Smear layer in Endodontics
The American Association of Endodontists defined smear layer as’’ surface film of debris retained on dentin of root canal, after instrumentation with either endodontic files or Rotary instruments
It is a muddy material composed of an amorphous layer of organic Debris and sometimes bacteria and it is assumed that debris and bacteria left inside the canal can affect the prognosis of root canal treatment
Defenition
The term ’smear layer’ in endodontic treatment is used most often to describe the grinding debris produces iatrogenically by the cutting dentin of the root canal.It is generally recognized that debridement of the root canal is the most important aspect of successful endodontic treatment
Factors affecting formation of smear layer in endodontics
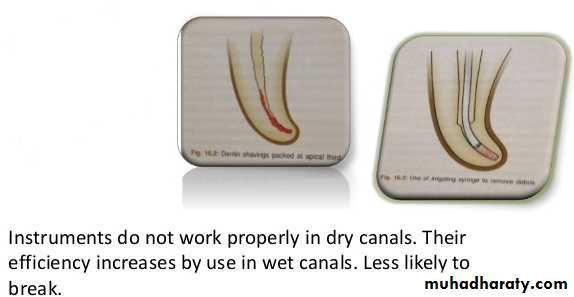
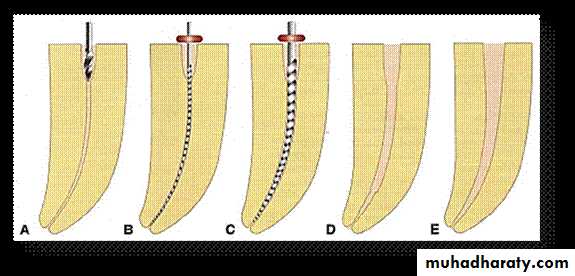
1-Type of Instruments : Increased centrifugal forces resulting from the movement and the proximity of the instrument to the dentine wall forms a thicker and more resistant smear layer (Jodakin and Austin, 1981) and thus the amount produced during automatic preparations, as with Gates-Glidden or post drills, will be greater in volume than that produced by hand filling2- Dentin cut wet / dry : – Filing a canal without irrigation (or cutting without a water spray) will produce a thicker layer of dentin debris and smear layer.
3-Proximity of the instrument of dentin walls:
More closely the instrument to dentinal walls more is the centrifugal forces producing thicker smear layer.4-Size and shape of root canals :
On account of the reduced dimension of the root canal, air bubbles frequently remain trapped and prevent total filling with the irrigant.Mechanical stirring with a lentulospiral removes the air bubbles, favors improved contact of EDTA with the canal walls, and takes the solution to areas that are not reached by the irrigating needle.
Organic component.
consists of heated coagulated proteins (gelatin formed by the deterioration of collagen heated by cutting temperatures), necrotic or viable pulp tissue, odontoblastic processes, saliva, blood cells and micro-organisms.Inorganic component.
is made up of tooth structure and some non-specific inorganic components.
Components of the smear layer
Reduction of dentin permeability to toxins and oral fluids.
• Reduction of diffusion (usually inwards by convection and outwards by hydrostatic pressure) of fluids and prevents wetness of cut dentin surface.• Bacterial penetration of dentinal tubules is prevented.
Advantages of smear layer in endodontic
• Smear layer is permeable to bacterial toxins.
It may harbor bacteria, either from original carious lesion or saliva, which may multiply taking nourishment from smear layer or dentinal fluid.
• Smear layer itself is infected. (Presence of bacteria)
• The smear layer may prevent the adhesion of composite resin system, bonding agents, GIC and polycarboxylate cements
Disadvantage of smear layer
• It blocks the antimicrobial effects of intracanal disinfectants and increases disinfecting tissue.
• Presence of smear layer would necessitate use of higher concentration and / or amount of anti bacterial agents.
• Acts as a intermediate physical barrier, interfere with adhesive penetration of sealers (Obturating materials) with dentinal tubules.
Smear layer in endodontics
When pathologic changes occur in the dental pulp, the root canal system can harbour several species of bacteria, their toxins and by products.These bacteria are predominantly gram- negative anaerobes
The morphology of the root canals is very complex therefore the mechanically prepared canals contain areas not accessible by endodontic instruments and bacteria will be found more in number in these areas.
Physical Barrier for Bacteria and disinfectants
Available evidence shows that bacteria and its by products present in infected root canals may invade the dentinal tubules. • Investigators have reported the presence of bacteria in the dentinal tubules of infected teeth at approximately half the distance between the root canal walls and the cemento-dentinal junction.
Bacterial penetration into the dentinal tubules is seen upto 150 m. in the apical 2/3rd of the root.
Thus even after chemomechanical instrumentation of the root canal, some bacteria still remain in the canal and dentinal tubules, for this reason, chemomechanical cleansing is often supported by the use of disinfectants
An important consideration in endodontics is the ultimate seal of root canals in order to prevent possible microleakage which may be the cause of future failure of the root filling.
Prepared dentin surfaces should be very clean to increase the sealing efficiency of obturation.
.
Smear Layer and Microleakage
Smear layer on root canal walls acts as an intermediate physical barrier and may interfere with adhesion and penetration of sealers into dentinal tubules
The use of injected thermoplasticized gutta-percha should be accompanied by the use of sealer regardless of whether or not the smear layer has been removed.
An absence of the smear layer causes less apical leakage than gutta-percha filled canal with the smear layer intact.
Apical Leakage
Chemical removal:
The quantity of smear layer removed by a material is related to its pH and the time of exposure (Morgan & Baumgartner 1997).A number of chemicals have been investigated as irrigants to remove the smear layer.
According to Kaufman & Greenberg (1986), a working solution is the one which is used to clean and irrigate the canal.
Methods to remove the smear layer
1- Chlorhexidine (CHX)
Relative absence of toxicityBroad spectrum antimicrobial substative activity (containued antimicrobial effect) because it binds (is adsorped) and released gradually from the hydroxyapatite surfaces.
2% CHX has similar antimicrobial action as 5.25% Naocl and is moe effective against Enterococcus faecalis
Advantage of CHX
2ry endodontic infections
At the end of chemomecaical preparation, because CHX doesn’t cause erosion of dentin like Naocl does as the final rinse after EDTA.
The activity of CHX is greatly reduced in the presence of orgainc matter.
Disadvantage of CHX
Cannot be the main irrigant in standard endodontic cases, because CHX doesn’t dissolve the smear layer or necrotic tissue.2- Sodium hypochlorite:
Naocl is one of the most widely used irrigating solution.Household bleach such as Chlorox contain 5.25%naocl .(INGLE)
Full strength (5.25%) is highly irritating to periapical tissues and reduces the flexural strength and elastic modulus of dentin.
A 2,25% is common concertation which decrease toxicity and still maintains some tissue dissolving and antimicrobial activity.
Advantages of NAOCL
Disove organic tissue,necrotic and vital organic tissue (unique property)Antimicrobial action
Lubricant
Inexpensive and readily a vailable
Disadvantage of NAOCL
Irritant to periapical tissues, mucous membrane and skin (INGLE).Unpleasent odour.
Can damage clothes.
The use as the final rinse following EDTA or citric acid(CA) produce severe erosion of the canal-wall dentin and should be avoided.
Causes haemolysis and ulceration, inhibits neutrophil migration and damages endothelial and fibroblast cels
3- EDTA(ethylene diamine tetra acitic acid)
Lubricant,chelator&declcifying agents.
Is the most effective chelating agent in endodontic therapy.
In general, file remove dentin faster than the chelators can soften the walls(Walton).
17% EDTA 1min remove inorgainc components.
EDTA is effective in smear layer removal only in coronal &middle thirds, but not in the apical component
EDTA has little effect on periapical tissue
Disadvantage of EDTA
Deactivation of (NAOCL) by reducing the available chlorine(WALTON)Contraindications of EDTA
• A large or blocked canal: if a sharp instrument is forced or rotated against a wallsoftened by the chelate, a new but false canal will be started
Curved canal once the large-sized instruments (size30 or greater)are being used
• These instruments are not as flexible as the smaller sizes and may produce root perforation
Precaution
EDTA will remain active within the canal for 5 days if not inactivated.
If the apical constriction has been opened, the chelate may seep out and damage
The periapical bone.
For this reason, at the completion of the appointment, the canal must be irrigated with Naocl
To in activate EDTA
4- Iodine Potassium Iodide(IKI)
Is less cytotoxic and irritating to vital tissues than Naocl and CHX, but obvious disadvantage of iodine is a possible allergic reaction in some patients.2 %and 4% iodine potassium iodide (IKI) has considerable antimicribial activity, but no tissue-disolving property.
It can be used at the end of chemomecanichal preparation like CHX.
Although Ca(OH) alone was unable to kill E>faecalis inside dentinal tubulus,Ca(OH)2 mixed with either IKI or CHX effectively disinfected entin
5- Hydrogen Peroxide (H2O2):
It destroy anaerobic microorganismsThe solvent action of H2O2 is less than that of Naocl, so H2O2 is less damaging to periapical tissues.
Solutions of (H2O2 and Naocl) may ueses alternatly during treatment this method is strongly suggested for irrigating canals of teeth that have been left open for drainage, because the effevecence is effective in disolving food parycles and other debris that may have packed the canal
Disadvantage of (H2O2)
Should not be the last irrigant used in a canal, because nascent oxygen may remain and cause pressure. Therefore Naocl should be used to react with H2O2 and liberate the Oxygen remainingIt was found when a quaternary ammonium bromide (CETRMIDE) has been added to(EDTA)solutions during instrumentation, there was no smear layer remaining except in the apical part of the canal.
Salvizol (Ravens Gmbh, Germany) is a commercial brand of 0.5% BDA(Bis-dequliium-acitate) and possesses the combined actions of chelation and organic debridement.
Kaufman et al. (1978) reported that Salvizol had better cleaning properties than EDTA.
6- Tetracyclines have low PH in concentrated solution,so it acts as a calcium chelator and cause root surface demineralize.
Hazne (2001) showed that 1% tetracycline hydrochloride or 5% citric acid can be used to remove the smear layerof root canal.
7- MTAD
A mixture of tetracycline isomer (doxycycline) an acid (Citric acid) and detergentAdvantage of MTAD
BiocompatibleMTAD may be superior to Naocl in antimicrobial action
MTAD is effective in killing E.faecalis found in failing treatment
MTAD doesn’t alter physical properties of dentin
MTAD can be used at the end of chemomecanical preparation after Naocl
8- Citric Acid (CA)
is a powerful antimicrobial agent, but its antimicrobial action is not as great as that of 5.25 percent sodium hypochlorite, which acts as a broad spectrum antibiotic effectively against bacteria, bacteriophages, spores, yeasts, and viruses.• Combining the two, sodium hypochlorite followed by 6 per cent citric acid would give an ideal endodontic irrigant.
9-Laser removal
Lasers can be used to vaporize tissues in the main canal, remove the smear layer and eliminate residual tissue in the apical portion of root canals..
Advantage depends on many factors,
including the power level,
the duration of exposure,
the absorption of light in the tissues, the geometry of the root
canal and the tip-to-target distance
Disadvantage:
The main disadvantage with laser removal of the smear layer in the small canal spaces with the relatively large probes that are available• The problem of smear layer is yet a controversy. To keep it or remove it is still a problem.
• However, if the smear layer is to be removed the method of choice seems to be the alternate use of EDTA and sodium hypochlorite solutions, or to use other Irrigants ,It is up to the dentists judgment
Conclusion
• Ingle’s Endodontics 6th Edition.
• Violich DR, Chandler NP. The smear layer in endodontics–a review. International Endodontic Journal. 2010 Jan 1;43(1):2-15.• Torabinejad M, Handysides R, Khademi AA, Bakland LK. Clinical implications of the smear layer in endodontics: a review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2002 Dec 31;94(6):658-66.
• Czonstkowsky M, Wilson EG, Holstein FA. The smear layer in endodontics. Dental Clinics of North America. 1990 Jan;34(1):13-25.
• Şen BH, Wesselink PR, Türkün M. The smear layer: a phenomenon in root canal therapy. International Endodontic Journal. 1995 May 1;28(3):141-8
References