Cardiac Lectures Dr. Ahmed Moyed Hussein
Anti-arrhythmic drug therapyClassification:
Anti-arrhythmic drugs may be classified according to their mode or site of action into (The Vaughan-Williams classification):
Fig: classification of antiarrhythmic drugs according to their site of action.
Class I drugs:Class I drugs act principally by suppressing excitability and slowing conduction in atrial or ventricular muscle.
They block sodium channels, of which there are several types in cardiac tissue. These drugs should generally be avoided in patients with heart failure because they depress myocardial function, and class Ia and Ic drugs are often pro-arrhythmic.
Class Ia drugs:
These prolong cardiac action potential duration and increase the tissue refractory period. They are used to prevent both atrial and ventricular arrhythmias.
Disopyramide. An effective drug but causes anticholinergic side-effects, such as urinary retention, and can precipitate glaucoma. It can depress myocardial function and should be avoided in cardiac failure.
Quinidine. Now rarely used, as it increases mortality and causes gastrointestinal upset.
Class Ib drugs:
These shorten the action potential and tissue refractory period. They act on channels found predominantly in ventricular myocardium and so are used to treat or prevent ventricular tachycardia and ventricular fibrillation.
Lidocaine. Must be given intravenously and has a very short plasma half-life, main side effects are: myocardial depression, confusion and convulsion.
Mexiletine. Can be given intravenously or orally, but has many side-effects.
Class Ic drugs:
These affect the slope of the action potential without altering its duration or refractory period. They are used mainly for prophylaxis of atrial fibrillation but are effective in prophylaxis and treatment of supraventricular or ventricular arrhythmias. They are useful for WPW syndrome because they block conduction in accessory pathways. They should not be used as oral prophylaxis in patients with previous MI because of pro-arrhythmia.
Flecainid: Effective for prevention of atrial fibrillation, and an intravenous infusion may be used for pharmacological cardioversion of atrial fibrillation of less than 24 hours’ duration. It should be prescribed along with an AV node-blocking drug, such as a β-blocker, to prevent pro-arrhythmia.
Propafenone: Also has some β-blocker (class II) properties. Important interactions with digoxin, warfarin and cimetidine have been described.
Class II drugs:
This group comprises the β-adrenoceptor antagonists (β-blockers). These agents reduce the rate of SA node depolarisation and cause relative block in the AV node, making them useful for rate control in atrial flutter and atrial fibrillation. They reduce myocardial excitability and the risk of arrhythmic death in patients with coronary artery disease and heart failure.Class III drugs:
Class III drugs act by prolonging the plateau phase of the action potential, thus lengthening the refractory period. These drugs are very effective at preventing atrial and ventricular tachyarrhythmias. They cause QT interval prolongation and can predispose to torsades de pointes and ventricular tachycardia, especially in patients with other predisposing risk factors.Amiodarone: It is probably the most effective drug currently available for controlling paroxysmal atrial fibrillation. It is also used to prevent episodes of recurrent ventricular tachycardia, particularly in patients with poor left ventricular function or those with implantable defibrillators. Amiodarone has a very long tissue half-life (25–110 days). An intravenous or oral loading regime is often used to achieve therapeutic tissue concentrations rapidly. The drug’s effects may last for weeks or months after treatment has been stopped. Side-effects are common (up to one-third of patients) including: photosensitivity, skin discoloration, corneal deposits, thyroid dysfunction, alveolitis, nausea and vomiting, hepatotoxicity, peripheral neuropathy, torsades de pointes, potentiate digoxin and warfarin effect.
Class IV drugs:
These block the ‘slow calcium channel’, which is important for impulse generation and conduction in atrial and nodal tissue, although it is also present in ventricular muscle. Their main indications are prevention of supraventricular tachycardia (by blocking the AV node) and rate control in patients with atrial fibrillation.Verapamil: The most widely used drug in this class. Intravenous verapamil may cause profound bradycardia or hypotension, and should not be used in conjunction with β-blockers.
Diltiazem: Has similar properties.
Other anti-arrhythmic drugs
Atropine sulphate (0.6 mg IV, repeated if necessary to a maximum of 3 mg): Increases the sinus rate and SA and AV conduction, and is the treatment of choice for severe bradycardia or hypotension due to vagal overactivity.Repeat dosing may be necessary because the drug disappears rapidly from the circulation after parenteral administration. Side-effects: dry mouth, thirst, blurred vision, atrial and ventricular extrasystole.
Adenosine: It produces transient AV block lasting a few seconds. It is used to terminate supraventricular tachycardias when the AV node is part of the re-entry circuit, or to help establish the diagnosis in difficult arrhythmias, such as atrial flutter with 2 : 1 AV block. Adenosine is given as an intravenous bolus, initially 3 mg over 2 seconds. If there is no response after 1–2 minutes, 6 mg should be given; if necessary, after another 1–2 minutes, the maximum dose of 12 mg may be given. Patients should be warned to expect short-lived and sometimes distressing flushing, breathlessness and chest pain. Adenosine can cause bronchospasm and should be avoided in asthmatics; its effects are greatly potentiated by dipyridamole and inhibited by theophylline and other xanthines.
Digoxin: It slows conduction and prolongs the refractory period in the AV node, this effect helps to control the ventricular rate in atrial fibrillation and may interrupt supraventricular tachycardias involving the AV node. Digoxin is largely excreted by the kidneys, and the maintenance dose should be reduced in children, older people and those with renal impairment. It is widely distributed and has a long tissue half-life (36 hours), so that effects may persist for several days. Measurement of plasma digoxin concentration helps identify digoxin toxicity or under-treatment.
Therapeutic procedures:
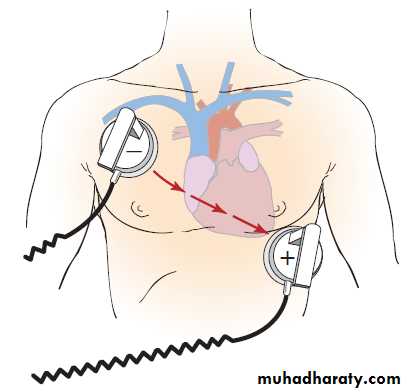
External defibrillation and cardioversion:The heart can be completely depolarised by passing a sufficiently large electrical current through it from an external source. This will interrupt any arrhythmia and produce a brief period of asystole that is usually followed by the resumption of sinus rhythm. Defibrillators deliver a DC, high-energy, short-duration shock via two large electrodes or paddles coated with conducting jelly or a gel pad, positioned over the upper right sternal edge and the apex. Modern units deliver a biphasic shock, during which the shock polarity is reversed mid-shock This reduces the total shock energy required to depolarize the heart.
Electrical cardioversion:
This is the termination of an organised rhythm, such as atrial fibrillation or ventricular tachycardia, with a synchronized shock, usually under general anaesthesia. The shock is delivered immediately after detection of the R wave ( synchronized shock) because, if it is applied during ventricular repolarization (on the T wave), it may provoke ventricular fibrillation. High-energy shocks may cause chest wall pain post-procedure, so, if there is no urgency, it is appropriate to begin with a lower-amplitude shock (e.g. 50 joules), going on to larger shocks if necessary.
Defibrillation:
This is the delivery of an unsynchronized shock during a cardiac arrest caused by ventricular fibrillation. The precise timing of the discharge is not important in this situation. In ventricular fibrillation and other emergencies, the energy of the first and second shocks should be 150 joules and thereafter up to 200 joules; there is no need for an anaesthetic, as the patient is unconscious.
Catheter ablation:
Catheter ablation therapy is the treatment of choice for patients with supraventricular tachycardia or atrial flutter, and is a useful treatment for some patients with atrial fibrillation or ventricular arrhythmias.A series of catheter electrodes are inserted into the heart via the venous system and are used to record the activation sequence of the heart in sinus rhythm, during tachycardia and after pacing manoeuvres. Once the arrhythmia focus or circuit is identified (e.g. an accessory pathway in WPW syndrome), a catheter is used to ablate the culprit tissue. For many arrhythmias, radiofrequency ablation is very attractive because it offers the prospect of a lifetime cure, thereby eliminating the need for long-term drug therapy.
Implantable cardiac defibrillators (ICD):
ICDs treat ventricular tachyarrhythmias using overdrive pacing, cardioversion or defibrillation. They are implanted in a similar manner to pacemakers. It is indicated in patients with previous attacks or at risk of ventricular arrhythmias.Sinoatrial nodal rhythms:
Sinus arrhythmia: Phasic alteration of the heart rate during respiration (the sinus rate increases during inspiration and slows during expiration) is a consequence of normal parasympathetic nervous system activity and can be pronounced in children. Absence of this normal variation in heart rate with breathing or with changes in posture may be a feature of autonomic neuropathy.
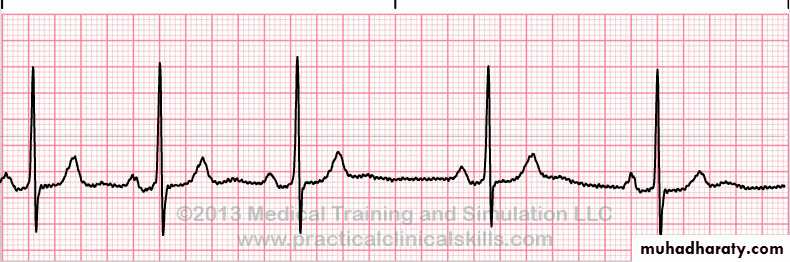
Fig: sinus arrhythmia
Sinus bradycardia: A sinus rate of less than 60/min may occur in healthy people at rest and is a common finding in athletes. Some pathological causes include:Myocardial Infarction
Sinus node disease (sick sinus syndrome)
Hypothermia
Hypothyroidism
Cholestatic jaundice
Raised intracranial pressure
Drugs, e.g. β-blockers, digoxin, verapamil
Fig: sinus bradycardia
sinus bradycardia requires no treatment. Symptomatic acute sinus bradycardia usually responds to intravenous atropine 0.6–1.2 mg.Sinus tachycardia:
This is defined as a sinus rate of more than 100/min, and is usually due to an increase in sympathetic activity associated with exercise, emotion, pregnancy or pathology , like:
Fever
Anaemia
Heart failure
Thyrotoxicosis
Phaeochromocytoma
Drugs, e.g. β-agonists (bronchodilators)
Fig: sinus tachycardia
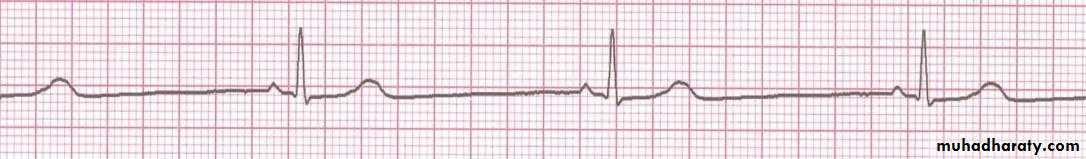
Treatment of sinus tachycardia is the treatment of underlying cause.Sinoatrial (SA node) disease (sick sinus syndrome):
Sinoatrial disease can occur at any age but is most common in older people. The underlying pathology involves fibrosis, degenerative changes or ischemia of the SA (sinus) node. The condition is characterized by a variety of arrhythmias:and may present with palpitation, dizzy spells or syncope.
Fig: sick sinus syndrome
A permanent pacemaker may benefit patients with troublesome symptoms due to spontaneous bradycardias. Pacing improves symptoms but not prognosis, and is not indicated in patients who are asymptomatic. Attacks of tachycardia can controlled by drug therapy.Atrial tachyarrhythmias
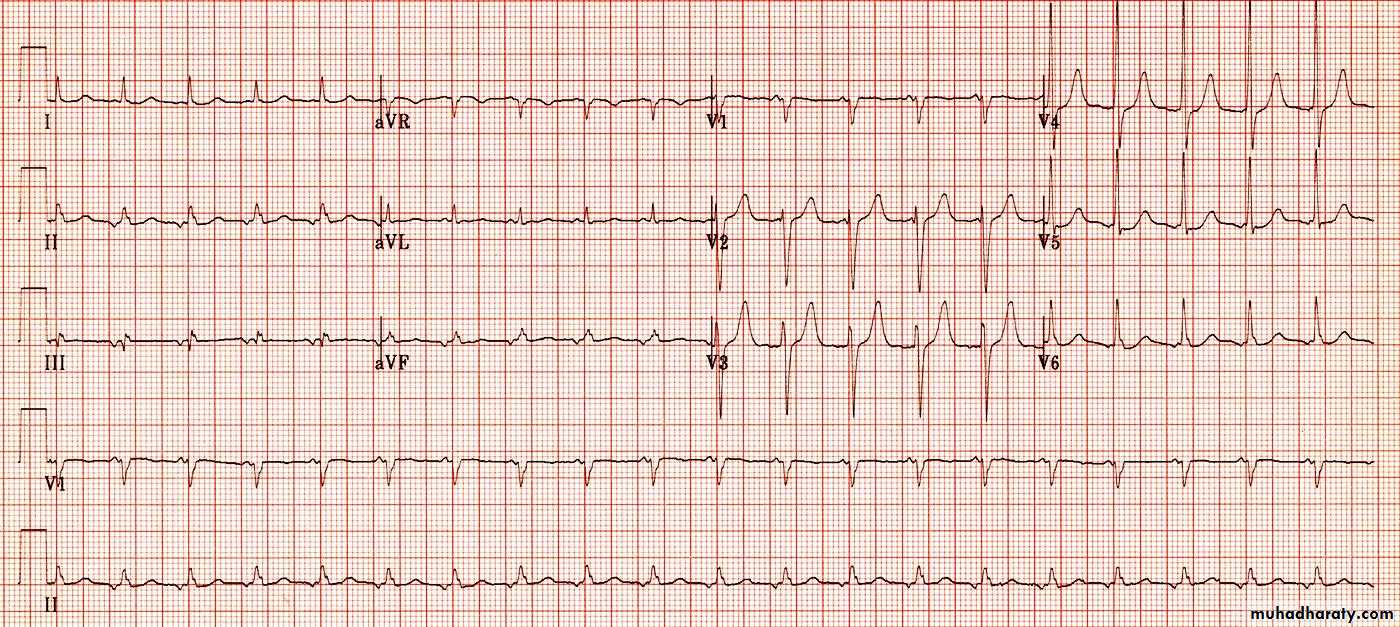
Atrial ectopic beats (extrasystoles, premature beats):These usually cause no symptoms but can give the sensation of a missed beat or an abnormally strong beat. The ECG shows a premature but otherwise normal QRS complex; if visible, the preceding P wave has a different morphology because the atria activate from an abnormal site.
Fig: atrial ectopic beats (second and 7th beat)
In most cases, these are of no consequence. Treatment is rarely necessary but β-blockers can be used if symptoms are intrusive.