Uveitis
Definition: it is an inflammation of the uveal tract (Iris, Ciliary body and choroid) and adjacent structures, most probably the retina.Classification:
- Anatomical.
- Clinical.
- Aetiological.
Anatomical Classification:
1- Anterior uveitis: which is subdivided into:a- Iritis: in which inflammation predominantly affects the iris.
b- Iridocyclitis: in which both the iris and anterior part of the ciliary body (pars plicata) are equally involved.
2- Intermediate uveitis:
It is characterized by involvement predominantly of the posterior part of the ciliary body (pars plana), periphery of the retina and the underlying periphery of the choroid.
3- Posterior uveitis:
Inflammation of the choroid and retina posterior to the equator of the eye.
4- Panuveitis:
Involvement of the entire uveal tract.
Clinical classification:
1- Acute uveitis: usually has a sudden, symptomatic onset and persists for up to 3 months. If the inflammation recurs following the initial attack it is referred as recurrent acute uveitis.2- Chronic uveitis: the onset is frequently insidious and may be asymptomatic. It usually persists for longer than 3 months. Acute or subacute exacerbations on chronic may occur.
Aetiological classification:
1- Idiopathic: which forms more than 50% of cases of uveitis.2- Associated with a systemic disease, e.g.:
a- Spondyloarthopathies: ankylosing spodylitis, Reiter's syndrome, psoriatic arthritis and chronic juvenile arthritis.
b- Inflammatory bowel disease: ulcerative colitis, Crohn's disease, Whipple's disease.
c- Nephritis.
d- Non-infectious multi-system disease: sarcoidosis, Behçet's disease.
e- Infectious systemic disease: e.g. TB, syphilis
f- Diabetes.
3- Infections:
a- Bacterial: tuberculosis. b- Fungal: Candidiasis. c- Viral: Herpes Zoster.
4- Infestations:
a- Protozoa: Toxoplasmosis. b- Nematodes: Toxocariasis.
Clinical Features:
Anterior uveitis
Symptoms:
• Acute anterior uveitis: Photophobia, pain, redness, decreased visual acuity and lacrimation.
• Chronic anterior uveitis: may be asymptomatic or give rise to mild redness and the perception of floaters.
Signs:
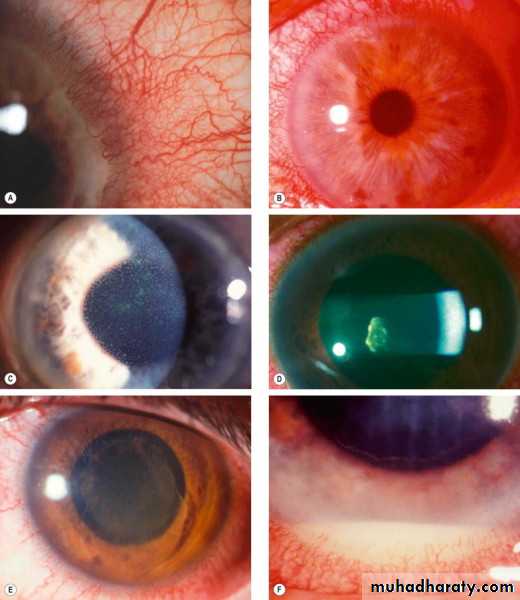
1- Circumcorneal injection: acute anterior uveitis has a violaceous hue.2- Miosis
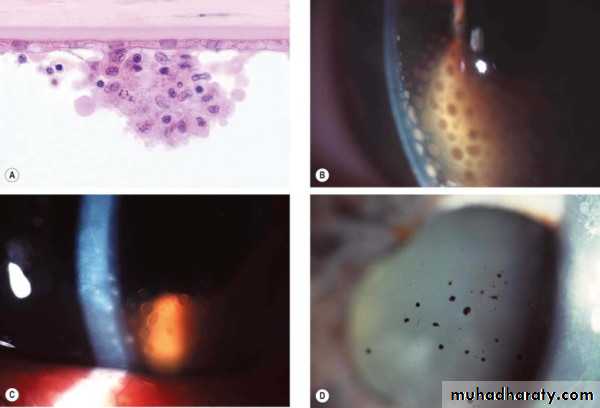
3- Keratic precipitates: cellular deposits on the corneal endothelium (deposition of inflammatory cells into corneal endothelium).
Their characteristics and distribution may indicate the probable cause of uveitis.
4- Cells: indicative of acute inflammation: it is graded from 1 to 4.
a- Aqueous cells.
b- Anterior vitreous cells.
5- Aqueous flare: is seen due to scattering of light by proteins that have leaked into aqueous humour by break down of blood-aqueous barrier. It is graded from 1 to 4 according to its haziness or obscuration to the details of iris.
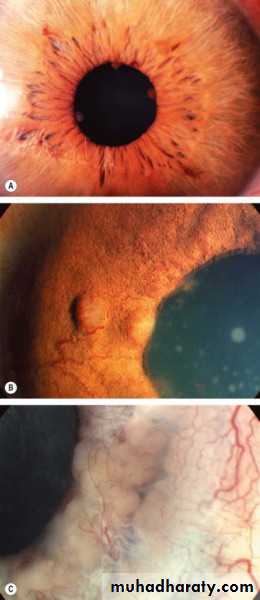
6- Iris nodule: which is a feature of chronic granulomatous inflammation.
7- Hypopyon
Complications of anterior uveitis:
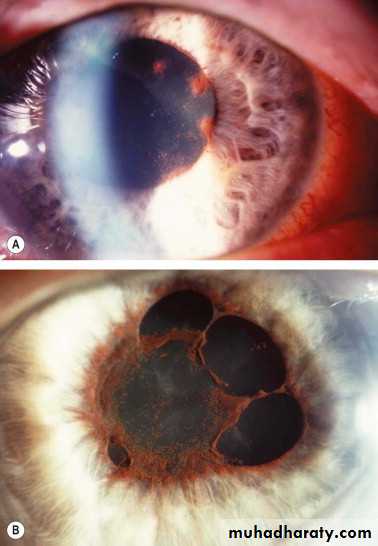
1- Posterior synechiae: 360° (seclusio pupillae) causes iris bombé that leads to closure of the angle of anterior chamber and ends with secondary angle closure glaucoma.2- Cataract.
3- Glaucoma: inflammatory or secondary angle closure glaucoma.
4- Cyclitic membrane formation which leads to traction and then detachment of the Ciliary body which causing phthisis bulbi.
Intermediate Uveitis
Symptoms:Initially, floaters (inflammatory cells in anterior vitreous) and later, decreased visual acuity due to macular edema (due to associated vitritis).
Signs:
Cellular infiltration of vitreous (vitritis).
Vitreous snowballs
Peripheral periphlebitis
Snowbanking is characterized by a grey-white fibrovascular plaque which may occur in all quadrants, but is most frequently inferior
Complications:
• Cystoid macular oedema.• Cyclitic membrane and phthisis bulbi.
• Cataract.
• Tractional retinal detachment.
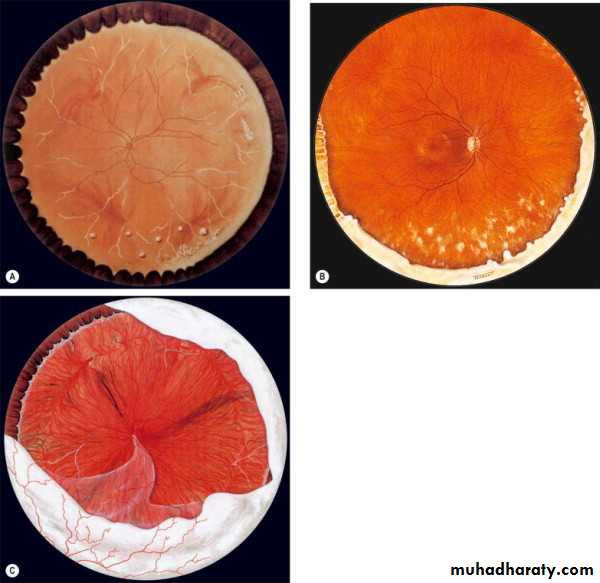
Posterior uveitis
Symptoms:1- Floaters (due to cells and flare in the vitreous).
2- Impairment of visual acuity (due to macular oedema).
Signs:
1- Cells, flare, opacities and posterior vitreous detachment (inflammatory process of vitreous (vitritis)
leads to its shrinkage and then separation of posterior vitreous face from the retina).
2- Retinitis: ill-defined, focal, white, cloudy appearance of retina with obscuration of retinal vessels.
3- Vasculitis: acute vasculitis, which is characterized by a fluffy white haziness surrounding the blood vessels.
Complications:
1- Cystoid macular oedema.2- Macular ischaemia.
3- Epiretinal membrane formation.
4- Vascular occlusion.
5- Retinal detachment (tractional).
6- Consecutive optic neuropathy (due to ischaemia that affects the ganglion cells layer, nerve fiber layer and the optic disc itself).
Special investigations for patients with uveitis:
1- X-Ray:- Sacroiliac joint (for ankylosing spondylitis). - Chest x-ray (for TB and sarcoidosis). - Skull calcification: toxoplasmosis.
2- Skin test: histoplasmosis, Mantoux and kveim (for sarcoidosis).
3- Serum tests: ANA (Anti-Nuclear Antibodies) as in chronic juvenile arthritis, VDRL, toxoplasmosis test (IFAT) and ELISA.
4- HLA-typing: HLA-B27 for ankylosing spondylitis and B5, B51 for Behçet's disease.
Treatment:
1- Mydriatics:Short acting: Tropicamide 0.5% (for <1y) & 1% (for > 1y), the duration of action is 6 hours.
Cyclopentolate 0.5% (for <1y) & 1% (for > 1y), the duration of is 24hours.
Phenylnephrine (sympathetic agonist)
Long acting: Atropine 0.5% (for <1y) & 1% (for > 1y), it is the most powerful cycloplegic and mydriatic, its duration of action is 2 weeks.
Indications for these mydriatic and cycloplegic drugs:
a- To promote comfort through muscles paralysis (except phenynephrine).
b- To prevent formation of posterior synechiae through continuous movement of the pupil.
c- To break down recently formed synechiae.
2- Steroids:
-Topical steroids: only for anterior uveitis, because they do not reach therapeutic levels behind the lens. Potent steroids are: prednisolone acetate, dexamethasone and betamethasone.Side effects of topical steroids (especially after prolonged use):
a- Glaucoma.
b- Cataract.
c- Corneal complications: they are rare, e.g. bacterial and fungal keratitis and recurrence of herpes simplex
keratitis.
d- Systemic side effects.
-Periocular injection of steroids:
Indications:a- Severe acute anterior uveitis.
b- As an adjunct to topical or systemic steroid in resistant cases. c- Intermediate uveitis.
d- Poor patient compliance with topical or systemic steroids.
-Intravitreal injection of steroids:
Injection of triamcinolone acetonide (2mg in 0.05ml) in resistant uveitic chronic cystoid macular oedema.-Systemic steroids:
Prednisolone tablets
Indications:
a- Intractable anterior uveitis resistant to topical and periocular steroids.
b- Intermediate uveitis unresponsive to preiocular injection.
c- Posterior ueveitis or panuveitis, particularly with severe bilateral involvement.
3- Immunosuppressive agents:
Either Antimetabolites (cytotoxic) as Azathioprine and Methotrexate, Or T-cell inhibitors as ciclosporin.Indications:
a- Sight (vision)-threatening uveitis:
Which is usually bilateral, non-infectious and has failed to response to adequate steroid therapy.
b- in patients with intolerable side effect from systemic steroids.