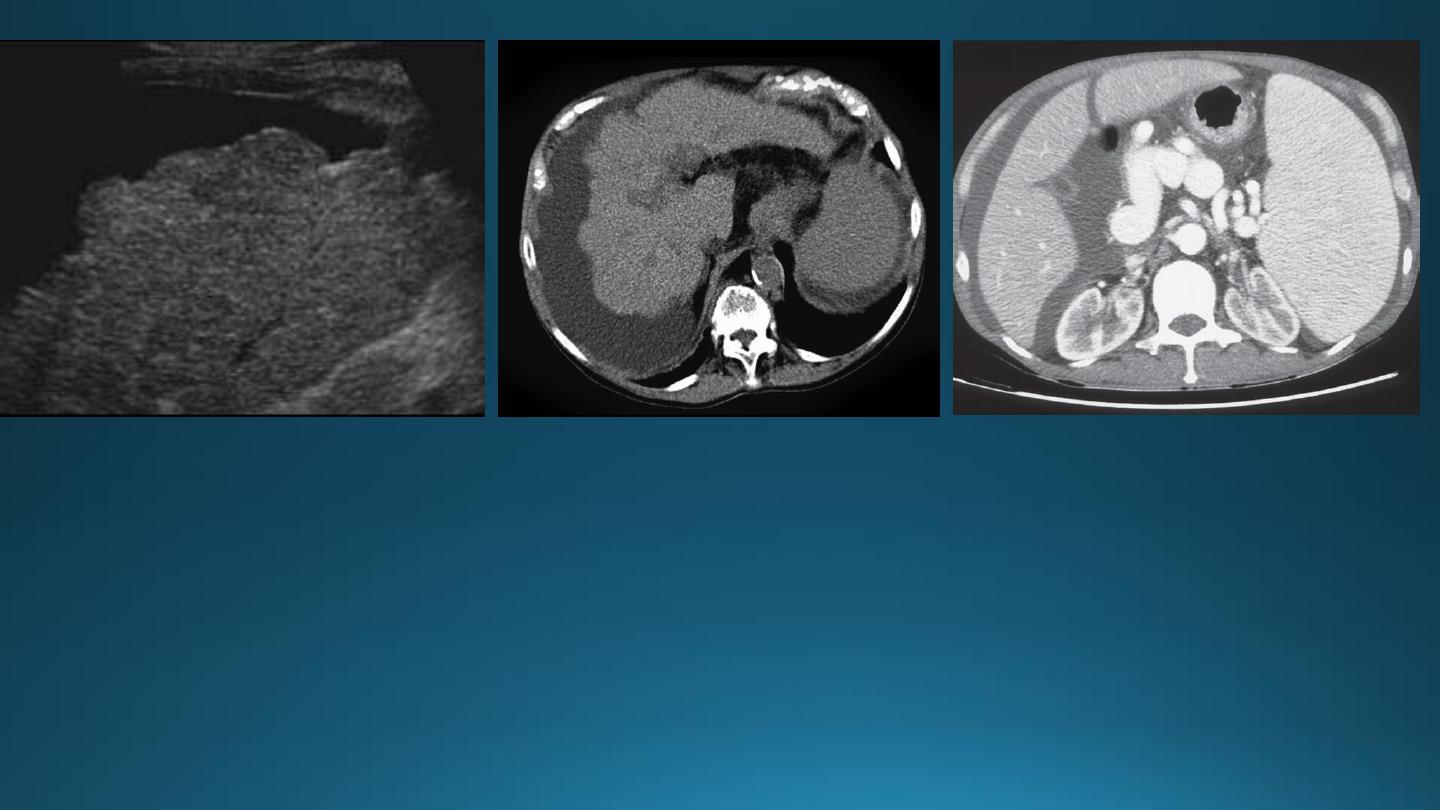
MALIGNANT LIVER NEOPLASMS
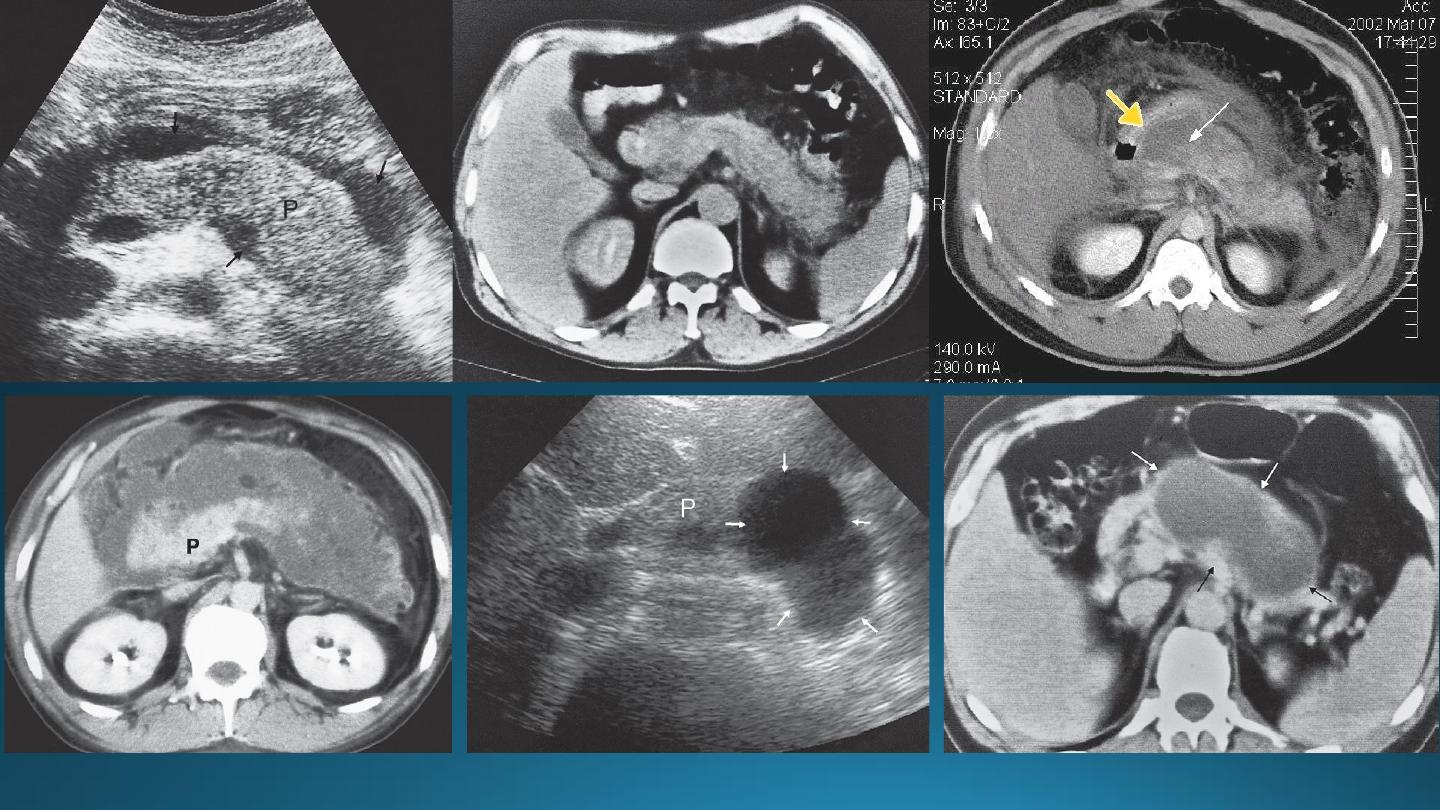
METASTASES
• Notably from carcinoma of stomach, colon, pancreas, lung and breast are much more common than
primary tumors.
• Metastases are often multiple, situated peripherally and of variable size.
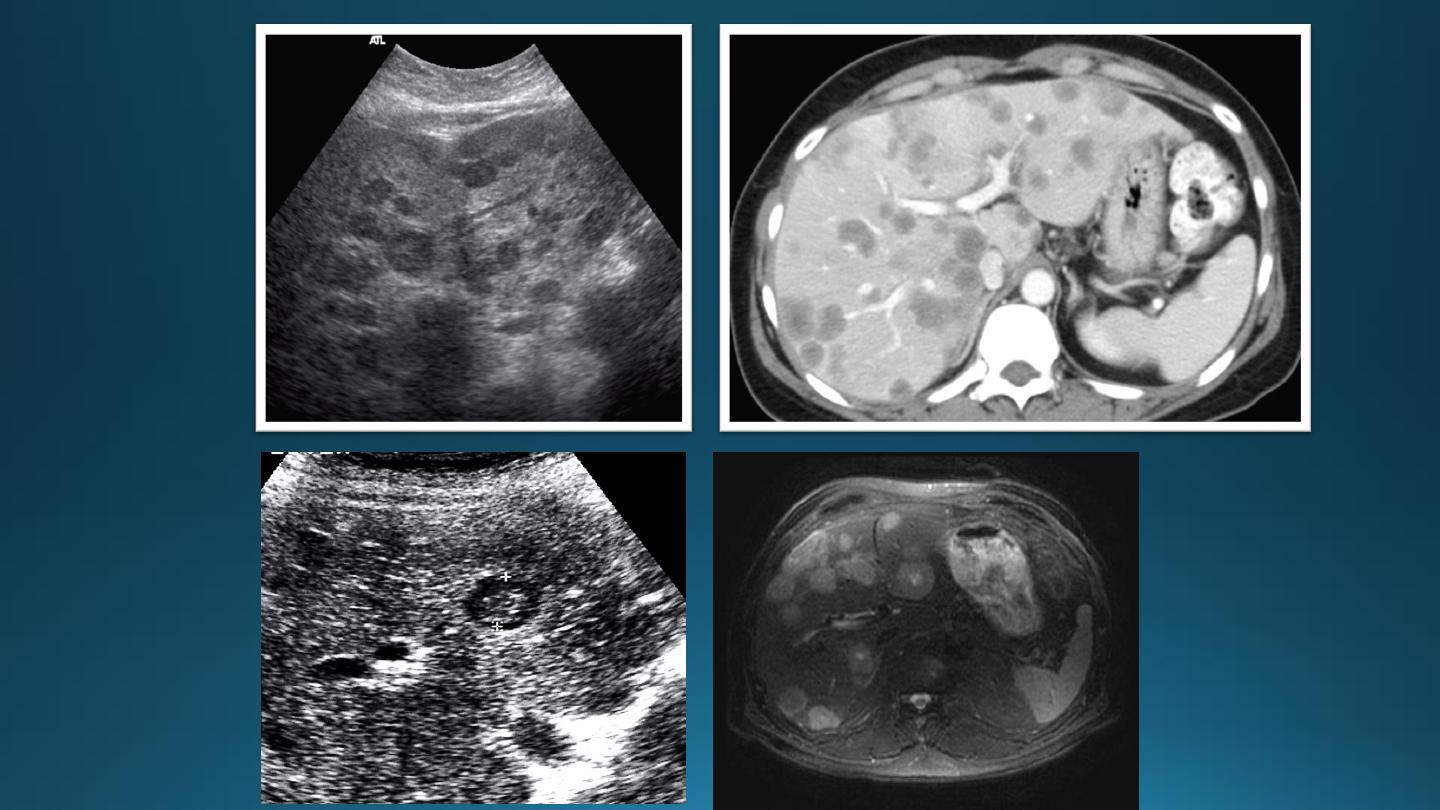
At US,
Solid or cystic or complex.
Isoechoic, hypoechoic or hyperechoic.
A metastases may have an echogenic center giving an appearance of "target lesion".
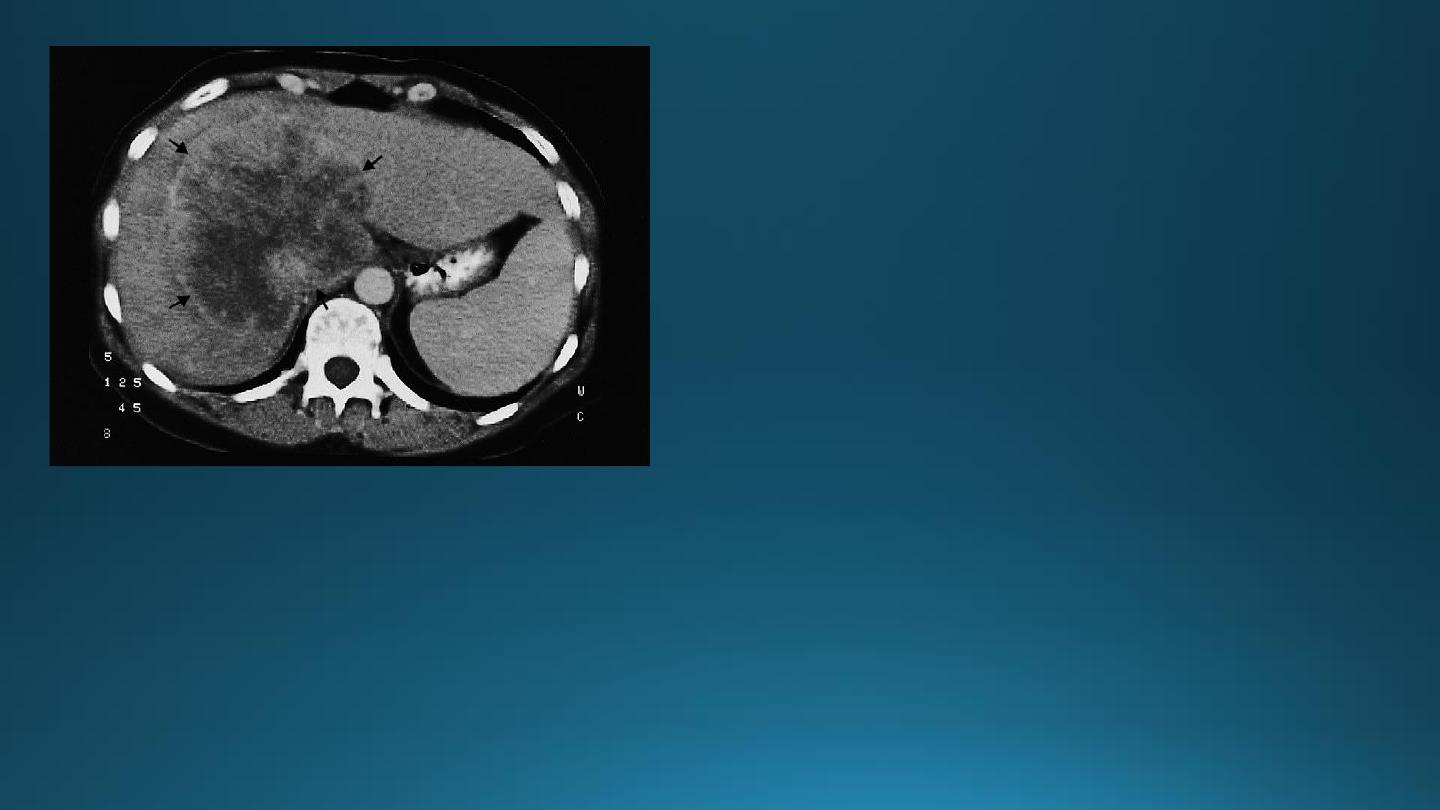
At CT,
metastases are seen as rounded areas, usually lower in density than normal liver parenchyma
with intense enhancement seen after IV contrast.
At MRI,
metastases typically have a signal lower than normal liver on T1 and a high signal intensity
on T2.
MALIGNANT LIVER NEOPLASMS
PRIMARY CARCINOMA
HEPATOMA
It is usually solitary , but may be multifocal.
70% associated with chronic liver disease.
Its CT,US and MRI features are similar to metastatic neoplasms.
CHOLANGIOCARCINOMA
FIBROLAMELLAR CARCINOMA
It is A rare tumor.
Often presenting in adolescents/young adults
A large mass, often with a central calcified scar.

BENIGN LIVER MASSES
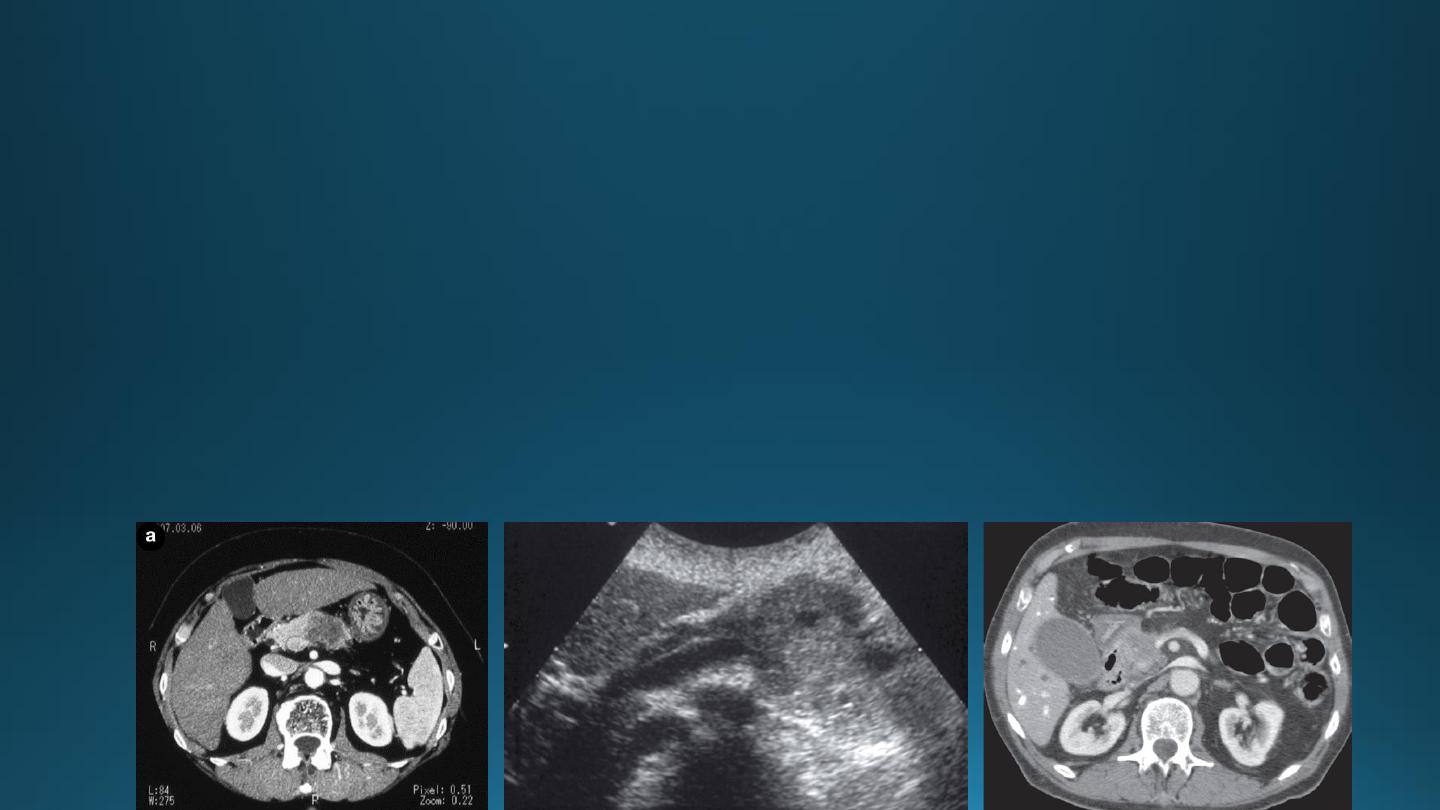
LIVER CYSTS
Simple cysts:
• may be single or multiple, usually congenital , some are due to infection
• Multiple hepatic cysts occur in adult polycystic disease
• US features of simple cyst: sharp margin, echofree, with acoustic enhancement
• CT features of simple cyst: very well defined margin with water density(HU=0 – 20).
• MRI features of simple cyst: low signal on T1 and high signal on T2.
• Simple cyst do not show enhancement after IV contrast in CT and MRI
Hydatid cysts
May be single or multiple
Few show calcified walls.
Daughter cysts may be seen within a main cyst at both US and CT.
Occasionally, metastases can have a cystic appearance.
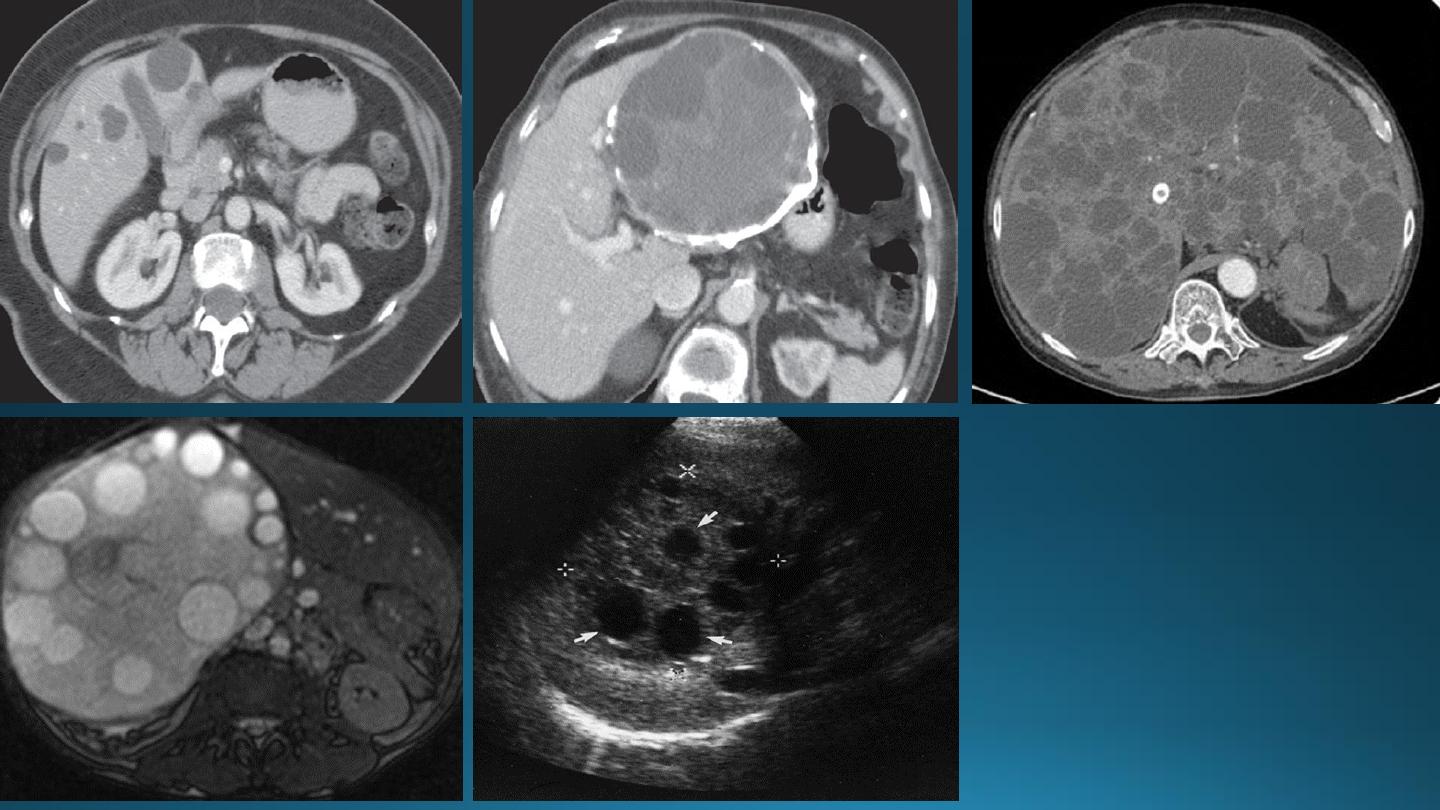
HEMANGIOMAS OF THE LIVER
They are the commonest benign tumors in liver.
They are common incidental finding and rarely requires treatment.
It may cause significant hemorrhage, especially after trauma, so percutaneous biopsy should be avoided.
Hemangiomas are typically well-defined, peripheral echogenic masses at US.
At CT, there is usually a characteristic peripheral, nodular and centripetal enhancement after IV contrast.
MRI shows uniform very high signal intensity on T2 images.
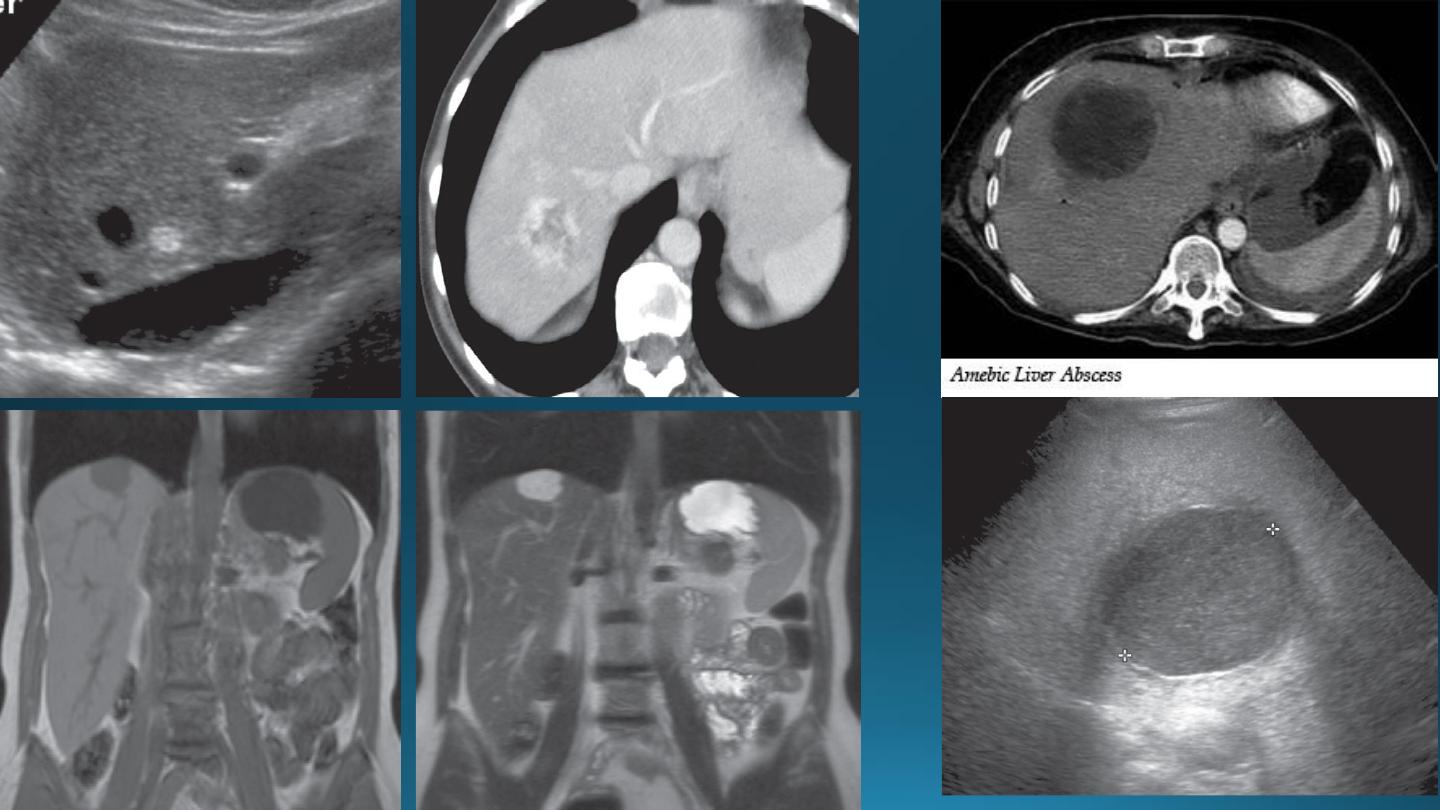
LIVER ABSCESS
It appears similar to cysts but have a thick irregular wall with fluid center.
Occasionally chronic abscess calcify.
It cannot be distinguished from necrotic tumor , but the clinical events should aid in the diagnosis.
Aspiration under US guidance is invariably undertaken.
ADENOMA
FOCAL NODULAR HYPERPLASIA
Both of these conditions appear as hypervascular masses on arterial phase, both on CT and MRI
CIRRHOSIS OF THE LIVER AND PORTAL HYPERTENSION
In
portal hypertension
, the pressure in the portal venous system is elevated due to obstruction of the blood flow in the
portal or hepatic venous system.
• Cirrhosis is the commonest cause.
• Occlusion of the hepatic veins (budd-chiari syndrome)
• Thrombosis of the portal vein following infection of the umbilical vein in neonates or secondary to acute pancreatitis
The signs of liver cirrhosis at CT and US are :
1. Reduction in size of the right lobe of the liver
2. Irregularity of the surface of the liver
3. Splenomegaly
4. Ascites
5. Coarse abnormal liver texture at US while at CT, the parenchyma appears normal until late in the disease.
• Patency of the splenic, portal & hepatic veins can be assessed with Doppler US, CT& MRI
•
For persistent bleeding varices, the percutaneous procedure known as TIPSS (transjugular intrahepatic
portosystemic shunt) can be undertaken
.
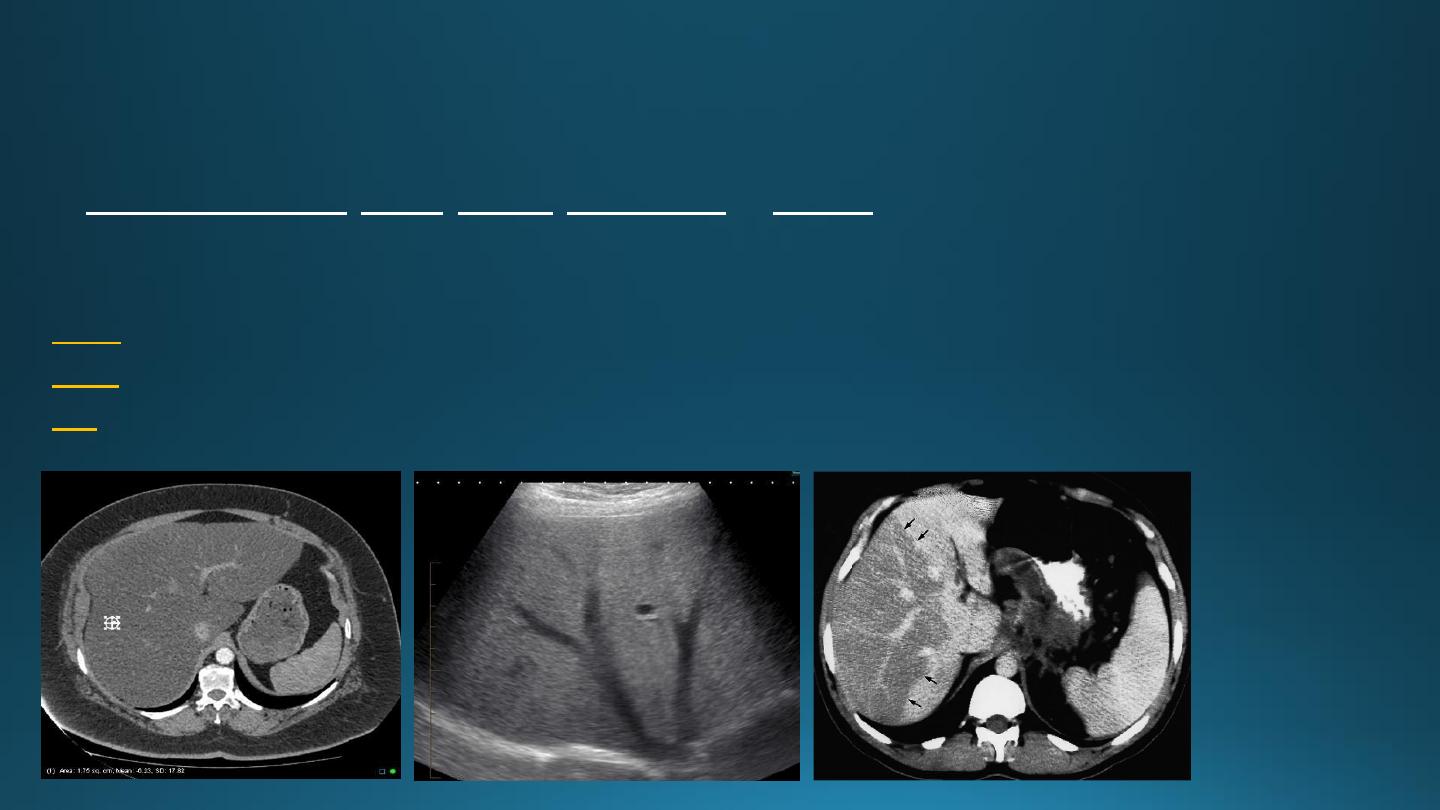
FATTY INFILTRATION OF THE LIVER
• It is a frequent finding
• Hypercholesterolaemia, obesity, diabetes, chemotherapy, or alcoholic.
• Focal or diffuse.
At CT,
liver density is less than splenic density
At US,
increased liver echogenicity (bright liver)
MRI
useful in problem cases because fat gives a characteristic set of signals
THE BILIARY SYSTEM
IMAGING TECHNIQUES:
ULTRASOUND
• Its is the initial simplest method for investigation.
• The patient is asked to fasting 6 hours to prevent GB contraction.
• The normal GB has a thin wall < 3 mm, and thickening of wall suggest cholecystitis.
• Stones > 2 mm can be identified.
• The normal CBD can be visualized in all patients and should not measure >7 mm unless the patient
done cholecystectomy when it may be larger.
• The lower end of CBD is often obscured by bowel gases.
• The normal intrahepatic tree is of such smaller caliber to be visualized by US.
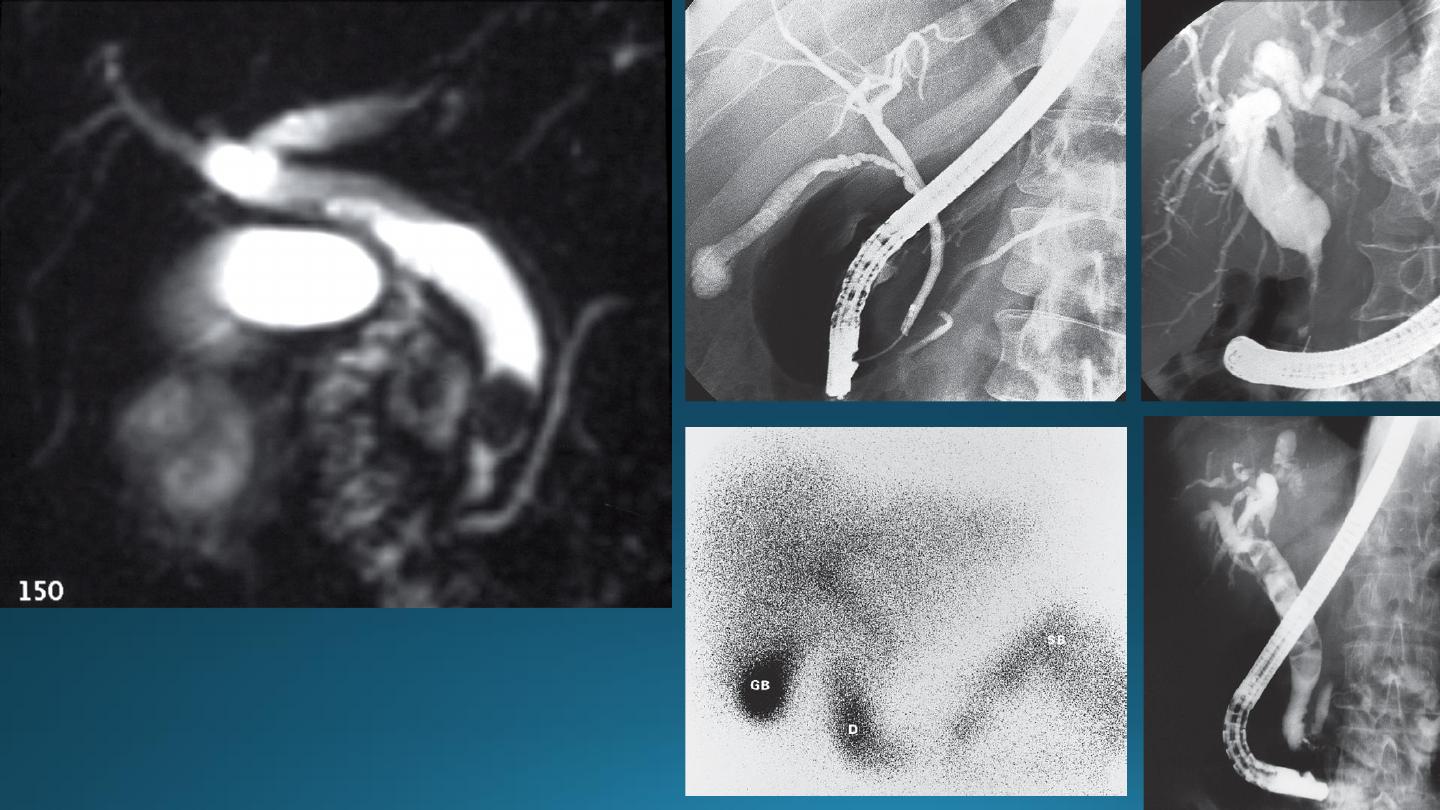
Magnetic Resonance Cholangiopancreaticography (MRCP)
• MRCP technique use heavily t2-weighted sequences.
• Bile and pancreatic ducts have high signal intensity.
• Unlike ERCP, it is non-invasive, does not require sedation and bowel intubation & no contrast agent used .
• ERCP is necessary for any endoscopic biopsy or treatment.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
Percutaneous Transhepatic Cholangiogram (PTC)
Hepatobiliary Radionuclide Scanning
(e.g. biliary atresia, leakage)
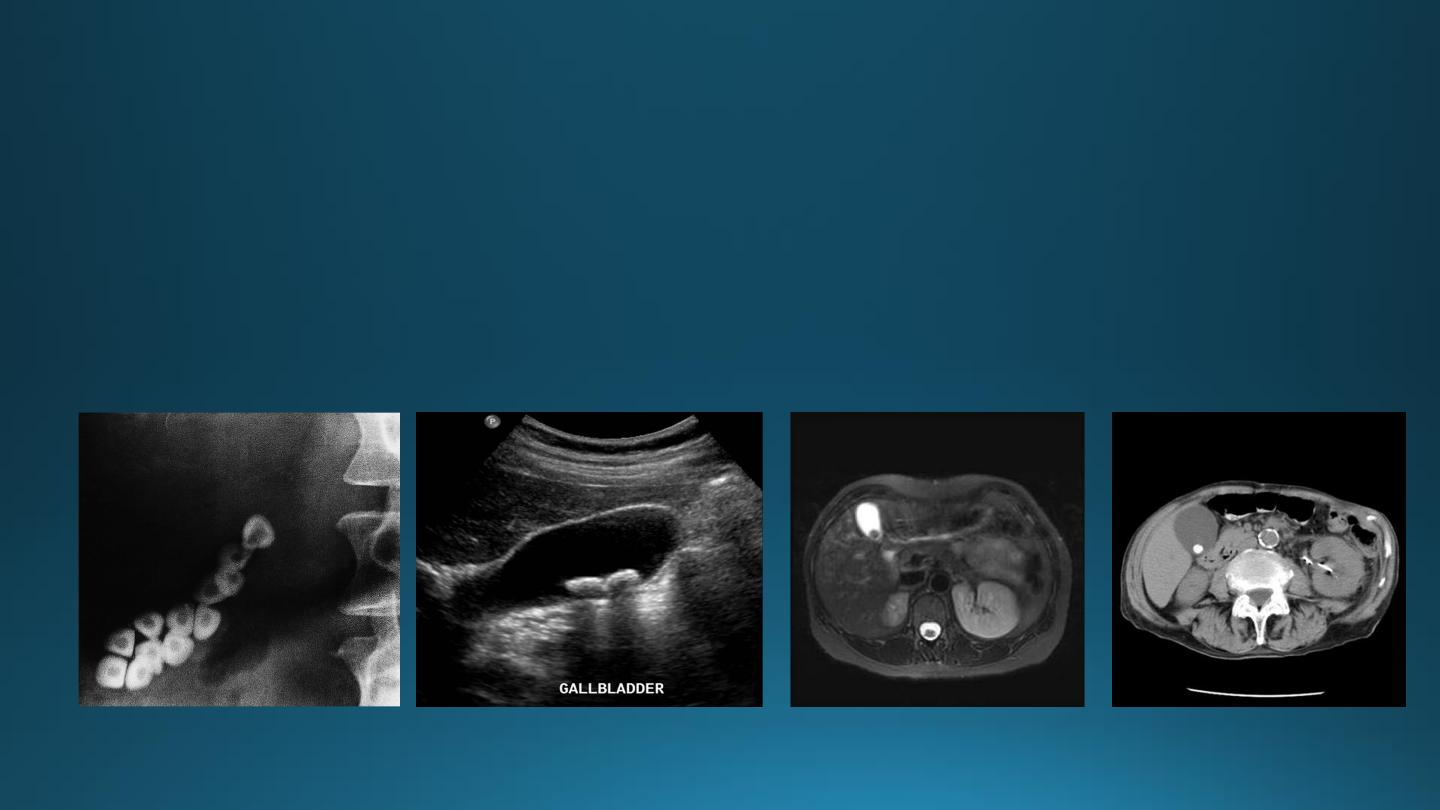
GALL STONES
• Gall stones are more frequent in middle age females.
• 20% of gall stones are visible on plain film.
• On US, stones are strongly echogenic with acoustic shadow (which is not seen with polyps).
• US is not reliable for detecting stones in CBD which are better demonstrated by MRCP
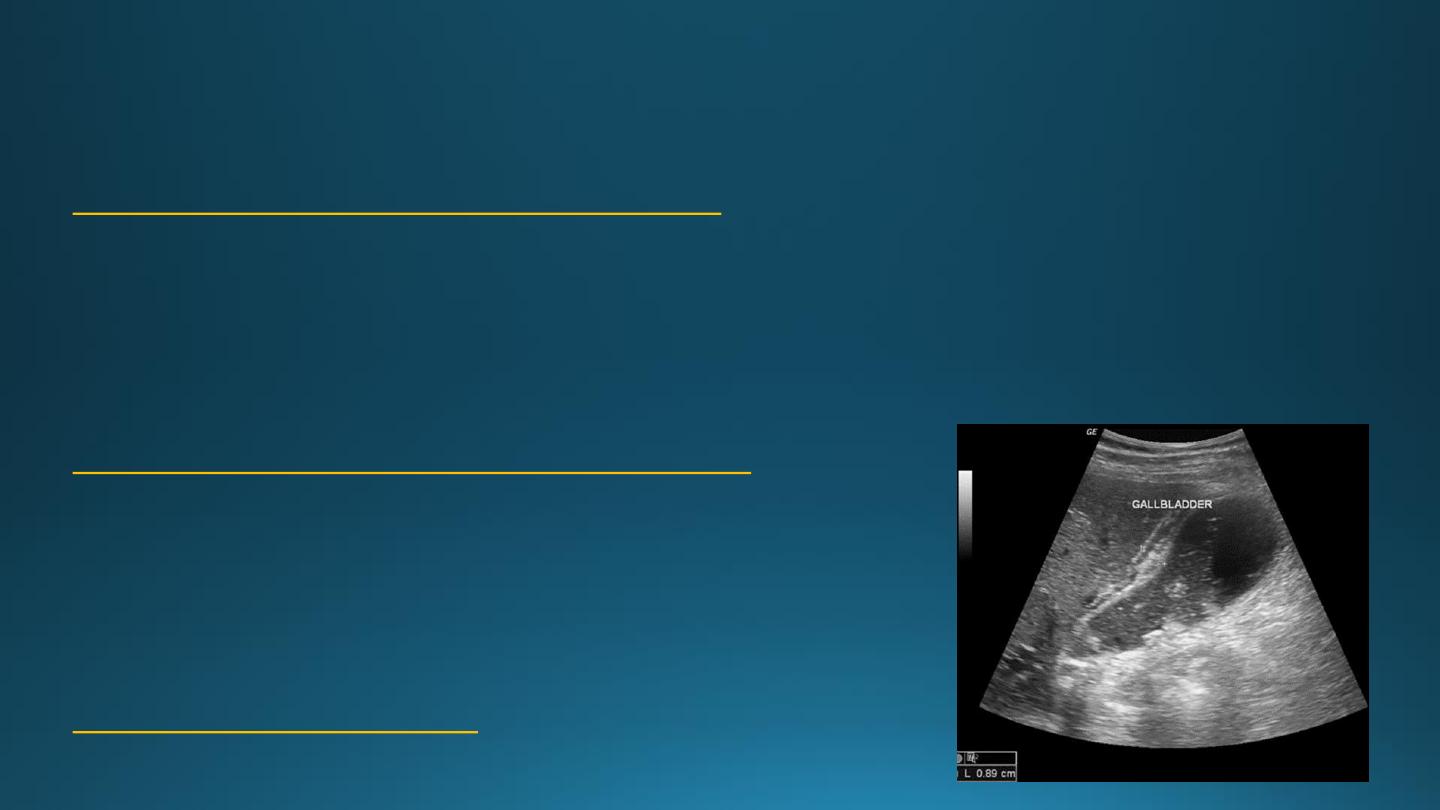
CHOLECYSTITIS
US features of early or uncomplicated acute cholecystitis:
1. Gall stones (which may be impacted in the GB neck or cystic duct)
2. Gall bladder wall thickening
3. Gall bladder distension
4. Positive sonographic Murphy's sign (focal tenderness over the GB when compressed by the US transducer)
US features of advanced or complicated acute cholecystitis:
1. Pericholecystic fluid collection
2. Striated appearance of the thickened GB wall
3. Intraluminal membranes caused by sloughed GB mucosa
4. Gas in GB wall or lumen resulting in emphysematous cholecystitis
US features of chronic cholecystitis
are thick wall and GB contraction
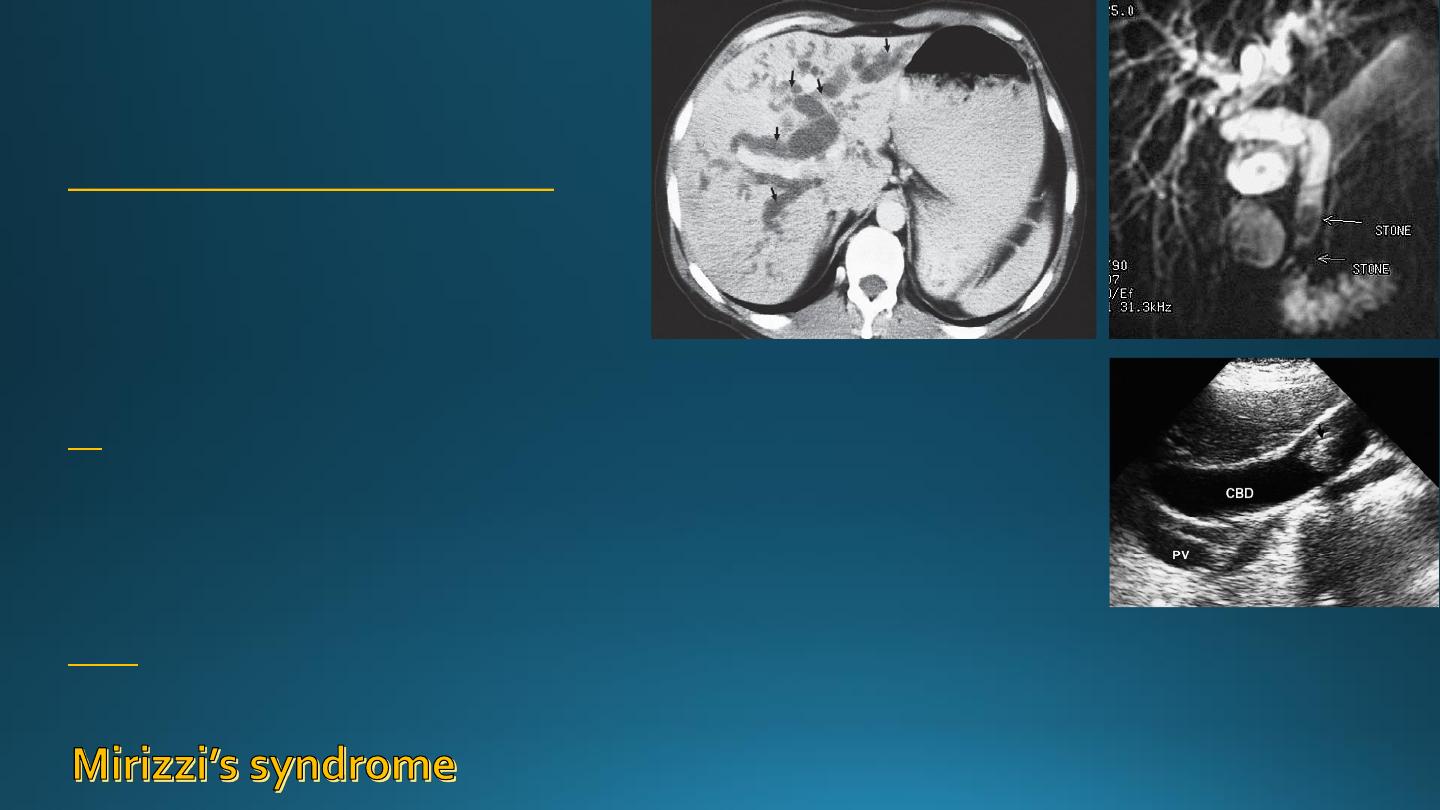
BILIARY OBSTRUCTION
Common causes of biliary obstruction are :
1. Impacted stone in CBD
2. Carcinoma of the head of pancreas
3. Carcinoma of the ampulla of vater
4. Cholangiocarcinoma
US
• Its the first test to be performed in obstructive jaundice.
• Us can show dilated ducts & can demonstrate the level of obstruction.
• Sometimes the specific cause of biliary obstruction e.g. stone or pancreatic head
tumor.
MRCP
is often more helpful than CT in cases of suspected CBD stones or biliary
stricture.

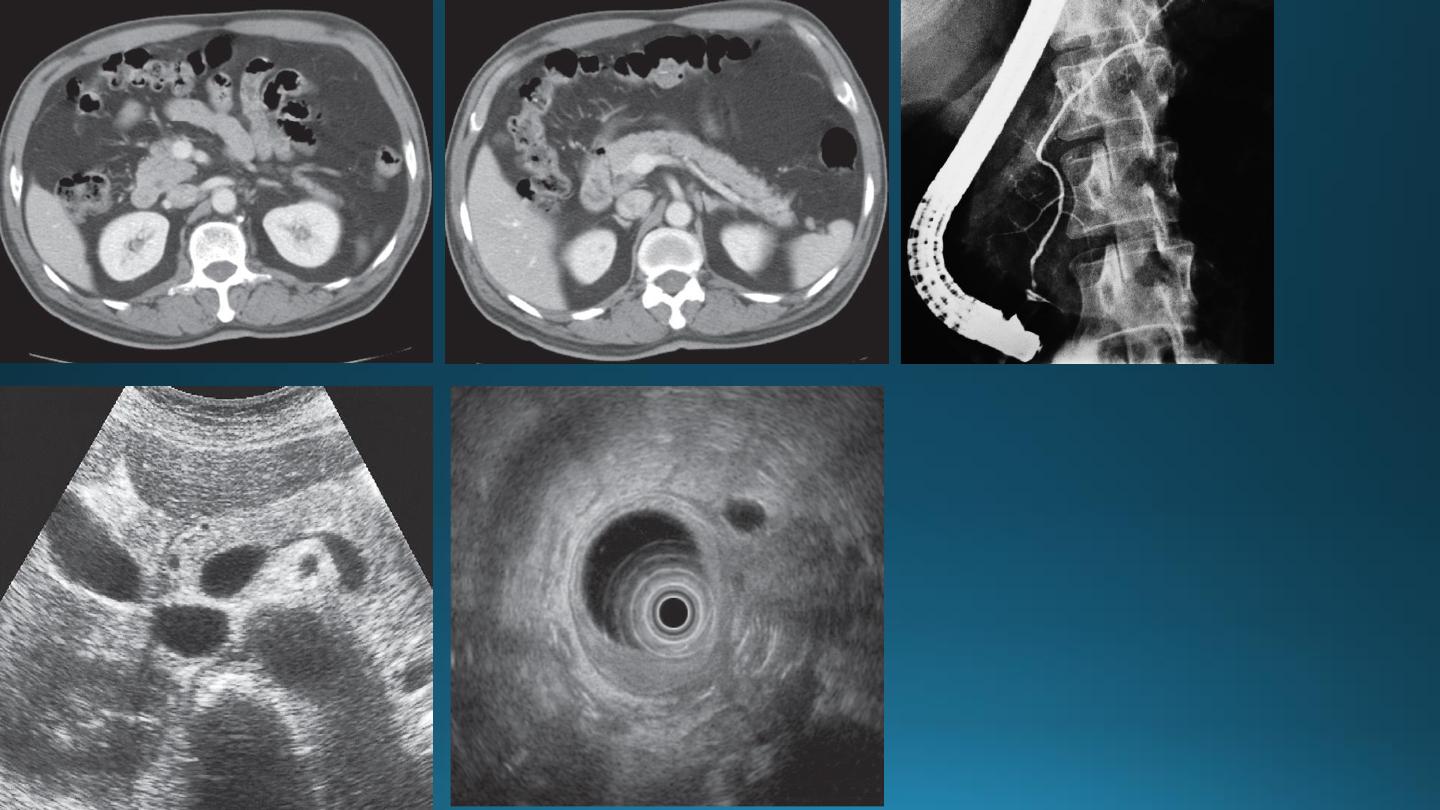
PANCREAS
CT
is the main stay for imaging of the pancreas, regardless of the amount of bowel adjacent to it.
US
limited by the gas in the GIT.
EUS
staging of pancreatic tumor.
MRCP
ERCP
• The normal pancreas is an elongated retroperitoneal organ surrounded by a variable amount of fat.
• The head is visualized to best advantage when the duodenum is opacified with oral contrast.
• The body of the pancreas lies in front of the SMA and V.
• The tail situated near the hilum of the spleen.
• The splenic vein lies behind the body, it join the SMV at the neck of the pancreas to form the portal vein.
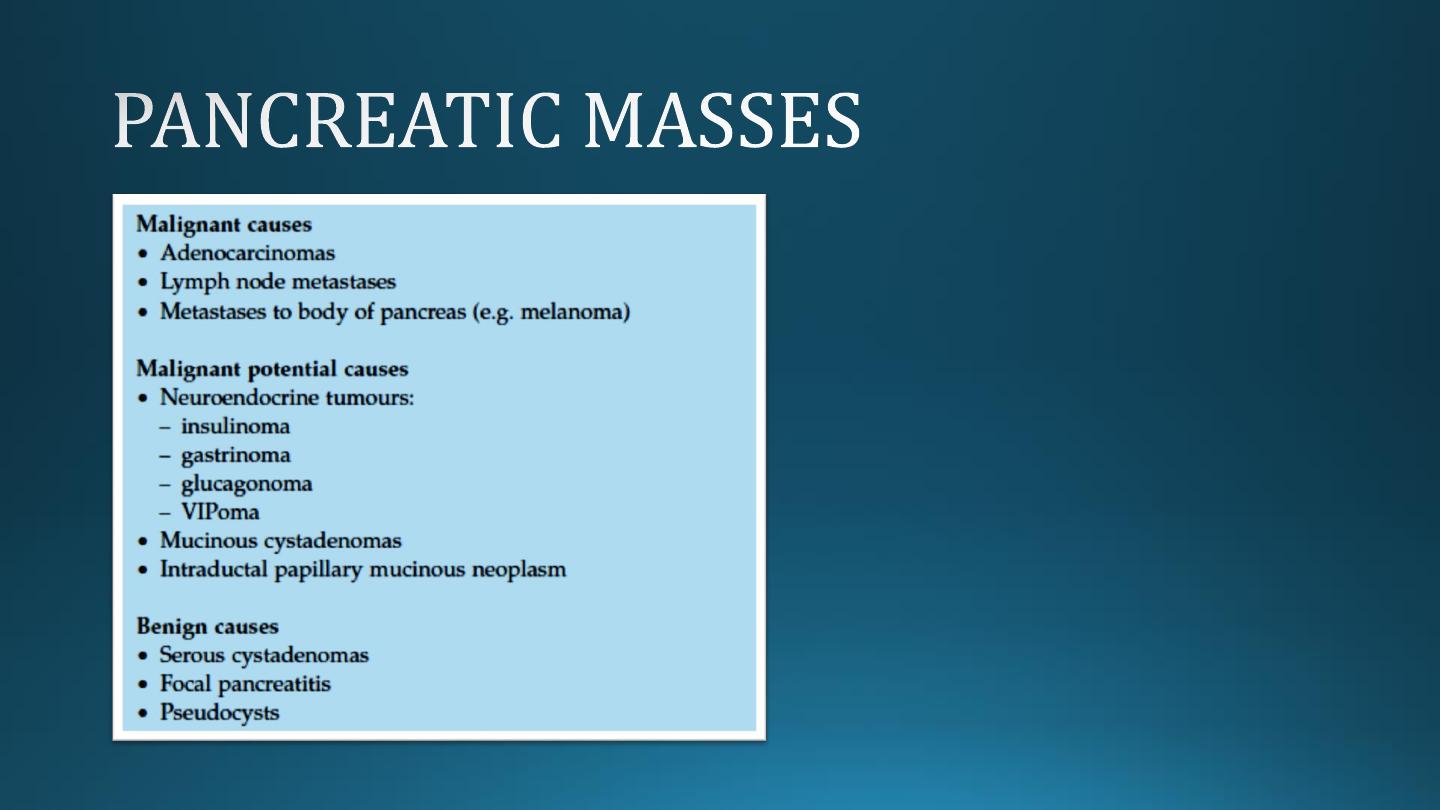
PANCREATIC ADENOCARCINOMA
• It locate in head of pancreas in 2/3 cases.
• It obstruct CBD even with small lesions giving rise to jaundice.
• Tumors in the body or tail become large until giving rise to symptoms.
• The important sign of carcinoma at both CT and US is a focal mass within or deforming the outline of the gland.
• On contrast-enhanced CT, the tumor appears of lower density compared to the normal pancreatic tissue.
• The main pancreatic duct may be dilated distal to an obstructing mass .
• Most tumors are irresectable at time of diagnosis because of involvement of regional LAP, liver metastases and
regional vascular encasement.

ACUTE PANCREATITIS
The pancreas is usually enlarged, often diffusely with irregular outlines due to extension of inflammatory process
into the surrounding fat. There may be low density areas at CT or echo-poor areas at US (edema and necrosis)
The diagnosis is usually made on clinical and biochemical grounds
The purpose of CT is to assess the severity and complications:
1. Pancreatic necrosis (areas with no enhancement)
2. Abscess appear as fluid collection which may contain gas
3. Vascular complications e.g. Splenic vein thrombosis, arterial erosion & pseudoaneurysm
4. Pseudocysts occur as a result of leak of pancreatic secretions that are contained in a cyst like manner within
and adjacent to the pancreas.
They can be demonstrated with CT or US as thick or thin walled cysts of variable sizes.
Many pseudocysts resolve in the weeks following an attack of acute pancreatitis, some persist and may need
surgical or percutaneous drainage.
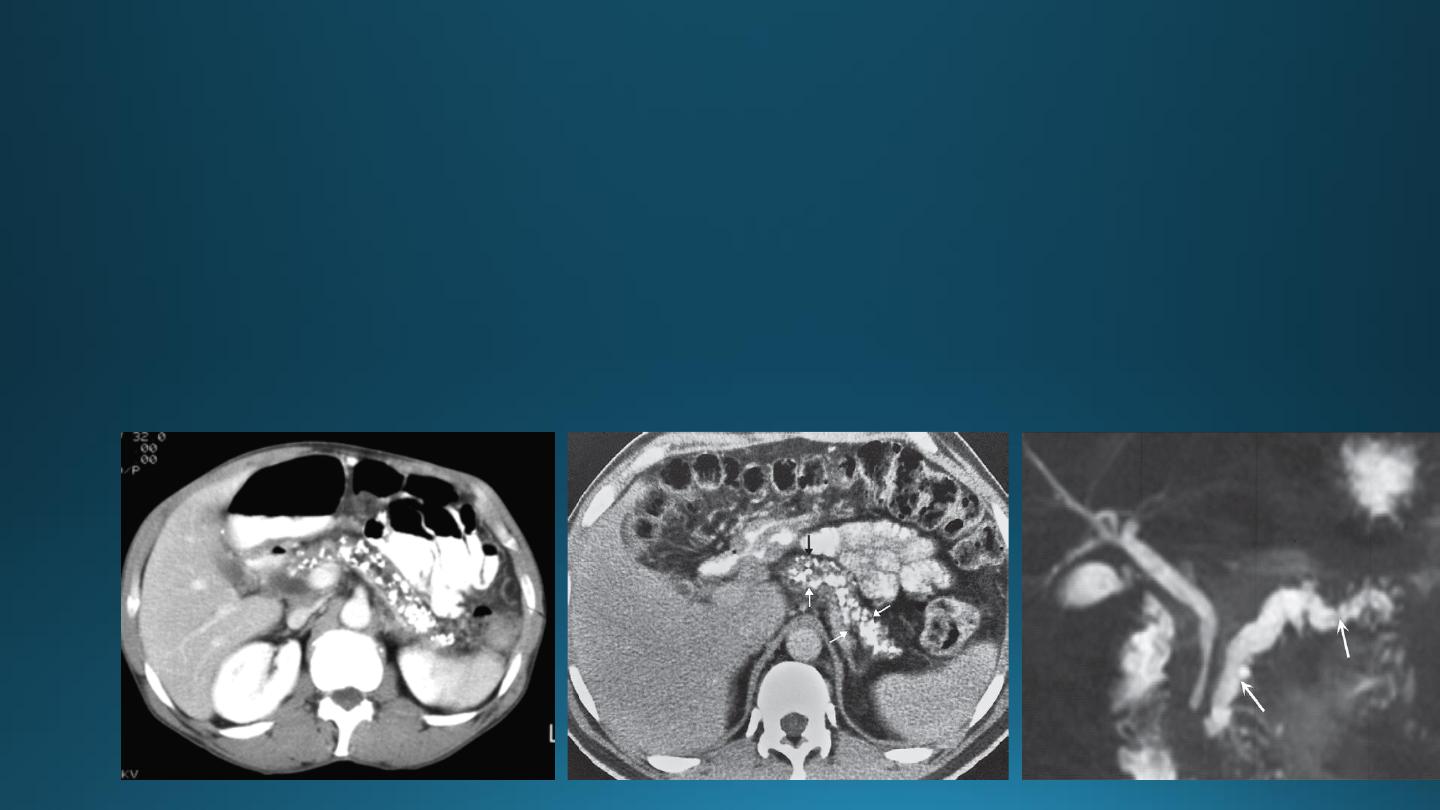
CHRONIC PANCREATITIS
• It result in fibrosis, calcifications, and ductal stenosis and dilatation.
• Pseudocysts are seen.
• The calcification often recognizable on plain x ray film, but more obvious on CT.
• The gland may enlarge focally or generally.
• The gland may atrophied.
• The pancreatic duct may be enlarged and irregular.
SPLEEN
• The commonly encountered
splenic masses
are cysts, including hydatid cysts, abscesses, and tumors.
• Lymphoma is much commoner than metastases, which are rare in the spleen.
Causes of splenomegaly
include lymphoma, portal hypertension, chronic infection and various blood disorders.
Splenic infarction
• Secondary to severe pancreatitis
• Pancreatic carcinoma
• Sickle cell and trauma
It show focal or complete loss of normal enhancement following IV contrast
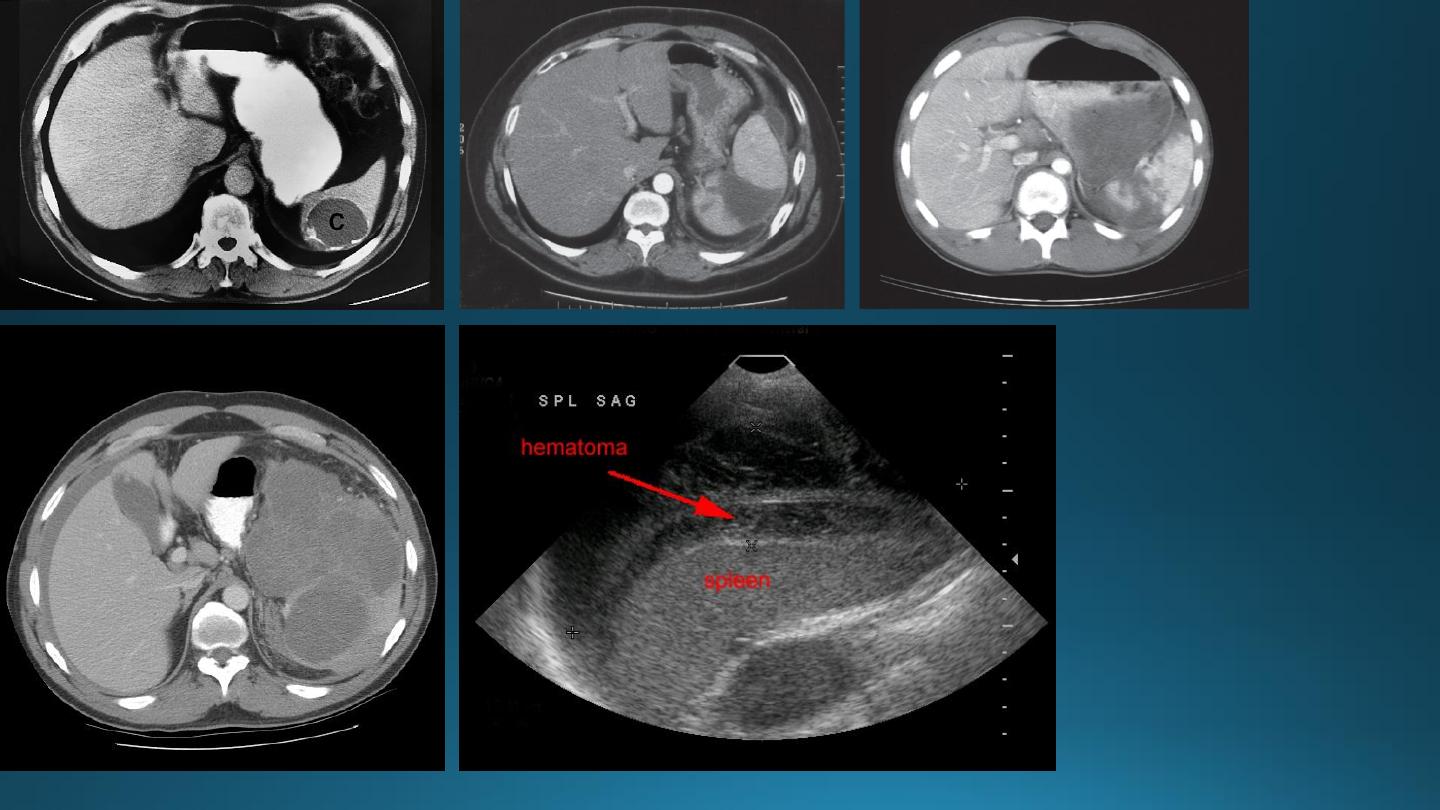
Splenic trauma
• The spleen is the most commonly injured organ in blunt trauma.
• CT is the superior method of investigation.