
Lecture-1
Respiratory System
We will focus on these main points about respiration:
1. Pulmonary Ventilation
2. Pulmonary Circulation, Pulmonary Edema, Pleural Fluid
3. Physical Principles of Gas Exchange; Diffusion of Oxygen and Carbon Dioxide through the Respiratory
Membrane
4. Transport of Oxygen and Carbon Dioxide in Blood and Tissue Fluids
5. Regulation of Respiration
6. Respiratory Insufficiency—Pathophysiology, Diagnosis, Oxygen Therapy
Anatomy of the Respiratory System
The lungs fill most of the thoracic cavity except for the space occupied by the heart and major blood vessels.
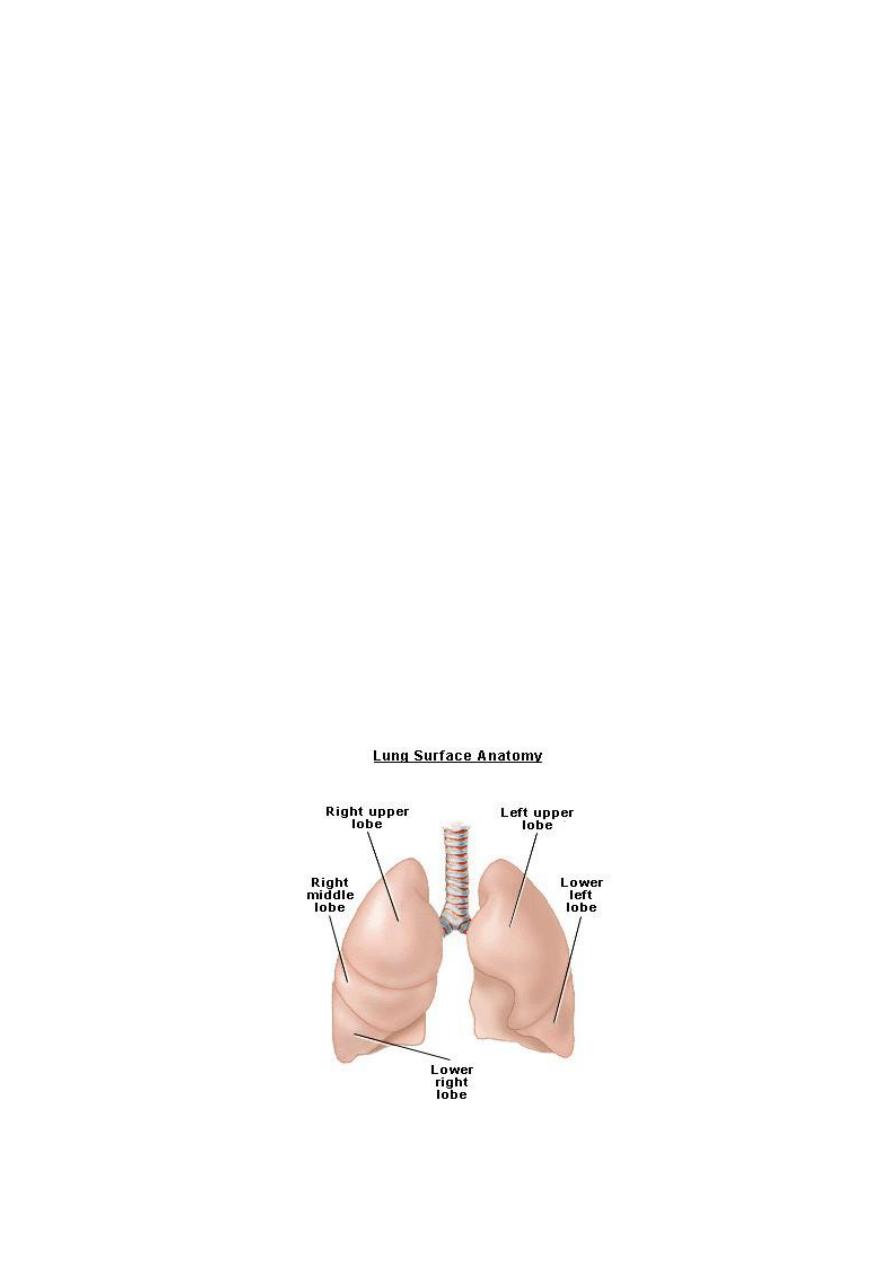
The lung consist of two lungs, right lung consist of three lobs ,right upper, middle and lower lobs (fig 1).
Left lung consist of two lobs, left upper and lower lobs.
The respiratory air passages consist of
1-Upper respiratory tract: refers to the nasal cavity, the pharynx.
2-Lower respiratory tract: includes the larynx, trachea which is divided into 2 bronchi, then bronchi is
divided into bronchioles, then terminal bronchioles, then respiratory bronchioles, then alveolar duct and
alveoli. These multiple divisions greatly increase the total cross-sectional area of the airways. Consequently,
the velocity of air flow in the small airways declines to very low values. There are 300 million alveoli in
humans and the total area of the alveolar walls in contact with capillaries in both lungs is about 70 m
2
.
Pulmonary Ventilation
The goals of respiration are to provide oxygen to the tissues and to remove carbon dioxide. To achieve
these goals, respiration can be divided into four major functions: (1) pulmonary ventilation, which means the
inflow and outflow of air between the atmosphere and the lung alveoli; (2) diffusion of oxygen and carbon
dioxide between the alveoli and the blood; (3) transport of oxygen and carbon dioxide in the blood and body
fluids to and from the body’s tissue cells; and (4) regulation of ventilation and other facets of respiration.
Mechanics of Pulmonary Ventilation (fig 2)
During inspiration (during normal quiet breathing), the first method is contraction of the diaphragm to
lengthen chest cavity and pull the lower surfaces of the lungs downward. The second method for expanding
the lungs is to raise the rib cage which increases the anteroposterior diameter between sternum and spine. All
the muscles that elevate the chest cage are classified as muscles of inspiration. The most important muscles
of inspiration are the external intercostals, but others that help (deep breathing) are the (1)
sternocleidomastoid muscles, which lift upward on the sternum; (2) anterior serrati, which lift many of the
ribs; and (3) scaleni, which lift the first two ribs.
During expiration, the diaphragm simply relaxes, and the elastic recoil of the lungs, chest wall, and
abdominal structures compresses the lungs and expels the air. During heavy breathing extra force is achieved
mainly by muscles of expiration that pull the rib cage downward during expiration are mainly the (1)
abdominal recti, which have the powerful effect of pulling downward on the lower ribs at the same time that
they and other abdominal muscles also compress the abdominal contents upward against the diaphragm, and
(2) internal intercostals.

Movement of Air In and Out of the Lungs and the Pressures That Cause the Movement
The lung is an elastic structure that collapses like a balloon and expels all its air through the trachea
whenever there is no force to keep it inflated.
Also, there are no attachments between the lung and the walls
of the chest cage, except where it is suspended at its hilum from the mediastinum.
Pleural Pressure and Its Changes during Respiration (fig 3)
Pleural pressure is the pressure of the fluid in the thin space between the lung visceral pleura and the chest
wall parietal pleura. Pleural fluid lubricates movement of the lungs within the cavity and due to continual
suction of excess fluid into lymphatic channels maintains a slightly negative pressure.
Normal pleural
pressure at the beginning of inspiration is about –5 cm of water which hold the lungs open to their resting
level.
Then, during normal inspiration creates more negative pressure, to an average of about –7.5 cm of
water.
Then, during expiration, the events are essentially reversed.
Alveolar Pressure (fig 3)
Alveolar pressure is the pressure of the air inside the lung alveoli.
When the glottis is open and no air is
flowing into or out of the lungs, the pressure in all lungs, all the way to the alveoli is equal to atmospheric
pressure, which is considered to be 0 cm water pressure. During inspiration, the pressure in the alveoli must
fall below atmospheric pressure, to about –1 cm of water which is enough to pull 0.5 L of air into the lungs
in the 2 seconds required for normal quiet inspiration.
During expiration, opposite pressures occur: The alveolar pressure rises to about +1 cm of water, and this
force the 0.5 L of inspired air out of the lungs during the 2 to 3 seconds of expiration.
Transpulmonary Pressure (fig 3)
It is the pressure difference between the alveolar pressure and the pleural pressure. It is a measure of the
elastic forces in the lung that tend to collapse the lungs at each instant of respiration, called the recoil
pressure.
Compliance of the Lungs (fig 4,5)
It is the extent to which the lungs will expand for each unit increase in transpulmonary pressure (if enough
time is allowed to reach equilibrium) and it is about 200 ml of air per cm of water transpulmonary pressure
in normal adult human being.
The compliance is oppose and determined by the elastic forces of the lungs which tend to collapse the lung.
These can be divided into two parts: (1) elastic forces of the lung tissue itself. The lung tissue elastic forces
are determined mainly by elastin and collagen fibers of lung parenchyma (2) elastic forces caused by surface
tension of the fluid that lines the inside walls of the alveoli and other lung air spaces. When the lungs are
filled with air, there is an interface between the alveolar fluid and the air in the alveoli. The water molecules
have a strong attraction for one another leading to that the water surface is always attempting to contract
which lead to force the air out of the alveoli through the bronchi and alveoli collapse. The net effect is to
cause an elastic contractile force of the entire lungs, which is called the surface tension elastic force
The tissue elastic forces tending to cause collapse of the air-filled lung represent only about one third of the
total lung elasticity, whereas the
fluid-air surface tension forces in the alveoli represent about two thirds.
Surfactant and Its Effect on Surface Tension: Surfactant is a greatly reduces the surface tension of water
because it is not dissolving uniformly in the fluid lining the alveolar surface. It is secreted by type II alveolar
epithelial cells, which constitute about 10 per cent of the surface area of the alveoli.
Surfactant is a complex
mixture of several phospholipids, proteins, and ions.
When the air passages leading from the alveoli are blocked, the surface tension in the alveoli tends to
collapse the alveoli. This creates positive pressure in the alveoli, attempting to push the air out. The amount
of pressure generated in this way in an alveolus can be calculated from the following formula:
Pressure=2* Surface tension/ Radius of alveolus
with normal surfactant, the pressure is about 4 cm of water pressure while when alveoli is lined with pure
water without any surfactant, the pressure is about 18 cm of water pressure due to increase the surface
tension when there is no surfactant.
Note from the preceding formula that the pressure generated as a result of surface tension in the alveoli is
inversely affected by the radius of the alveolus, which means that the smaller the alveolus, the greater the
alveolar pressure caused by the surface tension.
Respiratory distress syndrome of the newborn: It is the case occurs in small premature babies because:
firstly many of premature babies have alveoli radius less than one quarter that of an adult person leading to
increase the surface tension pressure. Secondly surfactant does not normally begin to be secreted into the
alveoli until between the sixth and seventh months of gestation, and in some cases, even later than that.
Therefore, many premature babies have little or no surfactant in the alveoli when they are born, leading to
increase surface tension and their lungs have an extreme tendency to collapse leading severe hypoxemia.
It is
fatal if not treated with strong measures, especially properly applied continuous positive pressure breathing.
Compliance of the Thorax and the Lungs Together
The compliance of the combined lung-thorax system is almost exactly one half that of the lungs alone—110
ml of volume per cm of water pressure for the combined system, compared with 200 ml/cm for the lungs
alone.
Figures
Figure 1: lung anatomy
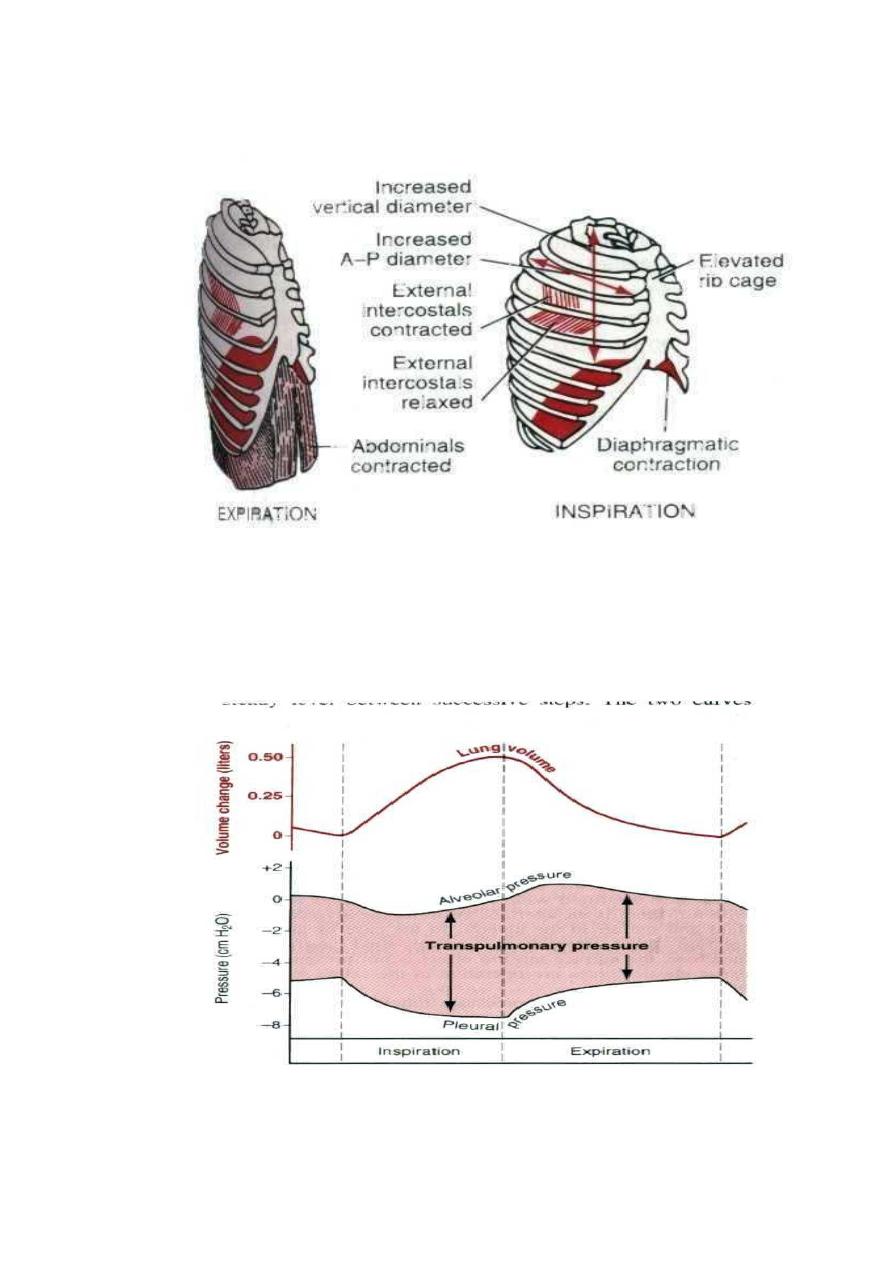
Fig 2: Contraction and expansion of the thoracic cage during expiration and inspiration.
Fig 3:
Changes in lung volume, alveolar pressure, pleural pressure, and transpulmonary
pressure during normal breathing.
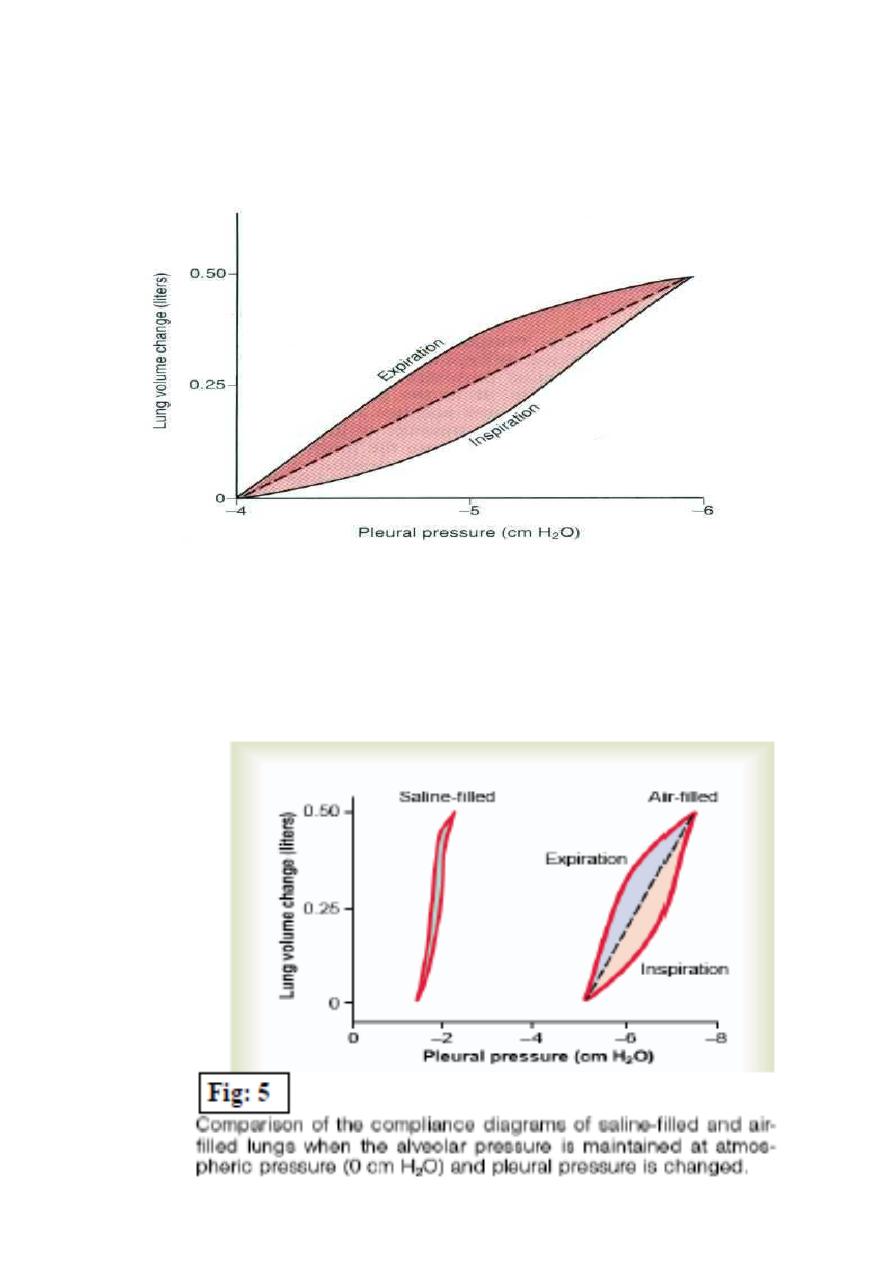
Fig 4:
Compliance diagram in a healthy person. This diagram shows compliance of the lungs
alone.
