Malignant skin tumors
Basal Cell Carcinoma-The commonest skin cancer.
-Typically affects individuals between the age of 40 and 79 years.
- more than 50% are males.
- more than 85% occur in the head and neck region. Common site in the face is above the line joining the angle of the mouth and the ear lobe. Most common site of presentation is the medial canthal area on the lower lid.
- more common in sun exposed parts of the body.
- more in fair(white)skin peoples.
- common in those who spend long time working outdoors like farmers and sailors (chronic accumulative sun exposure).
- UV light type B(in sun light) has a role as carcinogenic factors.
- basal cell carcinoma usually grow slowly, but locally invasive and penetrate deeper tissues, so it is called rodent ulcer. Metastasis is rare.
- The patient gives a history of “spot” that fails to heal.
- There are 5 clinical types of BCCs:
1.Nodular. typical presentation as a nodular appearance with a pearly rolled edge and telangiectatic vessels.
2.Superficial.
3.Cystic.
4.pigmented.
5.morphic.
-Differential diagnosis; Squamous cell carcinoma, solar keratosis, Malignant melanoma.
- Diagnosis by history, clinical examination and biopsy.
- Treatment:
1.Surgery as excision of tumor with safe margin of 2-5mm.
2.Radiotherapy.
3.Laser.
4.Cryosurgery.
5. Mohs’ surgical technique.
6.Curettes and electrodessication.
7.Chemotherapy as 5 flouro Uracil.(5FU).
- The recurrence rate is less than 10% in all modalities of treatments except with chemotherapy is about 20%. In case of Recurrent BCC the recurrence rate is about 34%.
Squamous Cell Carcinoma
-cell of origin is the keratinocytes(keratinizing epithelium, spindle cells) .
-Etiology;
1. solar radiation: chronic accumulative exposure to sun light (UV type B),so it is common in those working outdoors for long periods as farmers & sailors, & it is common in sun exposed parts of the body mainly face & hands, in the face the common site is the area below the line joining the angle of the mouth and the earlobe, 95% of SCC occur in the lower lip.
2. chemicals as smoking &spicy food.
3.chronic ulcers & skin diseases as pressure ulcers, osteomyelitis(with discharging sinus), old scars(results in SCC called Marjolin’s ulcer), radiation dermatitis, Discoid lupus erythematosis, solar (actinic) keratosis,-----e.t.c.
4.hereditary factors: as SCC is common in those with blue eyes &fair skin, also is common in those with Xeroderma pigmentosa & Albinism.
Premalignant conditions are;
1.Leukoplakia.2. Solar keratosis.
3. Bowen’s disease(SCC in situ).
4.Radiation dermatitis.
5.Xeroderma pigmentosa.
-Types: Clinical types:
1.Slow growing type, verrucous nature, exophytic. It is locally invasive & could metastasize.
2.Rapid growing type, nodular and indurated. Early ulcerate with local invasion & high rate of metastasis.
-Histopathological types:
1.Well differentiated type with high survival rate(CL.1).
2.poorly differentiated type with poor prognosis(CL.2).
-Metastasis: local invasion & destruction, lymphatic, and hematogenous metastasis.
-D.D.; solar keratosis, Keratoacanthoma, BCC, Chronic skin diseases.
-Diagnosis: history, clinical examination & biopsy.
-Treatment: same modalities used for BCC, but with surgery the safe margin is 1cm in the face & 7cm in other areas of the body.
Malignant Melanoma
-cell of origin is Melanocytes.
-etiology; sun light mainly type C.
-common in sun exposed parts.
-premalignant conditions are naevi(different types), Lentigo maligna.
-Clinical types:
1.Suprerficial spreading type. With high 5-year survival rate(90%).
2.Nodular type. With 5-year survival rate less than40%.
3.Lentigo maligna melanoma. Common in old age people and sun exposed parts.
4.Acral lentigenous melanoma. Common in black skin peoples, mucocutaneous junctions(lips & perianal areas), palm and sole.
5.Amelanotic melanoma.
-Histological grading:
Clark’s levels:
I within the Epidermis.
II within the papillary dermis.
III at interface between papillary and reticular dermis.
IV at level of reticular dermis.
V invades to the subcutaneous tissue.
Breslow’s thickness(levels):
- less than 0.76mm.
- 0.76-1.5mm.
- 1.5-4mm.
- More than 4mm.
Metastases:
1-Locally invasive.
2.lymphatic to the regional lymph nodes, melanoma in-transit is a pigmented lesion between the original lesion & the regional lymph nodes (which indicate presence of malignant cells in lymphatic vessels).
3.Hematogenous
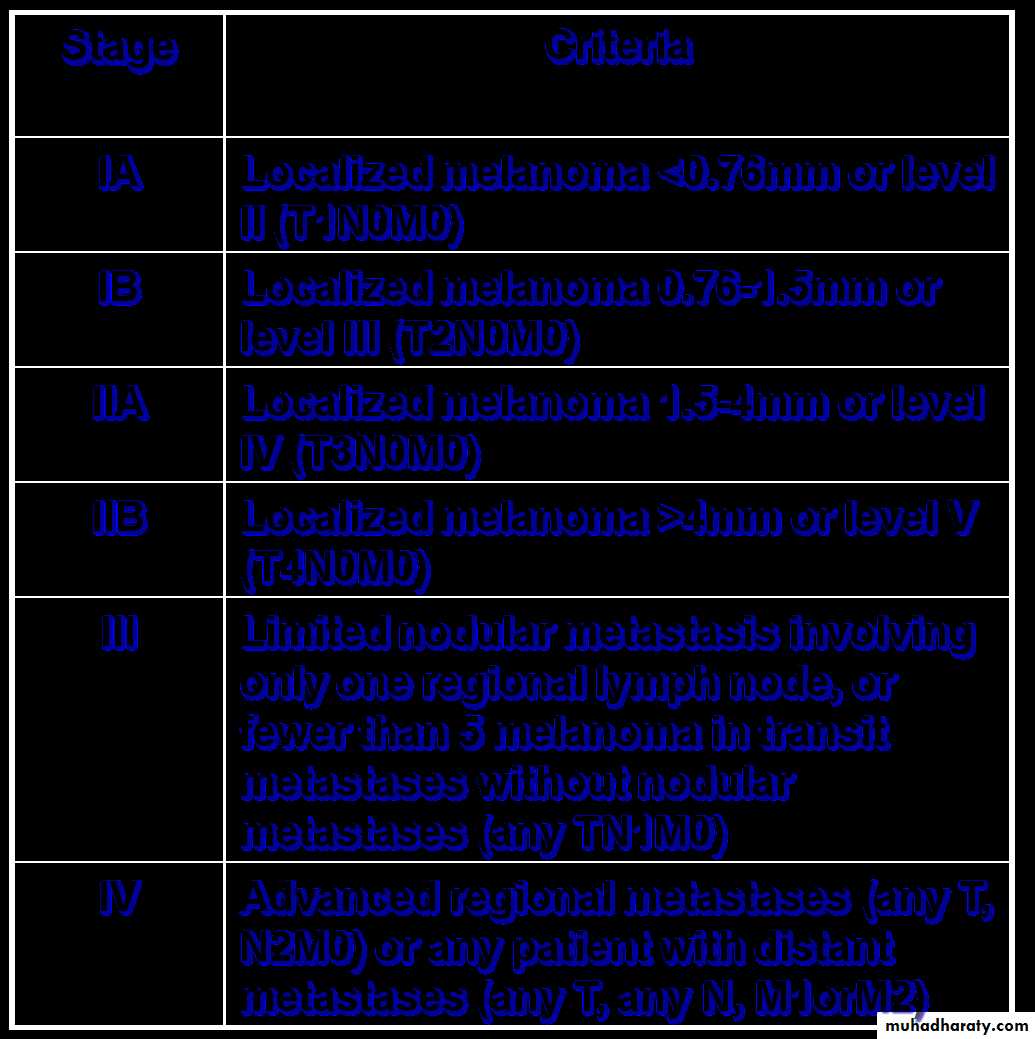
Staging
D.D; pigmented BCC, Naevi.
Diagnosis; History, clinical examination, and biopsy.
Treatment:
1.Surgical excision. safe margin 3cm.
2.Radiation.
3.Chemotherapy.
4.Immunotherapy.
This Lecture Collected By Omer Ahmed Al-Samrrai, 5th Grade of T.U.C.O.M