د.احمد دلالي باشي كيمياء حياتية 15\11\2017
عدد الاوراق ( 17 ) م\2\موصل lec: 1Titles of subjects in lecture 5
LIPID METABOLISMIntroduction:
Classification of Lipids:
I. Simple lipids:
a. Fats and oils
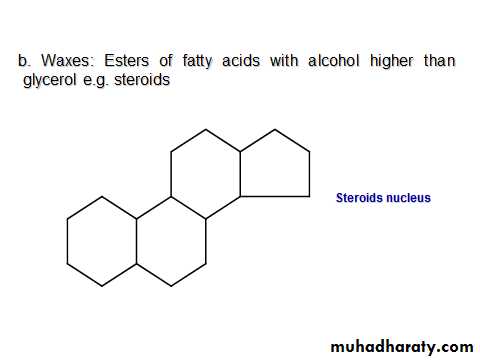
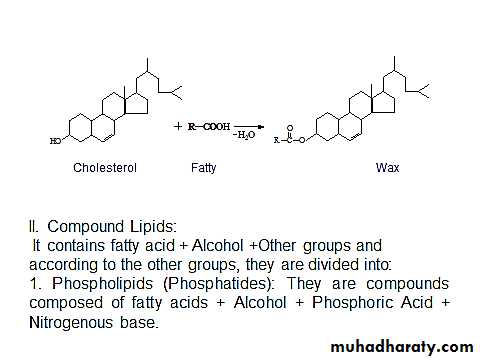
b. Waxes:
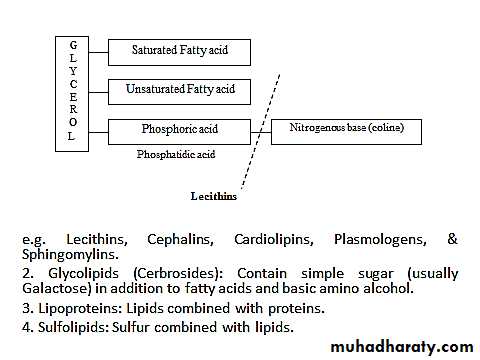
II. Compound Lipids:
III. Derived lipids:
LIPID METABOLISM
Introduction:LIPIDS:
The lipid is one of the three major constituents of the diet (Lipids, Carbohydrates & proteins).
It is primarily composed of C, H, & O in a ratio, which differ than in carbohydrates and in proteins.
They contain in their structure the fatty acids, which are organic acids of high molecular weight.
They have the common property of being insoluble in water and soluble in non-polar solvents e.g.
chloroform,
benzene,
ether, etc.
Lipids are important dietary constituent due to their high-energy value (1 g =9.1 kcal)
and due to the presence of fat-soluble vitamins
(Vit. A, D, E & K) and
Due to the presence of essential fatty acids in the natural food.
Classification of Lipids:
G
L
Y
C
E
R
O
L
Fatty acid
Fatty acid
Fatty acid
GL
Y
C
E
R
O
L
Fatty acid
Fatty acid
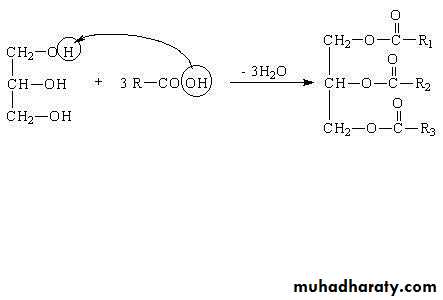
Fatty acidI. Simple lipids: They are esters of fatty acids and one of the various alcohols. They are divided into:
Fats and Oils: Esters of Fatty acids and glycerol.
CH2-OH
CH-OH
CH2-OH
Glycerol
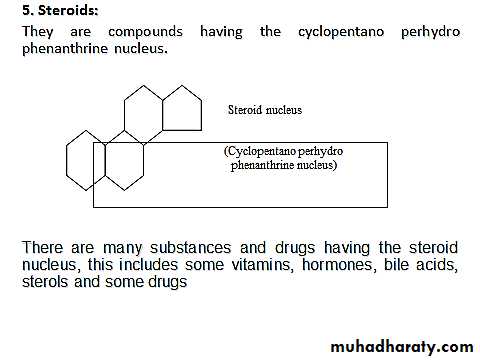
III. Derived lipids:
These include substances derived from the above groups by hydrolysis.This includes fatty acids (Saturated and unsaturated), Glycerol, steroids, alcohol in addition to fatty aldehydes & keton bodies.
Review of certain points in chemistry of lipids:
1. Saturated and unsaturated fatty acids:Saturated fatty acids have the general formula CnH2n+1COOH.
They contain no double bonds in their structure e.g.
Butyric acid -------------- C3H7COOH
Palmitic acid -------------- C15H31COOH
While the unsaturated fatty acids are characterized by the presence of one or more double bonds in their structure. They have the general formula CnH2n-1COOH (If one double bond) e.g.
Palmitoleic acid C15H29COOH.
If two double bonds CnH2n-3COOH.
If three double bonds CnH2n-5COOH. And so on.
The carbon atoms are numbered from the carboxylic carbon as no.1. The carbon atom adjacent to the carboxyl carbon as no.2 also known as α-carbon, No.3 is β & so on e.g.
3 2 1
CH3-CH2-…………..CH2 – CH2 – COOH
β α
2. Fats and Oils:
Fats are solid at room temperature, while oils are liquid at room temperature.
This is because fats contain saturated fatty acids while oils contain unsaturated fatty acids.
They are stored in the adipose tissues & serve as energy stores in addition they form an isolating layer in the subcutaneous tissues also surrounding certain vital organs to protect them from damage.
Glycerol Fatty acids Triglyceride or Triacyl glycerol (Fats and oils)
3. Essential Fatty acids:
They are:Lenoleic acid
Lenlenic acid &
Arachidonic acid
They are called essential as the body can not synthesis them and are required to be taken with food.
They are characterized by the presence of two or more double bonds in their structure; they were also called Vitamin F.
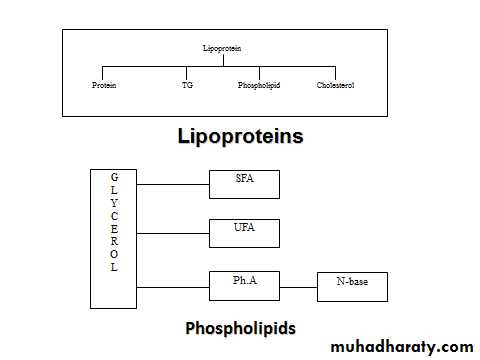
4. Lipoproteins:
They are chemical combinations between lipids and proteins in order to convert the fatty acids and cholesterol, which are insoluble in aqueous medium to soluble one,
due to the presence of hydrophilic groups in the protein.
Lipoproteins are important cellular constituents of the cell membrane and intracellular membrane e.g. nucleus and mitochondria.
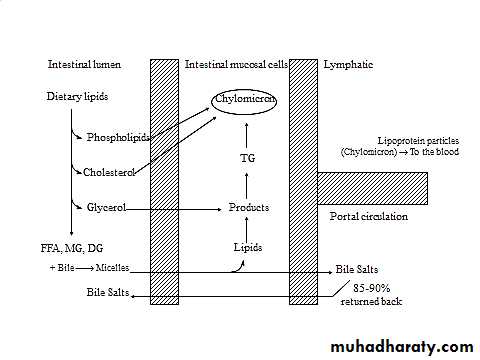
DIGESTION AND ABSORPTION OF LIPIDS
-The lipids of the diet are usually a mixture of different types of lipids, however the bulky of that are the triglycerides. Other types include Phospholipids, Cholesterol, FFA etc…-The lipids are hydrolyzed by lipase an enzyme usually presents in the intestinal lumen.
So the lipids are hydrolyzed or digested mainly in the intestinal lumen which contains the pancreatic and intestinal lipase.
-In the mouth there is no digestion of lipids. Also no digestion in the stomach.
Lipase may be found in small amount in the stomach and this is come from the regurgitation of pancreatic juice.Lipase in the stomach is usually inactive due to acidic medium of the stomach (pH1-2) while the optimum pH of lipase is around pH 8.
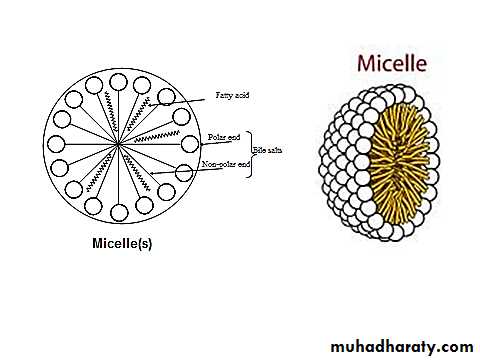
-Bile salts:
Bile salts are very necessary for the digestion and absorption of lipids in the small intestine.
Bile salts are mainly sodium and potassium salts of Cholic acid, Chenodeoxycholic acid, Glycocholic acid & Taurocholic acid in addition to small amount of other types.
Bile salts are synthesized in the liver and stored in the gall bladder. There are two main functions of bile salts these are:
1. Digestion of lipids:
Bile salts have important role in the digestion of lipids they act by emulsification of the lipids in the intestine.
The mechanism for this action is by decreasing the surface tension of water or aqueous medium so the fatty molecules will be divided into small particles and spread between the aqueous molecules, so the surface area of lipids increase.
This will help lipase to interact more closely with lipids.
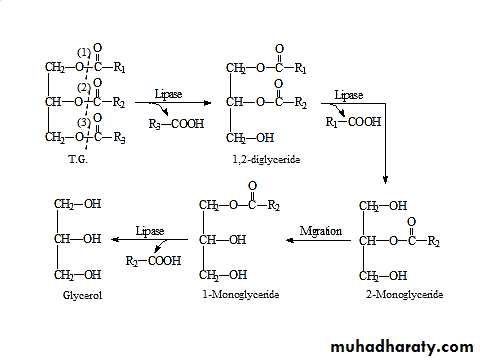
Lipase hydrolysis the finely divided fat globules by hydrolyzing the ester bond in the triglyceride.
Lipase acts specifically on ester linkage No.1& No.3, while No.2 is slowly hydrolyzed. Migration of fatty Acyl residue from position 2 to position 1 is usually occurring before hydrolysis.
The hydrolysis products in the intestinal lumen of triglycerides are glycerol, fatty acids, monoglycerides, diglycerides, some times even triglycerides are present in addition to phospholipids and cholesterol.
2. Absorption of lipids:
The above substances are present in the intestinal lumen. Some of them can pass to the intestinal mucosal cells while most of the other can not passes unless changed into certain manner to be easily move in aqueous medium.
This happen by combination with bile salts forming micelles in which the outer ends are the Polar parts and the non-polar ends are to the inside of the micelles , in between them the products of fat hydrolysis usually situated.
This is the mechanism for lipids products in which they passes to the intestinal mucosal cells where the uncompleted lipids digestion is completed and 85-90% of the bile will return back through the portal circulation to the liver.
Portal circulation or Hepatic portal circulation:
Blood flow from the abdominal organs that pass through the portal vein and hepatic vein then to the inferior vena cava before returning to the heart.
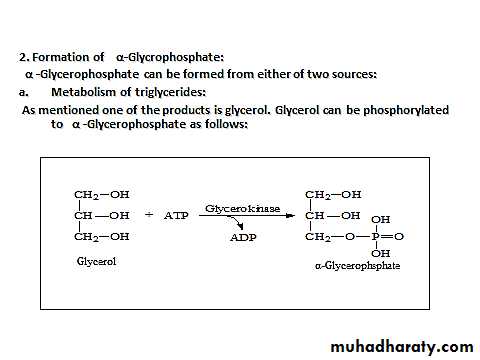
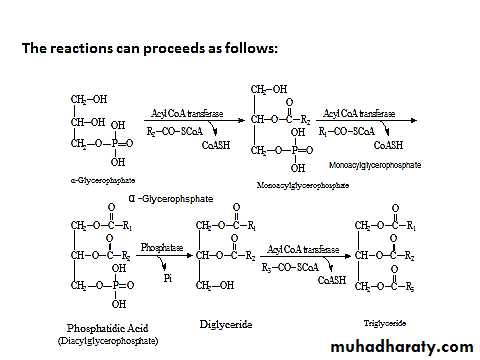
In the intestinal mucosal cells, resynthesis of triacyl glycerol (Triglyceride) will occur using glycerol or acylglycerol & the free fatty acids.
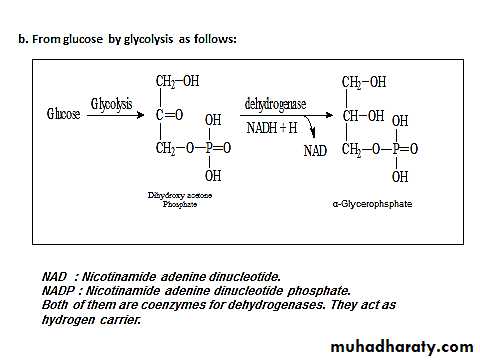
Any excess of fatty acids if present are esterified with α-Glycerophosphate which are produced during glycolysis.
The resynthesised triglyceride together with phospholipids and cholesterol passes into the lymphatic of the abdominal cavity combined with protein then to the blood through the thoracic duct and detected in the blood as lipoprotein particles called chylomicrons.
(Protein from the lymphatic or from the diet).
Absorption of fat-soluble vitamins:
The absorption of fat soluble vitamins (A, D, E& K) depend on the presence of bile forming micelles as mentioned in the absorption of fat.Hence, any defect or obstruction in the flow of bile, as well as any defect in fat digestion or absorption will lead to excrete the lipids as well as the fat soluble vitamins in the stool and result in steatorrhea (Excretion of lipids) and deficiency of fat soluble vitamins .
Lipoproteins:
The pure lipids are insoluble in water; however, they are largely transferred within the body by the blood, which is an aqueous medium.
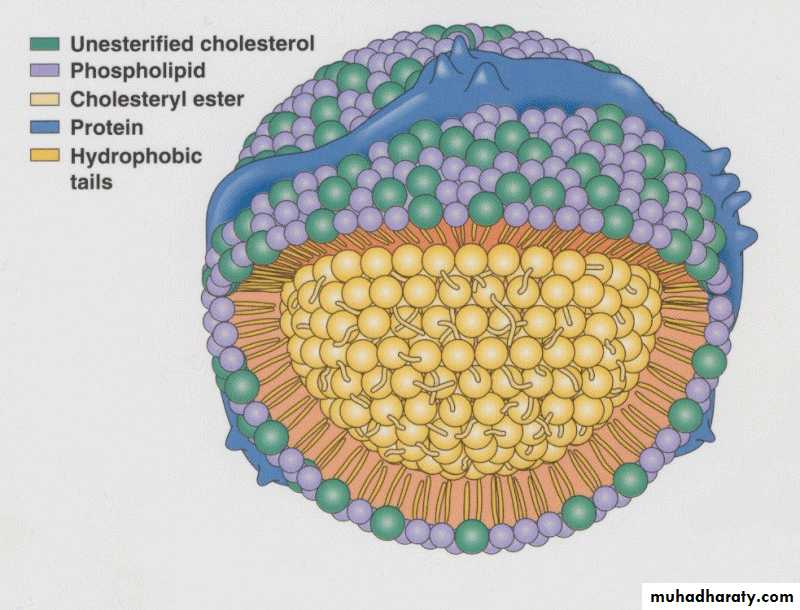
To accomplish this the lipids first is complexes with specific proteins (mainly globulin) to form lipoprotein.
The lipoprotein formed contains variable amount of triglycerides, phospholipids, cholesterol, and
proteins, which are soluble in the blood because of the presence of hydrophilic protein portion.
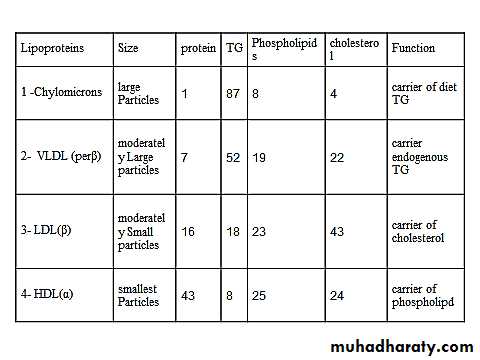
There are 4 major groups of lipoproteins that have been identified by means of ultracentrifugation & electrophoresis.
Types of lipoproteins:
Lipoproteins can be classified according to the density as:1. Chylomicrons: This has lowest density because the amounts of lipids are more than proteins, (Proteins have high molecular weight).
2. Very low-density lipoprotein (VLDL): also called Pre-β lipoprotein.
3. Lows density lipoprotein (LDL): also called β-lipoprotein.
4. High-density lipoprotein (HDL) also called α -lipoprotein.
The density of the lipoproteins depend on the quantity of proteins in the complex as proteins have high molecular weight then the density will increase with increased amount of proteins in the lipoprotein fraction.
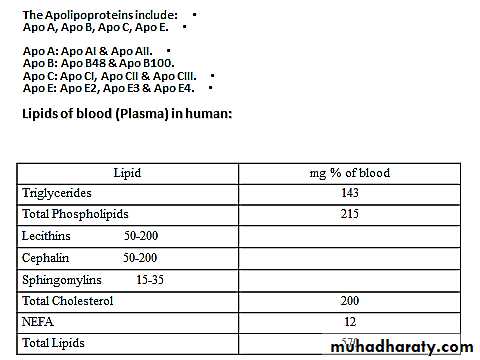
Average composition of the four major groups of lipoproteins in serum.
The large particles have a low density, high content of TG & low content of proteins.
As the particles become smaller their relative concentration of TG falls while the relative concentration of proteins will rise & these changes are accompanied by an increase in density.It is important to mention that there are considerable variation in size and composition of individual lipoprotein particles within each class.
The Apolipoproteins:
It is the protein part of the lipoproteins, which cover the lipid in the center of the lipoprotein to form a water-soluble mass by putting the lipid in the center and the protein on the outer surface.
The protein contents of lipoproteins differ widely in structure and functions. The apolipoprotein have been classified into groups e.g. apo A, apo B, etc. Some of these groups being subdivided further e.g. apoAI, apoAII etc. The roles of Apolipoproteins are:
1. Physical: They promote the solubility of lipids in plasma and enhance the stability of lipoprotein particles.
2. Regulatory: They have a role in controlling lipid metabolism e.g. the rate of tissue uptake of cholesterol or TG.
The large particles have a low density, high content of TG & low content of proteins.
As the particles become smaller their relative concentration of TG falls while the relative concentration of proteins will rise & these changes are accompanied by an increase in density.It is important to mention that there are considerable variation in size and composition of individual lipoprotein particles within each class.
The Apolipoproteins:
It is the protein part of the lipoproteins, which cover the lipid in the center of the lipoprotein to form a water-soluble mass by putting the lipid in the center and the protein on the outer surface.The protein contents of lipoproteins differ widely in structure and functions. The apolipoprotein have been classified into groups e.g. apo A, apo B, etc. Some of these groups being subdivided further e.g. apoAI, apoAII etc. The roles of Apolipoproteins are:
1. Physical: They promote the solubility of lipids in plasma and enhance the stability of lipoprotein particles.
2. Regulatory: They have a role in controlling lipid metabolism e.g. the rate of tissue uptake of cholesterol or TG.
Lipemia:
It is a term given when the blood lipids increase above the normal limit. The conditions, which lead to Lipemia, are:1. After meal rich in lipids (Physiological condition).
2. In diabetes Mellitus
3. During Starvation
4. In certain cases of Nephrosis and Myxodema.
Nephrosis: Excretion of protein with urine will occur.
Myxodema: Result from accumulation of protein in the lymph vessels.
In these cases lipid of blood increase due to decreased amount of protein in the blood and so the blood became turbid.
Lecture No. 12
β-Oxidation of fatty acids
Energetic of fatty acid oxidation:
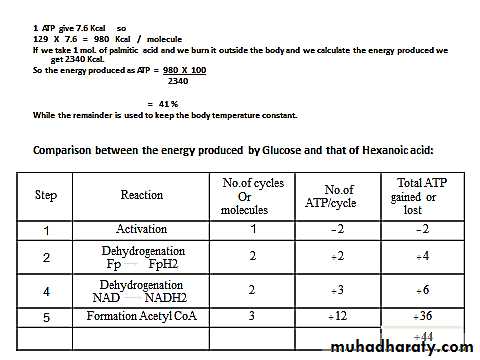
Comparison between the energy produced by Glucose and that of Hexanoic acid:
Role of Carnitine in fatty acid oxidation:
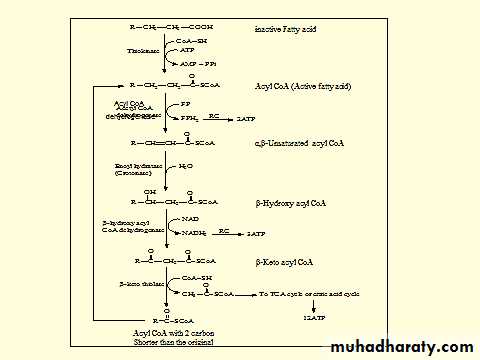
Fatty acid oxidation (Knoop's theory or β -Oxidation theory):
Also called lipolysis.The major route of fatty acid oxidation is the β-oxidation, which was proposed by knoop.
The name is derived from the oxidation of the activated fatty acid (Acyl CoA) in the β -carbon atom with the removal of 2 carbon atoms each time as Acetyl-CoA.
These reactions are catalyzed by group of enzymes in the mitochondria known as fatty oxidases.
The hydrolysis proceeds as follows:
When the no. of carbon atoms in the fatty acid is an even no. the hydrolysis procedure will continue till the end, while if the no. of carbon atoms is an odd no. then the hydrolysis continue till 3 carbon atoms remain which is propionyl CoA this is changed to SuccinylCoA which is a member of citric acid cycle.
Energetic of fatty acid oxidation:
The no. of cycles to reach the end products is equal to the No. of carbon atoms of the fatty acid devided by 2 minus 1 e.g. palmitic acid (16 carbon atom).
No. of Cycles is =16/2 = 8
8 - 1 = 7
No. of high energy phosphate bonds is 5 in each term, so
7 X 5 = 35 ATP
In this way 8 Acetyl CoA is formed, so
8 X 12 = 96 ATP & so
+35 From β- Oxidation
+96 From TCA cycles
-2 In step no. 1
-----------
129
It is known that glucose molecule give rise to 38 ATP while Hexanoic acid give rise to 44 ATP i.e. 6ATP more than given by carbohydrate.
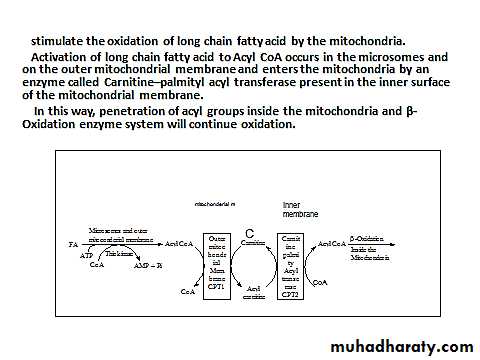
Role of Carnitine in fatty acid oxidation:
Long chain fatty acids cannot penetrate the mitochondrial membrane as happen with short chain fatty acids where they are oxidized inside the mitochondria by β -Oxidation system. Carnitine, which is β -Hydroxy
γ -trimethyl ammonium butyrate
In this way, the odd No. fatty acid will be converted to an even no. fatty acid and can be oxidized by the β-Oxidation enzyme system.
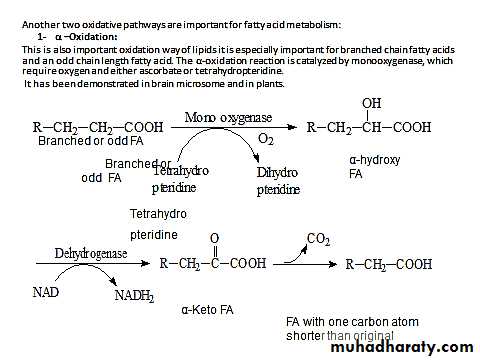
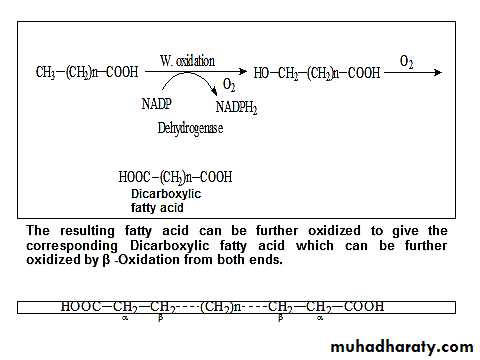
2.Omega Oxidation (Werkade):
This oxidation refers to the oxidation of the terminal carbon atom. Omega oxidation has been demonstrated in the liver microsomes and in some bacteria and the reaction is catalyzed by dehydrogenase, which requires NADP.
Lecture No 13
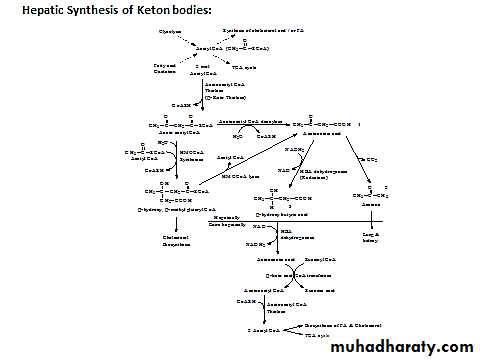
Keton bodies; Ketosis and Ketonemia:2. Formation, Utilization &Excretion of Keton Bodies:
3. Hepatic Synthesis of Keton bodies:
Keton bodies;
Ketosis and Ketonemia:
The Keton bodies or acetone bodies are aceto acetic acid, β-hydoxy butyric acid and acetone.
Under normal condition Keton bodies are formed in small amount in the liver.
These Keton bodies go to the blood to be oxidized extrahepatically in the peripheral tissues such as muscles, brain, kidney, lung, testes, etc. and this can occur by forming Acetyl CoA and enter the TCA Cycle.
This happen because the liver lack the enzyme β -Keto acid CoA Transferase.
Under certain metabolic conditions e.g. Starvation, diet rich in lipids, or high fat diet, also in sever cases of Diabetes Mellitus, and in certain conditions which leads to depletion of carbohydrate stores in the body, there will be an increase in the ratio of fatty acid oxidation (Lipolysis) in the liver.
This will produce a large amount of Keton bodies. The Keton bodies produced will accumulate in the blood, giving rise to ketosis.
So ketosis is the case in which the Keton bodies are produced more than the ability of the body to utilize them.
While, Ketonemia; is the increase in the concentration of Keton bodies in the circulation above the normal level.
Aceto acetic acid and β-Hydroxy butyric acids are organic acids. In ketosis they must be neutralized before excretion, this will lead to depletion of alkaline store or reserves in the body, leading to metabolic acidosis and loss of water and electrolytes.
These losses will account for reduction of circulatory blood flow, cardiac output, blood pressure, and renal flow, which is accompanied by collapse and shock.
This is usually seen in advanced stage of Diabetes Mellitus.
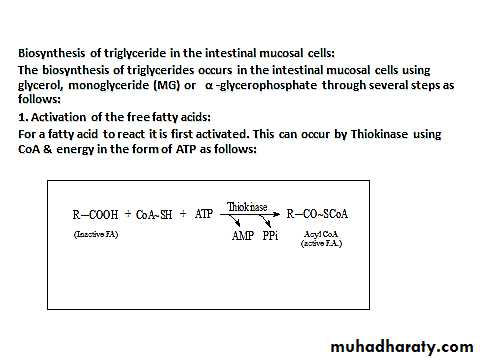
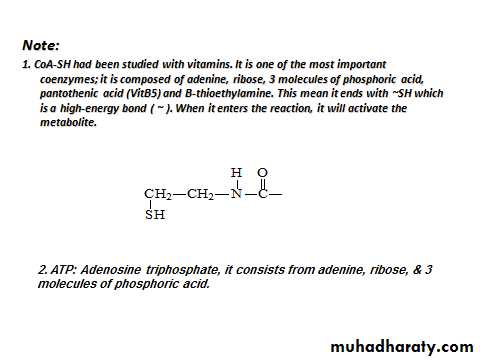
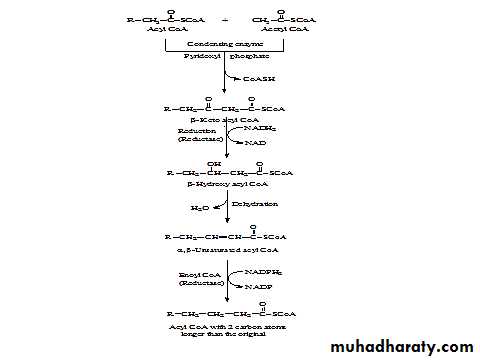
Biosynthesis of Lipids (Lipogenesis):
Fatty acids can be synthesized either in or out side the mitochondria.Mitochondria System of fatty acid synthesis:
In this system the mitochondria can catalyze the incorporation of AcetylCoA to existing fatty acid with intermediate chain length e.g. Stearic acid and palmitic acid.
Aceto acetic acid and β-Hydroxy butyric acids are organic acids. In ketosis they must be neutralized before excretion, this will lead to depletion of alkaline store or reserves in the body, leading to metabolic acidosis and loss of water and electrolytes.
These losses will account for reduction of circulatory blood flow, cardiac output, blood pressure, and renal flow, which is accompanied by collapse and shock.
This is usually seen in advanced stage of Diabetes Mellitus.
Biosynthesis of Lipids (Lipogenesis):
Fatty acids can be synthesized either in or out side the mitochondria.Mitochondria System of fatty acid synthesis:
In this system the mitochondria can catalyze the incorporation of AcetylCoA to existing fatty acid with intermediate chain length e.g. Stearic acid and palmitic acid.
Pyridoxal Phosphate or B6 is one of the most important coenzyme for many enzymes including transaminases and for carboxylase and condensing enzyme.
Vit B6 has many important biochemical functions especially in the brain metabolism.
Deficiency of VitB6 leads to dermatitis, loss of weight and mental disturbance.
It is present in leafy green vegetables and milk.
It is used as anti emetic during pregnancy.
Lecture No.14
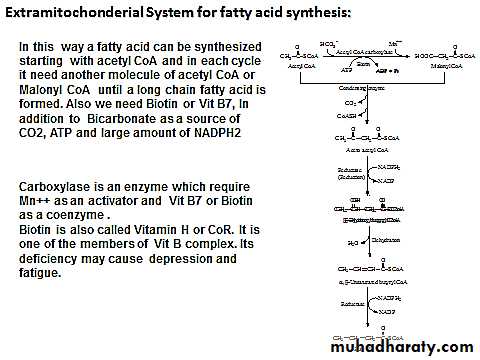
Extramitochonderial System for fatty acid synthesis:
Role of Insulin and citrate:
The liver and Lipid metabolism:
When the butyrylCoA takes the place of AcetylCoA and condense with
malonylCoA and the process is repeated for a total of 7 times palmitylCoA and then palmitic acid is the major end product.Summary:
CH3-CO~SCoA + 7HOOC-CH2CO~SCoA + 14NADPH2
CH3-(CH2)14-CO~SCoA + 7(CO2 + CoASH + H2O) + 14NADP
The high requirement of NADPH2 can be met by the production of NADPH2 via hexose monophosphate shunt.
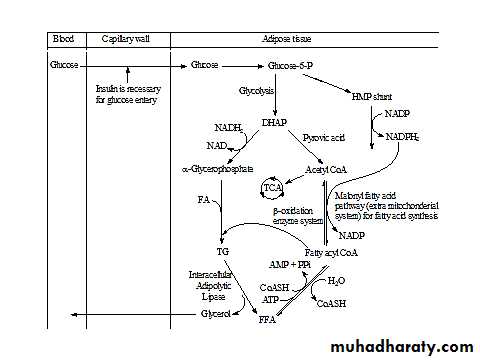
Role of Insulin and citrate:
Insulin act to stimulate fatty acid synthesis by increasing the supply of AcetylCoA because of increasing glucose utilization. This is a point for the interconnection between carbohydrate and lipid metabolism in the body.Citrate also stimulates the synthesis of AcetylCoA and MalonylCoA which are needed for the fatty acid synthesis,
whereas the end products e.g. palmitylCoA inhibit the pentose shunt and different key enzymes.
It appears that the control mechanisms are trying to coordinate the rate of synthesis with the rate of utilization of fatty acids and with the state of carbohydrate metabolism.
The liver and Lipid metabolism:
The liver can take up the plasma free fatty acids very actively for the synthesis of triglycerides and phospholipids, which may be stored in the liver or released into circulation. However, the liver and other tissues can utilizes free fatty acids for energy purposes more efficiently.
The liver has important role in cholesterol metabolism, for either synthesis of cholesterol or its conversion to bile acids.
3. Normal livers contain about 5% lipids. These lipids are found in kwpffur cells in the form of droplets. This figure may increase due to different factors. When the quantity of lipids in the liver reaches about 25-30% the case is called fatty liver.
This is may be due to many physiological or pathological factors. In this case the fatty globules will replace the entire cytoplasm of the cells and the liver cells become fibrotic and when the condition persist it will cause liver cirrhosis with impaired liver functions.
Lecture No. 15
Fatty liver syndrome:The factors causing fatty liver
Fatty liver syndrome:
There are many conditions, which result in the accumulation of fat and other lipids in the liver causing fatty livers, these conditions, include:1. Decreased fatty acid oxidation or
2. Increased fatty acid synthesis or
3. Impaired removal of fats from the liver or
4. Excessive mobilization of fats from the depots.
If this case is prolonged, this condition may lead to:
1. Enlargement of the liver
2. Fibrotic changes of the liver
3. Cirrhosis of the liver.
4. Severely impaired liver functions
Fatty livers may result from a number of abnormalities in the lipid metabolism. The factors causing fatty liver can be divided as follows:
I. Nutritional factors:
Prolonged increase of free fatty acids in the plasma :
This case may result from the:
a. Excessive mobilization of fatty acids from the adipose tissues or may be due:
b. Hydrolysis of plasma lipoproteins or chylomicrons, resulting in accumulation of triglycerides and hence fatty liver will result.
A similar situation may be found when:
c. Prolonged feeding of a high fat diet
d. During starvation or in :
e. Uncontrolled diabetes and when developed to Ketosis
2. Impairment in the biosynthesis of plasma lipoprotein:
In this case lipid transport is impaired specially triglycerides due to decreased lipoprotein (VLDL) resulting in accumulation of fats so fatty liver occurs.
This type of fatty liver associated with lack of lipotropic factor particularly Choline and Methionine. Methionine will be changed to Choline, which is necessary for the formation of Lecithin. (Phospholipids).
The Choline is required for the synthesis of phospholipids (Lecithin) as it forms a part of its structure. It is synthesized by trasmethylation of Methionine (Which is an amino acid) hence diet low in protein may indirectly cause fatty livers.
3- Deficiencies of certain vitamins e.g. Vitamin E, B6, B5 (pantothenic acid). Also deficiency of certain nutrients e.g. essential fatty acids have been reported to produce fatty livers in experimental animals.
The mechanism is not clear, for essential fatty acids may cause decreased synthesis of phospholipids.
In addition, excessive ingestion of cholesterol and some other substances e.g. Cysteine and Serine may result in fatty liver.
Cholesterol may react with essential fatty acids to form esters so phospholipids synthesis may be decreased due to decreased essential fatty acids.
For Cystein and Serine they may encourage the synthesis of proteins so Methionine may be used for protein biosynthesis so Choline biosynthesis may be decreased.
Endocrine Factors:
Hormones, which increase hepatic lipids storage includes:
Adrenocorticotrophic hormones ACTH (Pituitary) which increase miniralocorticoids and glucocorticoids.
Adrenal cortical hormones e.g. cortisol, aldosterone and androgens.
Sex steroids.
Insulin.
III. Other factors:
The use of certain drugs or certain toxic substances:This include certain antibiotics e.g. puromycine, also alcohol, chloroform, carbon tetrachloride, phosphorous, lead & arsenic الخارصين.
The mechanism of action of these substances appears to be inhibition of hepatic protein synthesis.
Lecture No. 16
Lipid Metabolism in Adipose tissues:
Regulation of lipid metabolism in adipose tissues:
Lipid Metabolism in Adipose tissues:Adipose tissues function as an area for caloric storage when there is an excessive intake of calories. This will be transformed to fatty acid and to triglycerides and stored in the adipose tissues.
While when there is a stress or other energy defects fatty acids will be released from the adipose tissues.
Glucose by itself can provide all the atoms needed for triglyceride synthesis.
Cholesterol Biosynthesis:
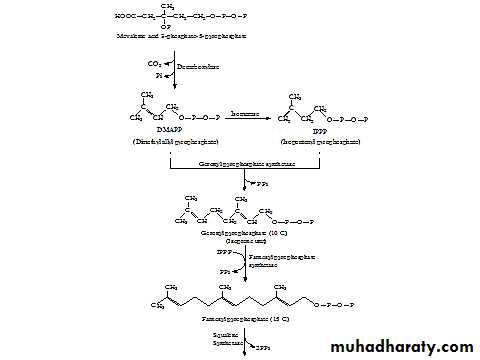
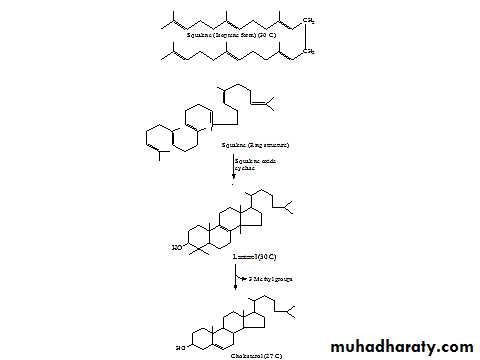
Tissues known to be capable of synthesizing cholesterol include the liver, adrenal cortex, skin, and intestine.AcetylCoA is the source of all the carbon atoms in cholesterol through several stages and can be summarized as follows:
Synthesis of mevalonic acid (6 Carbon atoms)
Loss of carbon dioxide CO2 from mevalonic acid to form isoprenoid units ( 5 carbon atoms )
Condensation of 6 isoprenoid units to give squalene (30 carbon atoms )
Transformation of squalene to Lanosterol.
Conversion of Lanosterol to Cholesterol (27 carbon atoms).
Lecture No. 17
1. Metabolism of Cholesterol2. Compounds lowering blood cholesterol level:
3. Dietary factors:
4. Hypocholesterolemic drugs:
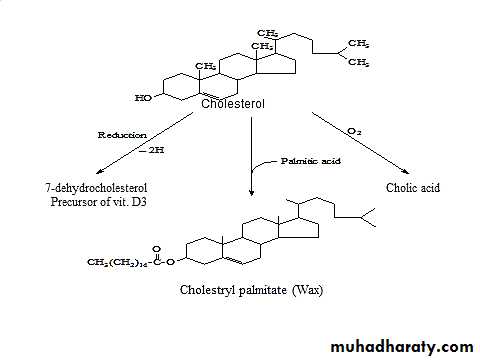
Metabolism of Cholesterol:
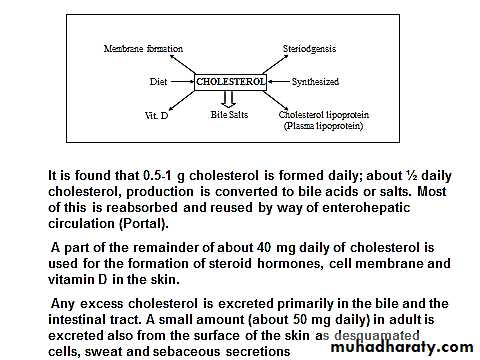
Cholesterol is the most important compound of those classified as sterols. Cholesterol is a precursor of bile salts, steroid hormones, and vitamin D.Dietary sources of cholesterol amounting between 500-750 mg daily in the adults, which are in the form of animal products (meat, livers, eggs and milk lipids).
It is estimated that a 70-kg adult male has some 75-150 g of cholesterol in his body. Serum cholesterol level range from 150-200 mg % (Desirable to be less than 200 mg/dl or less than 5 mmol/L).
In normal adults cholesterol is found in the liver (about 0.3%) skin (0.3%) brain tissues (2%) intestine (0.2%) and certain endocrine gland with the adrenal glands containing about 10%
As much as 50% of myelin sheath that surrounds the nerves is cholesterol, which is necessary for proper nerve conduction, and normal brain functions.
The relatively high content of cholesterol in the skin may be related to vitamin D formation while that of adrenal and other endocrine glands is to steroid hormone synthesis.
Compounds lowering blood cholesterol level:
Dietary factors:Replacing polyunsaturated fatty acid instead of saturated fatty acids in the diet can lower the blood cholesterol level.
It is evident that arteriosclerosis may be due to relative deficiency of unsaturated fatty acids in the diet. On these bases corn or, cotton seed oil, lower the blood cholesterol level while butter fat increases the blood cholesterol level.
Hypocholesterolemic drugs:
Clofibrate: Trade mark (Atromide-S):This drug will inhibit the hepatic cholesterol biosynthesis and lowering the VLDL.
D-Thyroxin:
It lowers cholesterol in the blood by accelerating the catabolism of cholesterol.
3.Cholestyramine:
It lower blood cholesterol level by increasing the excretion of cholesterol this will inhibit the enterohepatic circulation of the bile and increasing the catabolism of cholesterol to replace the loss of bile acid.
Nicotinic Acid:
It decreases the plasma lipids (Cholesterol & triglyceride) by interfering with the fatty acid metabolism.
Estrogen:
It lowers blood cholesterol level by decreasing LDL (the major carrier for cholesterol).
Etofibrate (Lipo-Merz retard 500mg):
It lowers cholesterol and triglyceride. It is used for the treatment of primary and secondary hyperlipidemias.Statine derivatives
(Simvastatine, lovastatine, rosuvastatin,
fluvastatin & Atorvastatin):
They act as an inhibitor for HMGCoA reductase.