METABOLIC BONE DISEASE
Dr.Ahmed SaiedMBChB FIBMS
General
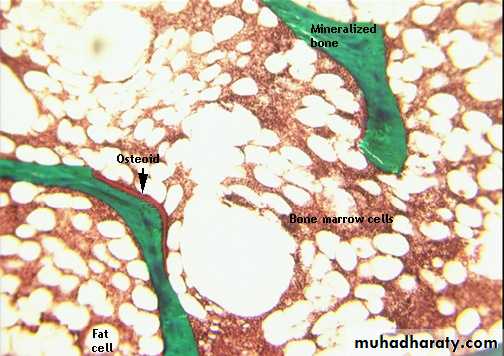
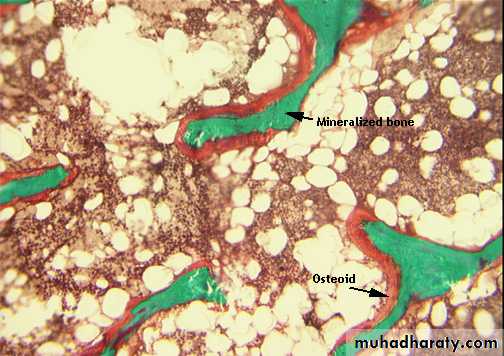
Bone tissue consists of:Extracellular substance
* Osteoid: collagen, mucopolysaccharide
* Crystalline component: calcium phosphate, hydroxyapatiteCells
* Osteoblasts
* Osteoclasts
Bone is constantly absorbed and replaced with new bone.
Disturbances in this equilibrium result in either too much bone (increased radiodensity, osteosclerosis) ortoo little bone (decreased density = osteopenia).
OSTEOPENIA
Osteopenia is a nonspecific radiographic finding that indicates increased radiolucency
of bone. Bone density may be difficult to assess because of technical factors (kVp, mA)that influence the radiographic appearance.
Types
1- Osteoporosis: decreased amount of normal bone2- Osteomalacia: decreased bone mineralization
3- Marrow replacement: bone replaced by tumor, marrow hyperplasia,or
Metabolic products
4- Hyperparathyroidism: increased bone resorption
• Specific radiographic clues
• Disorder• Looser zones
• osteomalacia
• subperiosteal resorption
• hyperparathyroidism
• focal lytic lesions
• disseminated multiple myeloma
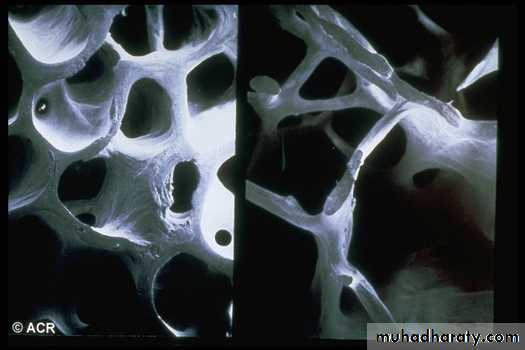
OSTEOPOROSIS
Classification
Primary osteoporosis (most common): unassociated with an underlying illness
* Type I osteoporosis: postmenopausal
* Type II osteoporosis: senile
-Idiopathic juvenile osteoporosis
Secondary osteoporosis (less common)
1- Endocrine disorders(Hypogonadism , Hyperthyroidism, Cushing's disease, Acromegaly, Nutritional, Malabsorption syndromes, Alcoholism, Scurvy.2- Hereditary metabolic or collagen disorder
(Osteogenesis imperfecta, Marfan syndrome, Ehlers-Danlos syndrome, Homocystinuria, Hypophosphatasia, Wilson's disease, Alkaptonuria, Menkes' syndrome)3- Drugs (Heparin
Exogenous steroidsRadiographic features
* Osteopenia: 30%-50% of bone has to be lost tobe detectable by plain film
* Diminution of cortical thickness: width of both
MCP cortices should be less than half the shaft
diameter
* Decrease in number and thickness of trabeculae
in bone
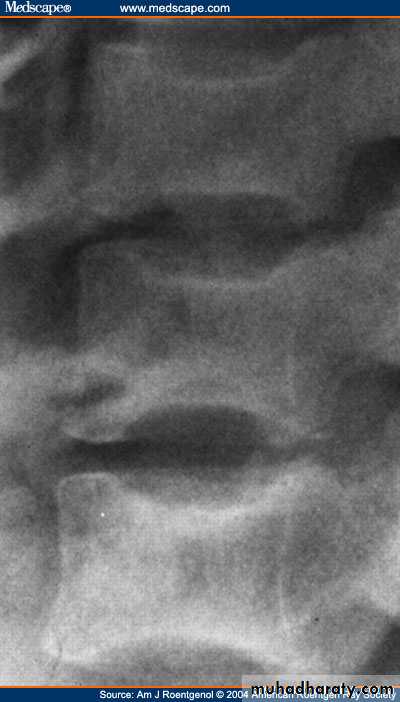
Vertebral bodies show earliest changes:
resorption of horizontal trabeculae
Empty box vertebra: apparent increased density of vertebral endplates due to resorption of spongy bone
Vertebral body compression fractures: wedge, biconcave codfish bodies, true compression
* Pathological fractures
Qualitative assessment:
Singh index is based on trabecular pattern of proximal femur.Patterns:
1-Mild: loss of secondary trabeculae
2-Intermediate: loss of tensile trabeculae
3-Severe: loss of principal compressive trabecular
Quantitative bone densitometry
Predicts the risk for developing fractures
3 methods are available:
* Single-photon absorption
Measures cortical bone density of radial shaft
* Dual-photon absorption with radionuclide or dual-energy
x-rayMeasures vertebral and hip
Quantitative CT with phantom Measures vertebral body density (trabecular only)
Most effective technique for evaluation of bone density
Indications for measurements:
Initiation of estrogen replacement therapy or phosphonate therapy* Establish diagnosis of osteoporosis
* Assess severity of osteoporosis
*Monitor treatment efficacy
OSTEOMALACIA
Abnormal mineralization of bone is termed Osteomalacia in adults and rickets in children.In the past, the most common cause was deficient intake of vitamin D.
Today, absorption abnormalities and renal disorders are more common causes.
Nutritional deficiency of:
*Vitamin D * Calcium * PhosphorusAbsorption abnormalities
*Gastrointestinal (GI) surgery
* Malabsorption
*Biliary disease
Renal
*Chronic renal failure *Renal tubular acidosis *Proximal tubular lesions * Dialysis induced
Abnormal vitamin D metabolism
*Liver disease * Hereditary metabolic disorders
Drugs
* Dilantin * Phenobarbitol
Rickets
Normal
Osteomalacia
Normal Osteoporosis
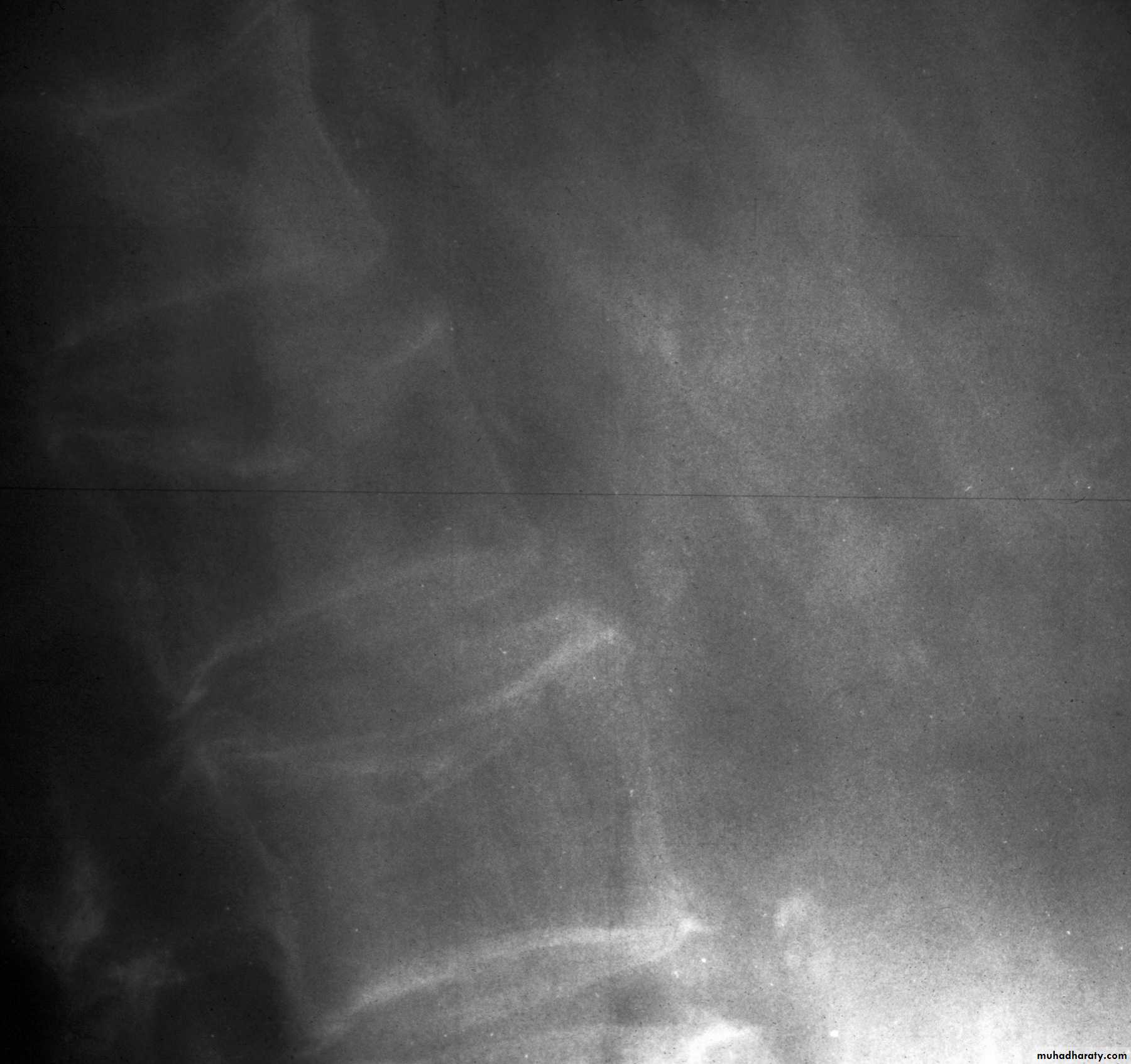
AP view looser’s zone
frogleg view looser’s zone
Osteomalacia: Bone scanRadiographic features
1-Generalized osteopenia2-Looser's zones (pseudofractures):
cortical stress fractures filled with
poorly mineralized osteoid tissue.
* Milkman's syndrome: osteomalacia
with many Looser's zones
Typical location of Looser's zones
(often symmetrical)
Axillary margin of scapula
Inner margin of femoral neck
Rib
Pubic, ischial rami
* Osteomalacia may be indistinguishable from osteoporosis; however, Looser's
zones are a reliable differentiating feature.
RENAL OSTEODYSTROPHY
Renal osteodystrophy is a general term that refers to a myriad of radiographic
osseous changes in patients with renal failure.
Radiographically, these changes are
secondary to osteomalacia, secondary hyperparathyroidism, and aluminum intoxication.
Radiographic features
-Changes of osteomalaciaOsteopenia and cortical thinning
Looser's zones occur but are uncommon
-Changes of hyperparathyroidism
* Subperiosteal resorption (e.g., SI joint resorption)
* Rugger jersey spine
* Brown tumors
* Osteosclerosis
* Soft tissue calcification &Chondrocalcinosis
HYPERPARATHYROIDISM (HPT)
Parathyroid hormone stimulates osteoclastic resorption of bone. HPT is usually detected by elevated serum calcium during routine biochemical screening.Three
types:
Primary HPT:
Adenoma, 85% (single 90%, multiple 10%)
Hyperplasia, 12%
Parathyroid carcinoma, 1%-3%
Secondary HPT: most often secondary to renal failure; rarely seen with ectopic
parathyroid production by hormonally active tumor
Tertiary HPT: results from autonomous glandular function following
longstanding renal failure
Radiographic features:
Clavicuiar lysis, Subperiosteal resorption
Brown tumors ,General osteopenia
(Bone resorption is virtually pathognomonic(Subperiosteal resorption
Radial aspect of middle phalanges
(especially index and middle finger)
Phalangeal tufts
Trabecular resorption
Salt and pepper skull
Cortical resorption
Tunneling of MCP bones (nonspecific)
Subchondral resorption
Widened SI joint
Distal end of clavicle
Widened symphysis pubis
Can lead to articular disease
Brown tumors (cystlike lesions) may be found anywhere in the skeleton but
especially in the pelvis, jaw, and femur.
0 Loss of the lamina dura
Soft tissue calcification
Chondrocalcinosis
0 Complication: fractures
Hyperparathyroidism
Xrays:
sub-periosteal resorptionpepper pot skull
rugger jersey spine
cystic brown tumours
Hyperparathyroidism
Xrays:sub-periosteal resorption
pepper pot skull
rugger jersey spine
cystic brown tumours
Hyperparathyroidism
Xrays:sub-periosteal resorption
pepper pot skull
rugger jersey spine
cystic brown tumours
Hyperparathyroidism
Xrays:sub-periosteal resorption
pepper pot skull
rugger jersey spine
cystic brown tumours
Hyperparathyroidism
Xrays:sub-periosteal resorption
pepper pot skull
rugger jersey spine
cystic brown tumours
Marrow Disease
CLASSIFICATION
Malignant infiltration
* Myeloma
* Leukemia/lymphoma
*Metastases (small cell tumors)
Secondary marrow hyperplasia
*Hemoglobinopathies
*Hemolytic anemias
Lysosomal storage diseases
* Gaucher's disease
*Niemann-Pick disease
SICKLE CELL ANEMIA
Structural defect in hemoglobin (hemoglobin S; point mutation). Most hemoglobinopathies(over 250 are known) result in rigid hemoglobin and hemolysis.
Incidence: 1% of blacks. Diagnosis is confirmed by hemoglobin electrophoresis. Sickle
cell disease (IlbSS) has many bone findings, whereas sickle cell trait (HbAS) is only
occasionally associated with bone infarcts. Hemoglobin sickle cell disease has same
bone findings but the spleen is enlarged.
Radiographic features
Hyperplasia of marrow
* Hair-on-end appearance of skull
Pathological fractures
@ Biconcave H-shaped vertebra
Q Osteopenia
! Vascular occlusion
AVN occurs primarily in medullary space of long bones, hands, growing
epiphyses
* Bone sclerosis from infarctions
* H-shaped vertebral bodies
involvement of growing epiphyses leads to growth disturbances
* Dactylitis (hand-foot syndrome): bone infarcts of hands and feet
Osteomyelitis
I * High incidence: most are caused by Staphylococcus
Salmonella infection more common than in general population
Most commonly at diaphysis of long bones
Osteomyelitis and infarction may be difficult to distinguish.
* Small calcified fibrotic spleen due to autoinfarction
* Cholelithiasis
* Progressive renal failure
Papillary necrosis
* Cardiomegaly: high output congestive heart failure (CHF)
Pulmonary infarcts
Plain radiography. Anterior-posterior view of bilateral knees. Note the irregular areas of lacy and serpentine calcific deposits in bilateral distal femurs and proximal tibias typical for bone infarcts.
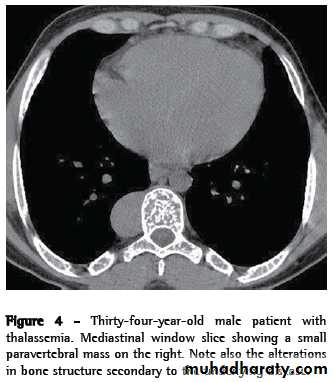
THALASSEMIA (COOLEY'S ANEMIA)
Genetic disorder characterized by diminished synthesis of one of the globin chains.Radiographic features
Hyperplasia of marrow is the dominant feature.* Expands the marrow space: hair-on-end skull
* Modeling deformities of bone: Erlenmeyer flask deformity
* Premature closure of growth plates
* Paravertebral masses due to extramedullary hematopoiesis
Vascular occlusion
* Scattered bone sclerosis
* H-shaped vertebral bodies
* AVN less common than in sickle cell
Other
* Cardiomegaly and CHF
* Secondary hemochromatosis
Cholelithiasis
THALASSEMIA (COOLEY'S ANEMIA)
Genetic disorder characterized by diminished synthesis of one of the globin chains.Radiographic features
Hyperplasia of marrow is the dominant feature.* Expands the marrow space: hair-on-end skull
* Modeling deformities of bone: Erlenmeyer flask deformity
* Premature closure of growth plates
* Paravertebral masses due to extramedullary hematopoiesis
Vascular occlusion
* Scattered bone sclerosis
* H-shaped vertebral bodies
* AVN less common than in sickle cell
Other
* Cardiomegaly and CHF
* Secondary hemochromatosis
Cholelithiasis