Streptococcal disease
Group A (Beta hemolytic)1
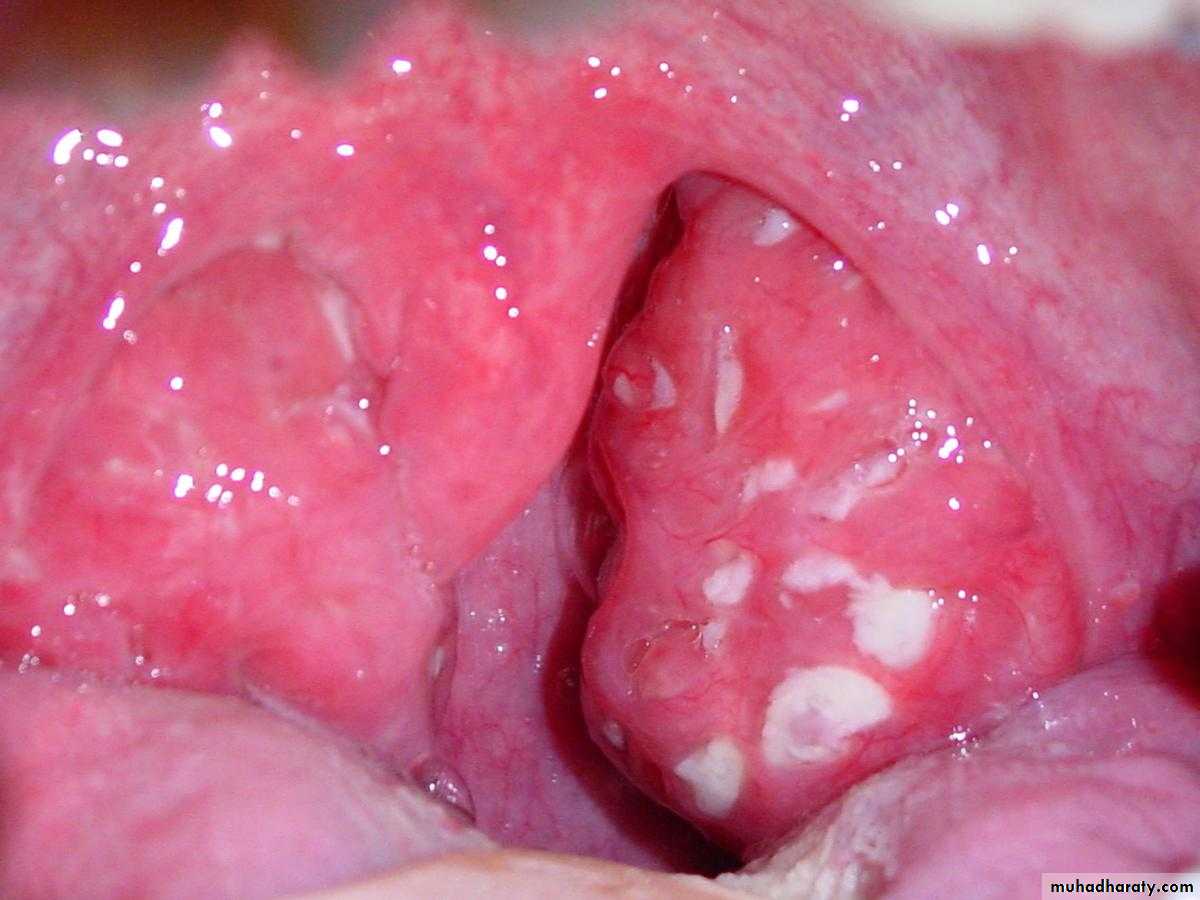
1.Strept. Sore throat:
Presented with sudden onset fever, exudative tonsils or pharynx, tender enlarged ant. Cervical LN, absence of cough or rhinorrhea .Subsequent OM or peritonsillar abscess may occur.
AGN can occur within1-5 weeks (mean 10days)RF can occur within 3 weeks (mean 19 days)
2
3
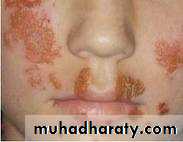
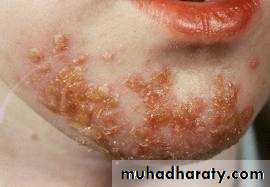
2.Strept. Skin infection :
(pyoderma, impetigo). usually superficial may proceed to vesicular, pustular, and encrusted stage.RF is not an important complication, however AGN may occur later usually 3 weeks after skin infection.
4
3.Scarlet fever :
It occurs when the infecting strain of Strept. Produces pyrogenic exotoxine (erythrogenic toxin) & the patient is sensitized but not immuned to the toxin.It present with fever, nausea, vomiting, fine erythema punctate blanch on pressure (sandpaper) sparing the face
5
4.Erysipelas and acute cellulites :
Red, Tender, edematous spreading lesion with definite raised border6
Infection agent:
Streptococcus Pyogenes, (group A).Of approximately 130 serologically distinct types.
Group A Strept. producing skin infection Are usually of different serologic types from those associated with throat infection.7
In scarlet fever, three immunological different types of erythrogenic toxin (pyrogenic exotoxin A,B &C) have been demonstrated
M-type mucoid strains are involved in recent outbreaks of RF.
8
Occurrence :
Strept. sore throat &scarlet fever are common in temperate zones.In apparent infection is common
Strept. Sore throat is unusual <2-3 years. peak incidence in the age group 6-12 years &declines there after .
9
Reservoir : Human
Mode of transmission :Direct contact with patient or carriers
Large droplets
Indirect through contaminated articles (rare)
Nasal carriers are particularly likely to transmit diseases
10
Dried Strep. Reaching the air via contaminated items are viable but apparently non infectious for mm. &intact skin
Incubation period : 1-3 days
Period of communicability:
Untreated :10-21 days
Treated: 24 hours
The contagiousness of the carriers decreased sharply in 2-3 weeks after onset of infection.
11
There is maternal immunity
There is tendency for repeated attack of RF with further cardiac damage following each attack of Strept. Group A infection.Recurrence of AGN is unusual
One attack of erysipelas predispose to subsequent attacks.
12
• Prevention:
• mode of transmission• 1. Public education relation to AGN &RF
• prompt Dx
• complete course of antibiotic
• Provide easily accessible lab. facilities for recognition of group A Strept.
• Milk pasteurization
• Safe preparation of food
• Exclusion of people with skin infection for food handling
• Secondary prevention of complication
13
Control
Reporting is not necessary except at time of epidemic.Isolation
Disinfection of discharge
Search and treat carriers among contacts
Specific Rx penicillin is drug of choice for 10 days (oral or IM) (no resistance) and erythromycin if there is penicillin allergy
14
TOXOPLASMOSIS
1516
Toxoplasmosis
1. Identification: A systemic protozoan disease; infections are frequently asymptomatic, or present as acute disease with L.N enlargement + fever.Toxoplasma cyst (containing viable organisms) may remains in tissues for life on the host.
17
• Transmission to the fetus occurs almost only when woman acquire infection during pregnancy.
• Conversely, women that has been infected before being pregnant have no risk of transmitting the disease to their offspring except in immune-compromised patient.
• Approximately 50-60% of fetuses whose mothers acquire the infection during the pregnancy will be affected.
Clinically
18
Congenital toxoplasmosis:
A primary infection during early pregnancy may lead to fetal infection with death or manifestations as chorioretinitis, brain damage with intracerebral calcification, hydrocephaly, microcephaly, jaundice, rash and hepatosplenomegaly.
Infection in late pregnancy → mild or sub clinical fetal disease + delayed chronic chorioretinitis. These infants should be observed over a period of up to 10 years for the development of antibodies, or for the development of lesions as delayed chronic chorioretinitis.
19
1. Clinical signs.
2. Serological tests:Serological test is the primary mean of diagnosis, but result must be interpreted carefully.
IgG Ab peak in concentration one to two months after infection & remain positive indefinitely. Direct agglutination test (DAT) detect IgG titer which reached to more than 1:1000 within 3 months of onset then decreased and remain at lower level for life.
Diagnosis
20
• Seroconvertion or fourfold increase of IgG Ab suggests recently acquired infection.
• Persistence of IgG Ab titer stable exclude recent infection.21
• IgM-specific Ab can be detected two weeks after infection & reach peak at one month & decline thereafter to disappear within six to nine months.
22
Diagnosis
• Clinical signs.
• Serological tests
•
• Culture (fluid, body tissue).
• Biopsy.
23
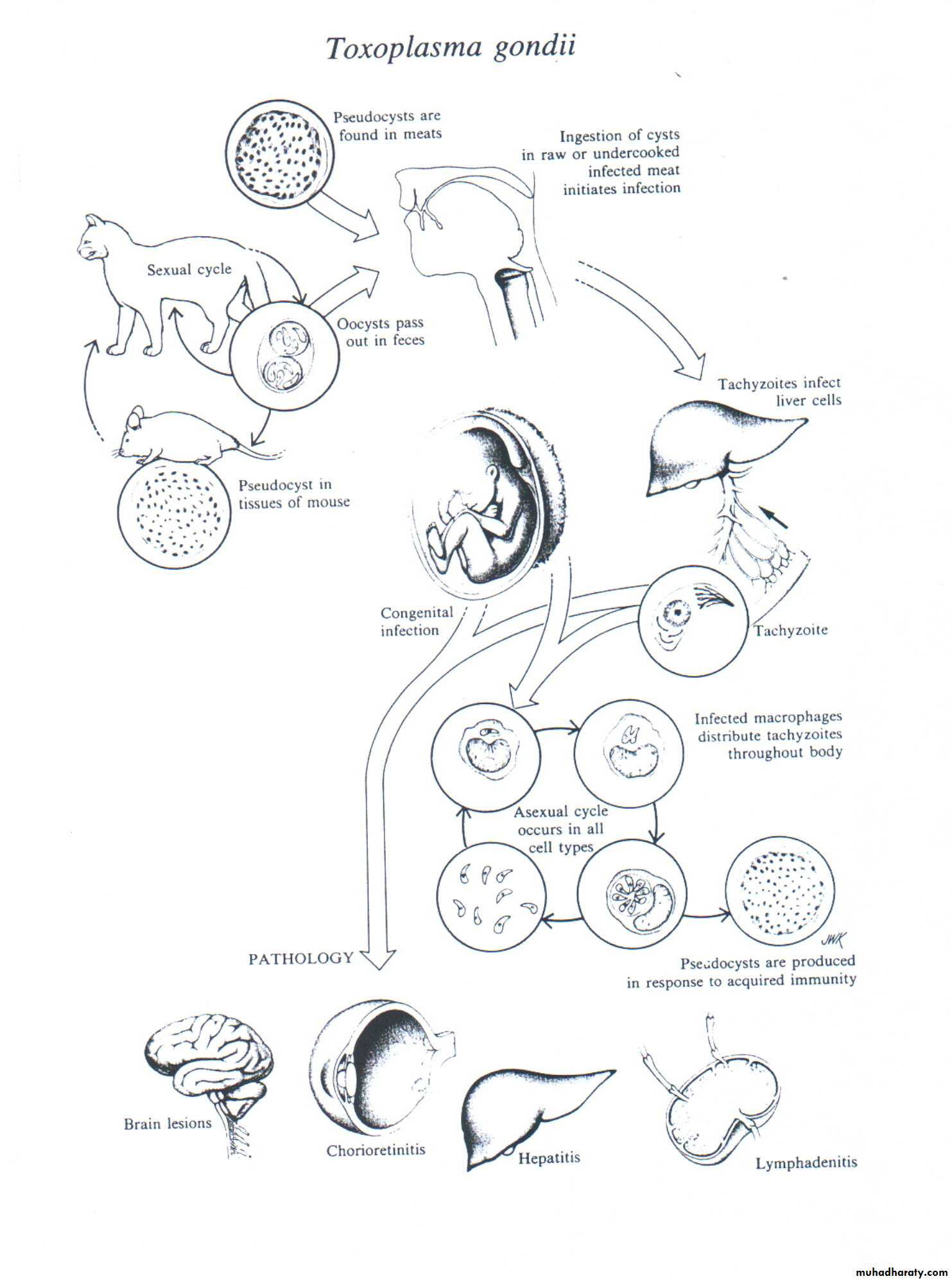
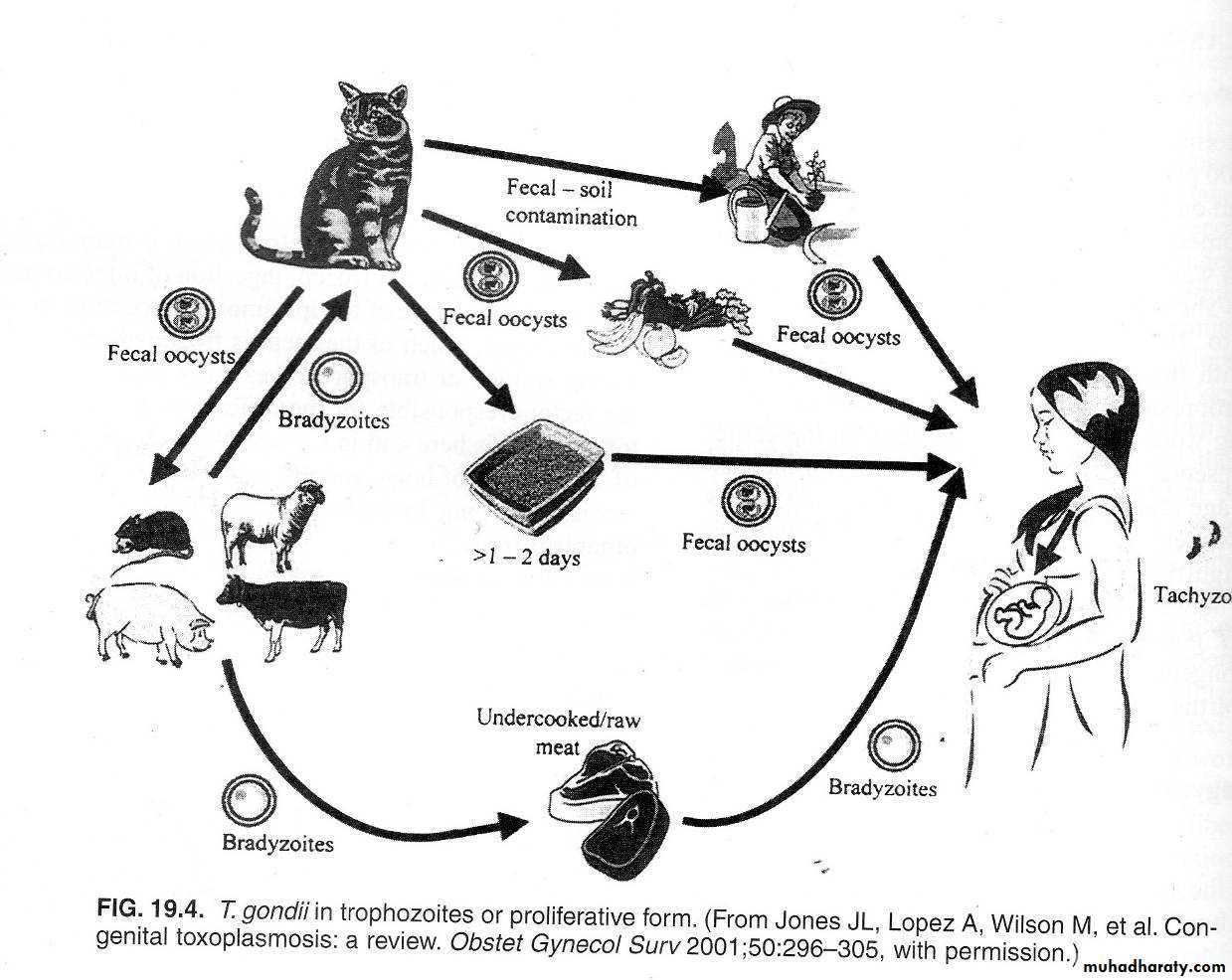
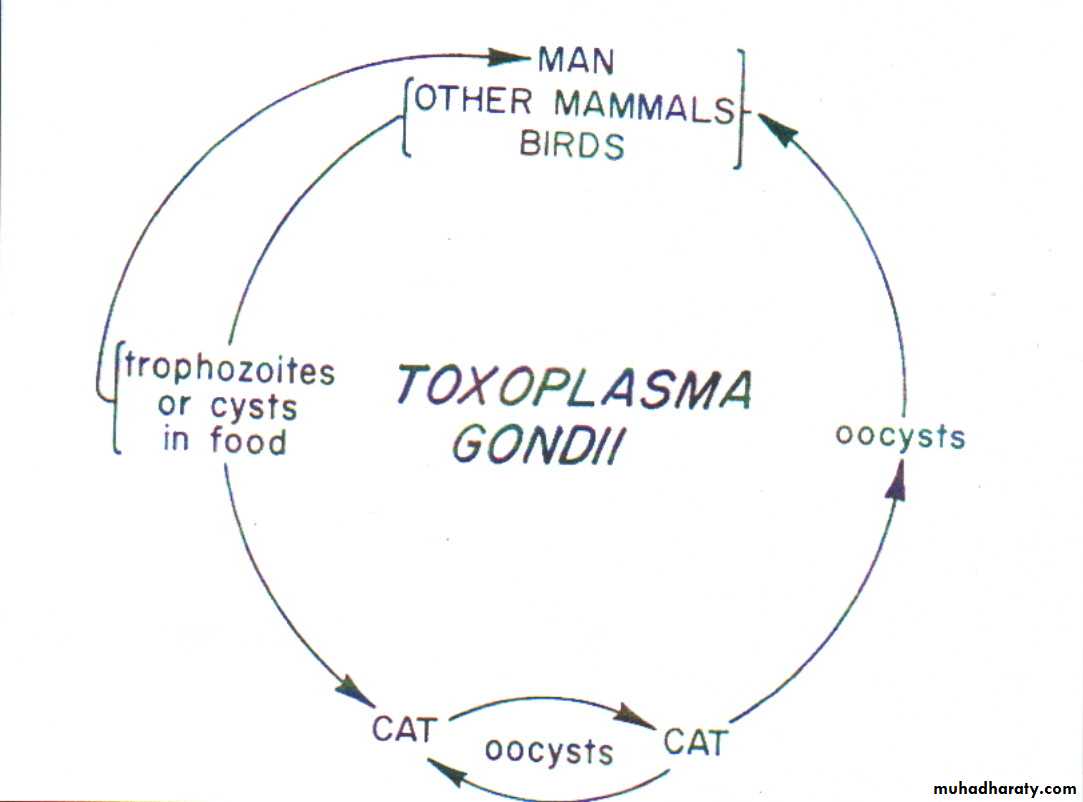
2. Infectious agents: Toxoplasma gondii, an intracellular protozoan of cat
2425
26
27
3. Occurrence: Infection in human is common; its distribution is world wide in mammals & birds.
• 4. Reservoir:
• Definitive hosts are cats (in intestinal tract) which acquire infection from eating infected mammals (rodents and birds).
•
• Intermediate hosts → sheep, goats, rodents, swine, cattle, chickens and birds.
28
5. Mode of transmission
• “No man to man transmission except in utero”• Transplacental infection to fetus.
• Eating raw or undercooked infected meat (pork or mutton, very rarely beef) containing tissue cysts.
• Ingestion of infected oocysts in food or water contaminated with cat feces. Consumption of raw goat milk.
• Blood transfusion or organ transplantation.
29
6. Incubation period: 10 – 20 days
7- Period of communicability:“No man to man transmission except in utero”.
8- Susceptibility: is general
immunity → long lasting or permanent
Ab persist for years, probably for life.
30
• A- Preventive measures:
• Educate pregnant women:
• Cook meat thoroughly or freeze it well (-20°C).
• Avoid cleaning litter pans and contact with cats
• Feed cats dry, canned or boiled food (keep them as indoor pets).
• Dispose of cat feces.
• Wash hands thoroughly after handling raw meat and soil.
9. Method of control:
31
B- Control of patients, contacts and environment:
• Reporting: none• Isolation: none
• Disinfection not applicable.
• Quarantine: not applicable.
• Immunization of contacts: not applicable.
• Investigation of contacts and source of infection: none
32
7) Specific treatment:
• combination of pyrimethamine (daraprim) + sulfadiazine + folinic acid for 4 weeks.• Add clindamycine and systemic corticosteroid in ocular toxoplasma.
• Treatment of pregnant women → spiramycine it prevents placental infection and reduces the frequency of maternal transmission in about 60%. Combination with other drugs might be more effective.
• Use triple regime if U.S or other investigations indicate that fetal infection has occurred, but avoid daraprim in 1st 16 weeks of pregnancy because of it's possible teratogenic effect.
33
In our country where maternal toxoplasmosis is common disease, routine screening during prenatal visits is mandatory.