Organophosphate poisoning
Dr. Shamil AL-Nuaimipest is any harmful, destructive, or troublesome animal, plant or microorganism.”
“…a pesticide is any substance or mixture of substances intended for preventing, destroying, repelling, or mitigating any pest.”Definition of Pesticide
Acute pesticide poisoning is an important cause of worldwide morbidity and mortality.
Ninety-five percent of fatal pesticide poisonings occur in developing countries. Serious cases of pesticide poisoning are more likely to occur in adults than in children.About three-quarters of the pesticide fatalities were due to suicide.
ExposureHome Exposure
• Accidental ingestion• Lawn and garden use
• Insect control
• Food supply
• Water supply
Occupational Exposure
• Farms & Farm worker
• Pesticide applicator
• Manufacture
• Mixing and handling
• Landscapers
Other Exposure
•Dietary exposure•Pesticide residues on crops
•Community exposure
•Airborne drift from commercial app
•Contaminated drinking water
•Leaching from soils to ground water
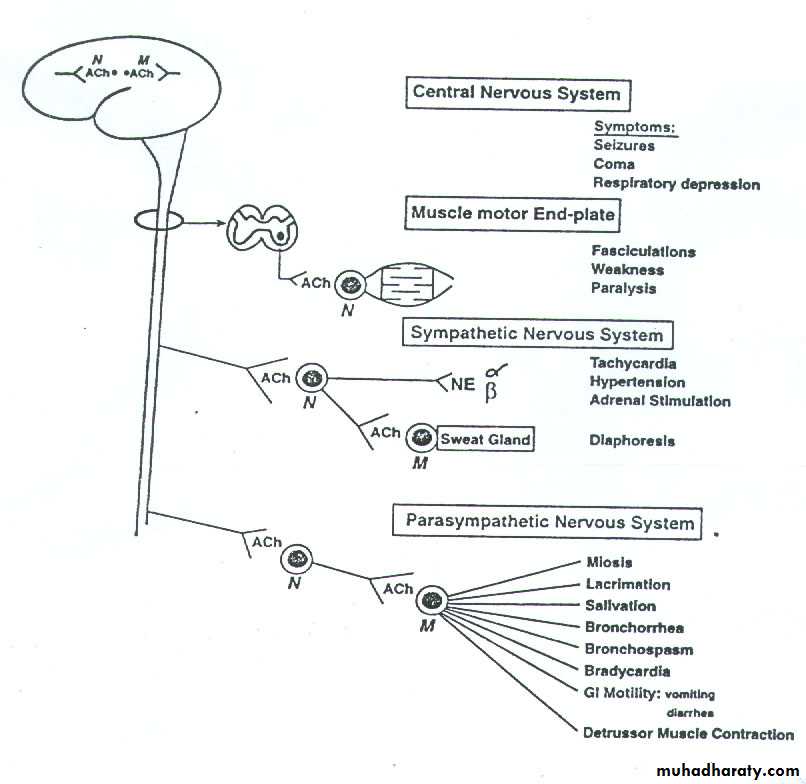
Organophosphate compounds produce muscle weakness by three different mechanisms:
The first occurs during the cholinergic phase.Fasciculation progress to paralysis due to depolarization and desensitization blocks at the on neuromuscular junction
MECHANISM OF ACTION
During the second or intermediate phase excessive entry of calcium ions into the muscle due to prolonged transmitter receptor interaction probably produces muscle necrosis.
Finally, muscle weakness may be due to demyelination of nerves.
This begins 2 to 3 weeks after intoxication and spares the muscle of respiration.
Acute Effects
Cholinergic FeaturesThe cholinergic effects of organophosphate poisoning depend on the balance between muscarinic and nicotinic receptors
The mnemonic DUMBELS describes signs of cholinergic excess.
Clinical Presentation
DUMBELS (diaphoresis and diarrhea; urination; miosis; bradycardia, bronchospasm, emesis; excess lacrimation; and salivation).Intermediate Syndrome
Occurs after resolution of acute cholinergic crisis.
24-96 hours after exposure.Characteristics:-acute respiratory paresis, muscular weakness
(facial, neck and proximal limb muscles).Cranial nerve palsies and depressed tendon reflexes (often)
Lacks muscarinic symptomatology. Result of pre-and postsynapticdysfunction of neuromuscular transmission.
Compounds involved are methyl parathion, fenthion and
dimethoate.(Organophosphate-induced delayed neuropathy)
Damage to afferent fibers of peripheral and central nerves andInhibition of “neuropathy target esterase” (NTE).
Certain OPs rarely cause this kind of neurotoxicity.
Manifests as weakness or paralysis and paresthesia of the
extremities. Predominantly legs. May persists for weeks to years.Suggested diagnostic criteria for the organophosphate-induced delayed syndrome include the following:
1. A history of severe acute organophosphate poisoning about 1 to 6 weeks prior to the onset.
. 2. Symptoms and signs of polyneuropathy and later with or without concurrent pyramidal signs.
. 3.Denervation changes shown by electromyography.
. 4.Slow recover.
. 5.Reasonable exclusion of other nervous disease
Chronic Effects
Skin decontamination
Gastrointestinal decontaminationPulmonary ventilation
Cardiopulmonary monitoring
Treatment
Aging:- As time progresses with OP binding to AChE, it’s phosphoryl bond is strengthened by loss of one alkyl group from phosphoryl adduct.(Pralidoxime use therefore is limited after a couple of
days).Atropine noncompetitively antagonizes both muscarinic and CNS effects of organophosphate poisoning
Atropine has no effect on muscle weakness or respiratory failure in severe poisoning, since this drug does not reactivate the cholinesterase enzymes.
ANTIDOTES
For a therapeutic intravenous dose in symptomatic patients, use 2 to 4 mg in adults or 0.015 to 0.05 mg/kg in children every 15 minutes as needed.
The administration of atropine as an antidote does not require confirmation by acetylcholinesterase levels.
The drying of secretions or full atropinization, rather than dilated pupils, is the effective endpoint of atropine titration.
Do not wait for the return of cholinesterase levels before treating significantly symptomatic patients with atropine.
Alternate routes for atropine administration (when rapid intravenous access cannot be achieved) may induce the intraosseous route in children, and nebulized atropine by inhalation in adults.
Therapy with 2PAM should be continued for at least 18 hours or longer, depending on the patient's clinical status and the properties of the suspected toxin.
In a severely poisoned adult the dosage of pralidoxime (e.g., 500 mg/hour) should be continuously maintained until clear and irreversible clinical improvement is achieved. This may take days until residual insecticide is cleared from body stores
Pralidoxime (2PAM)
If severely dyspneic give 4 to 6 mg atropine plus 2PAMCl 1 g IV. Watch heart rate, blood pressure
If moderate exposure to vapor (respiratory distress, gastrointestinal signs and symptoms, muscle twitching): give 6 mg atropine and 2PAMCl. Always give diazepam (10 mg IM)
Cautions
Seizures often respond to atropine and 2PAM. If they do not, give diazepam.
Watch for worsening of respiratory depressionObserve for recurrence of nicotinic symptoms. If they do not recur for the next 24 hours, discontinue therapy.
Weaning the patient off should be performed by set increments (e.g., 25% every 8 hours). Watch the patient for at least 1 hour after each adjustment.
1.Avoid parasympathomimetic agents (physostigmine, succinylcholine) because they may potentiate anticholinesterase activity
2.Phenothiazines and antihistamines have anticholinesterase activity
3.Central nervous system depressants (e.g., opiates)
During antidote administration, the patient should be followed closely for signs of respiratory failure and atropinization
Full recovery generally occurs within 10 days when optimum treatment is quickly instituted.
Persistent CNS effects and peripheral neuropathies have been reported in a few survivors.
The patient must avoid reexposure until cholinesterase activity is over 75% of normal survivors
Prognosis