Dilatation of the bowel
Causes of bowel dilatation
1. Mechanical SB obstruction :
small bowel dilation with normal or reduced caliber of colon
2. Mechanical LB obstruction:
dilated colon down to the point of obstruction. May be accompanied by small
bowel dilation if the ileocecal valve becomes incompetent
3. Generalized paralytic ileus:
SB and LB dilatation, gas may be present in the rectum
4. Localized peritonitis:
dilatation of loops adjacent to inflammatory process (sentinel loops)
5. Closed loop obstruction :
e.g. cecal and sigmoid volvulus
6. Toxic dilatation of the colon:
the dilatation is maximal in transverse colon more than 6 cm
The haustra are lost or grossly abnormal . Ulcerative colitis is the commonest cause
7. SB infarction :
mimic obstruction of SB or LB depending on distribution of ischemia
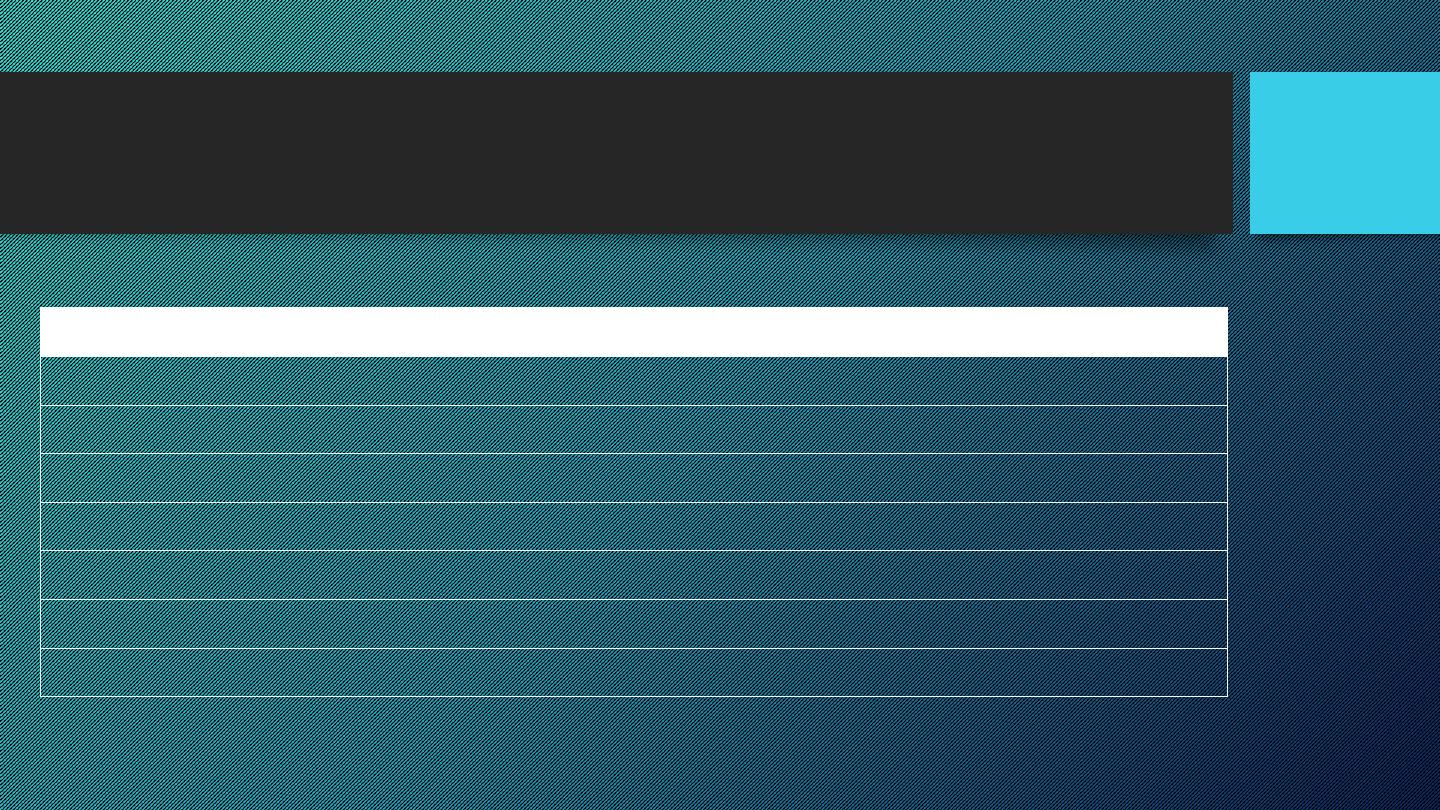
Dilatation of the bowel
Small bowel obstruction
Large bowel obstruction
Valvulae conniventes
Present
Absent
Number of loops
Many
Few
Distribution of loops
Central
Peripheral
Haustra
Absent
Present
Diameter
3 – 5 cm
More than 5 cm
Radius of curvature
Small
Large
Fecal material
Absent
Present
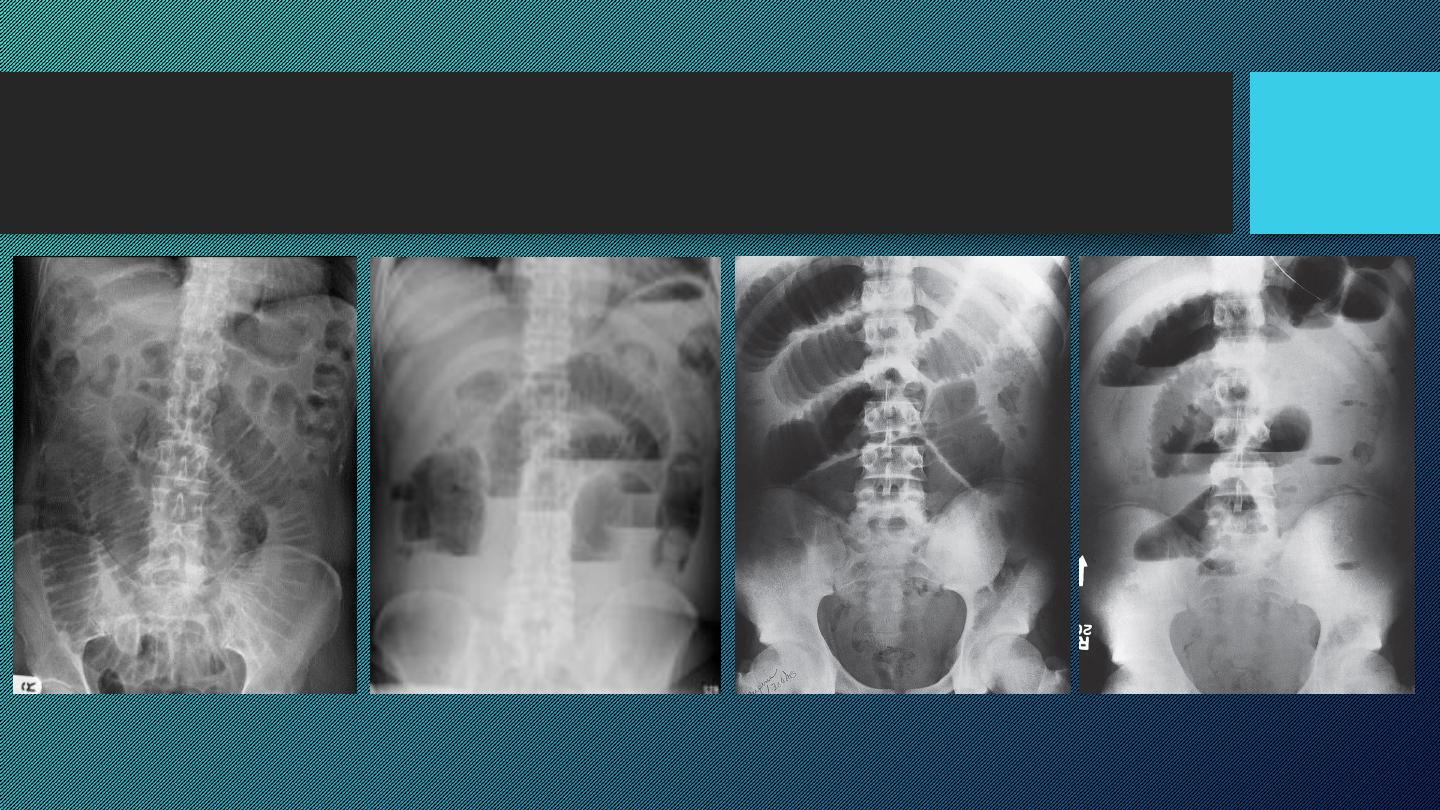
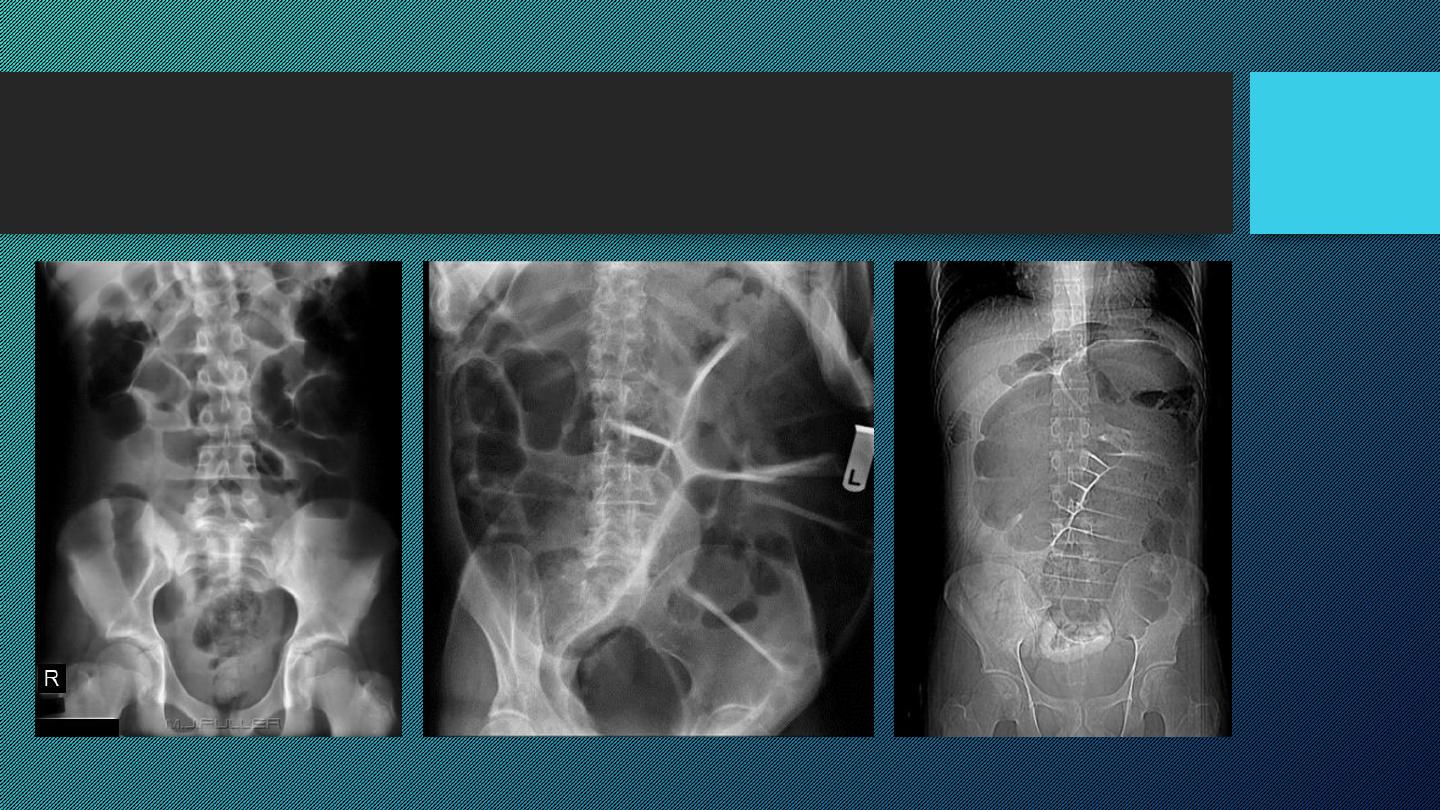
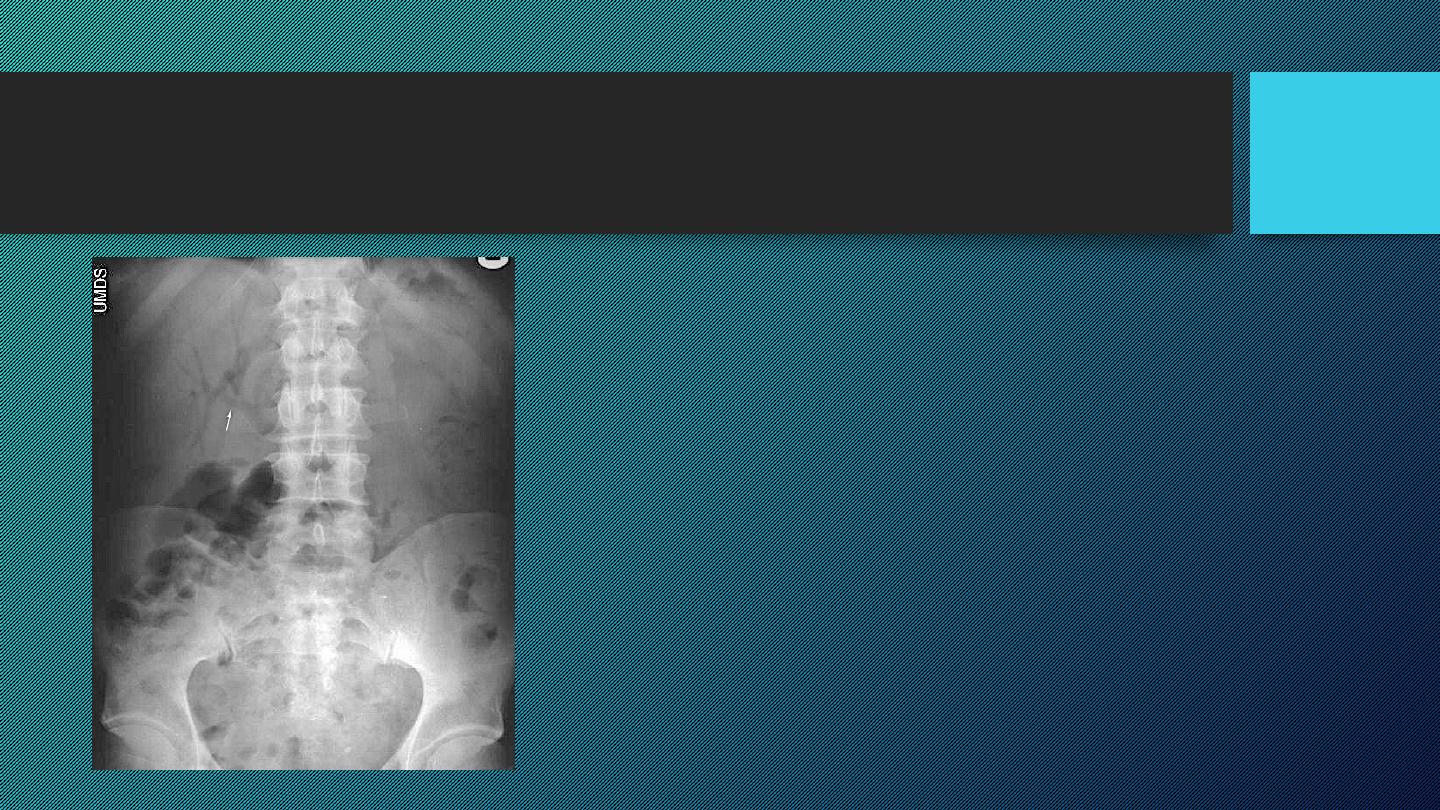
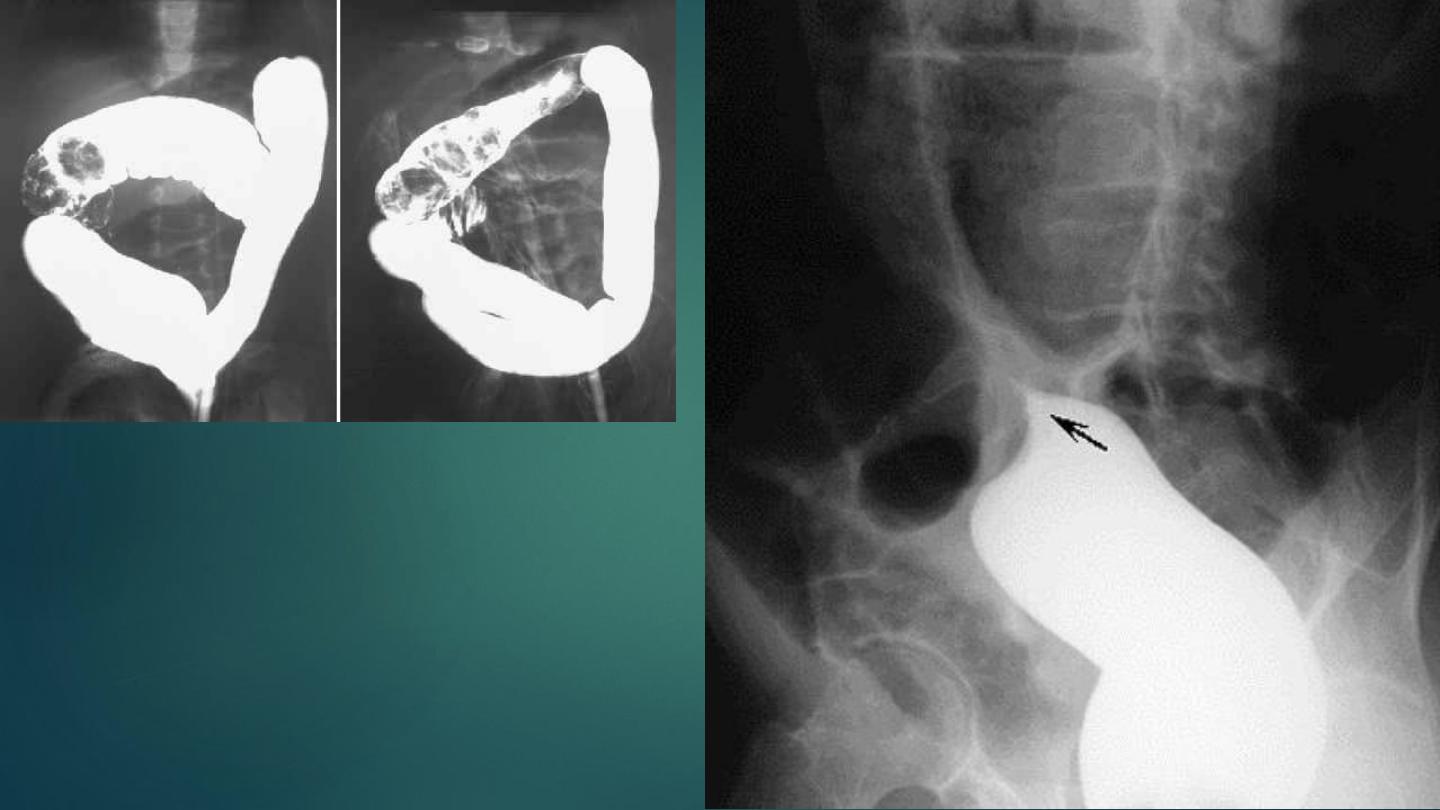
SMALL INTESTINAL OBSTRUCTION
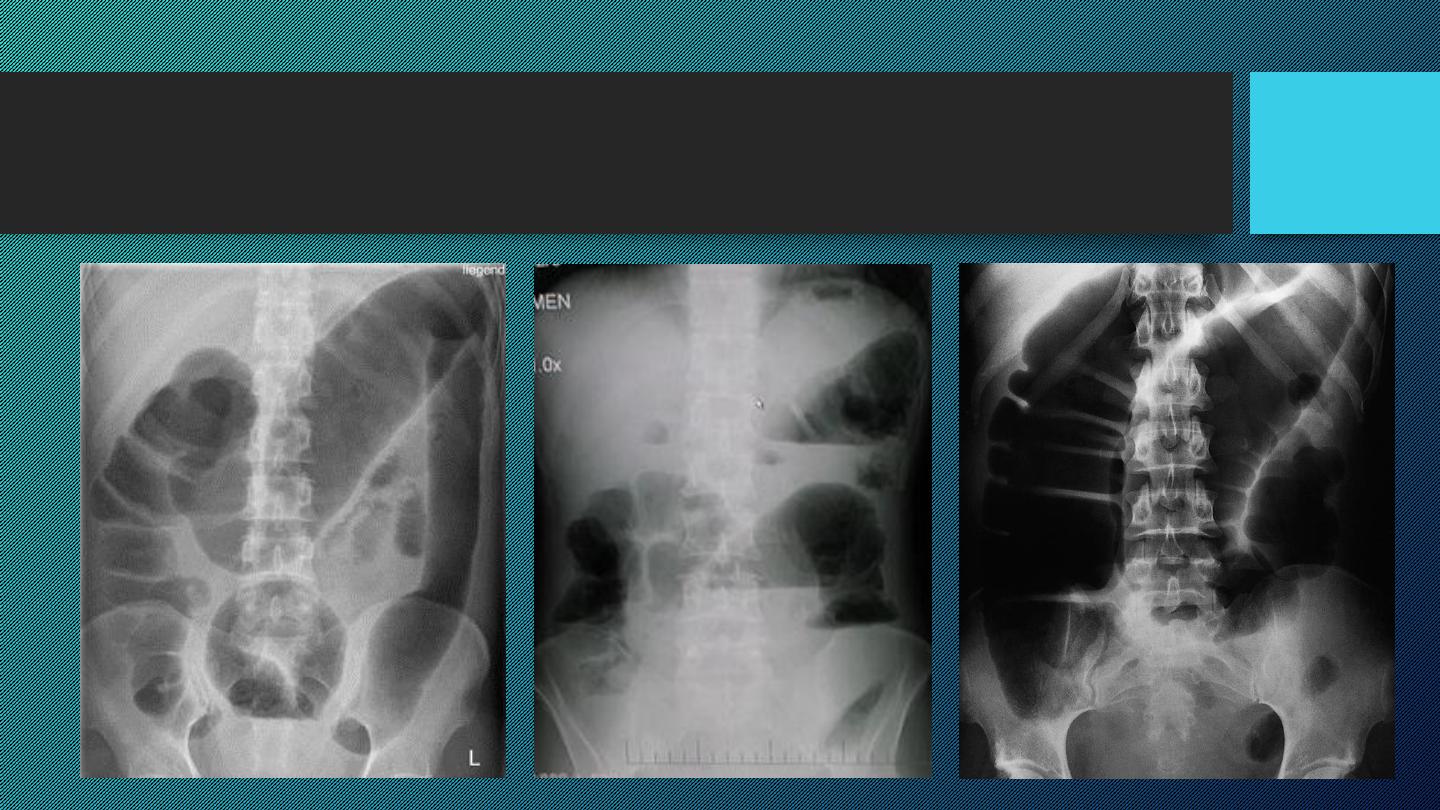
LARGE INTESTINAL OBSTRUCTION
Dilatation of the bowel
Dilatation of the bowel

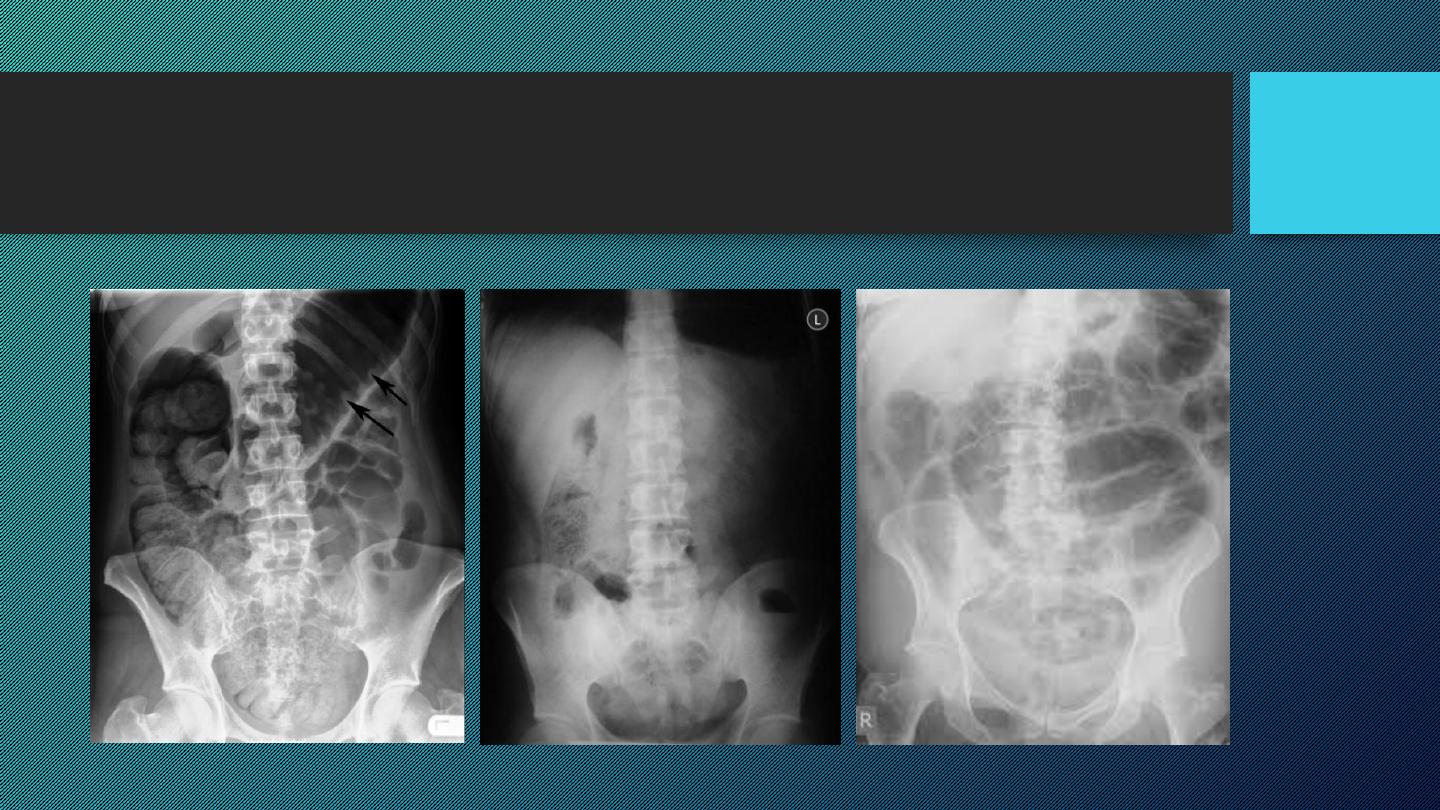
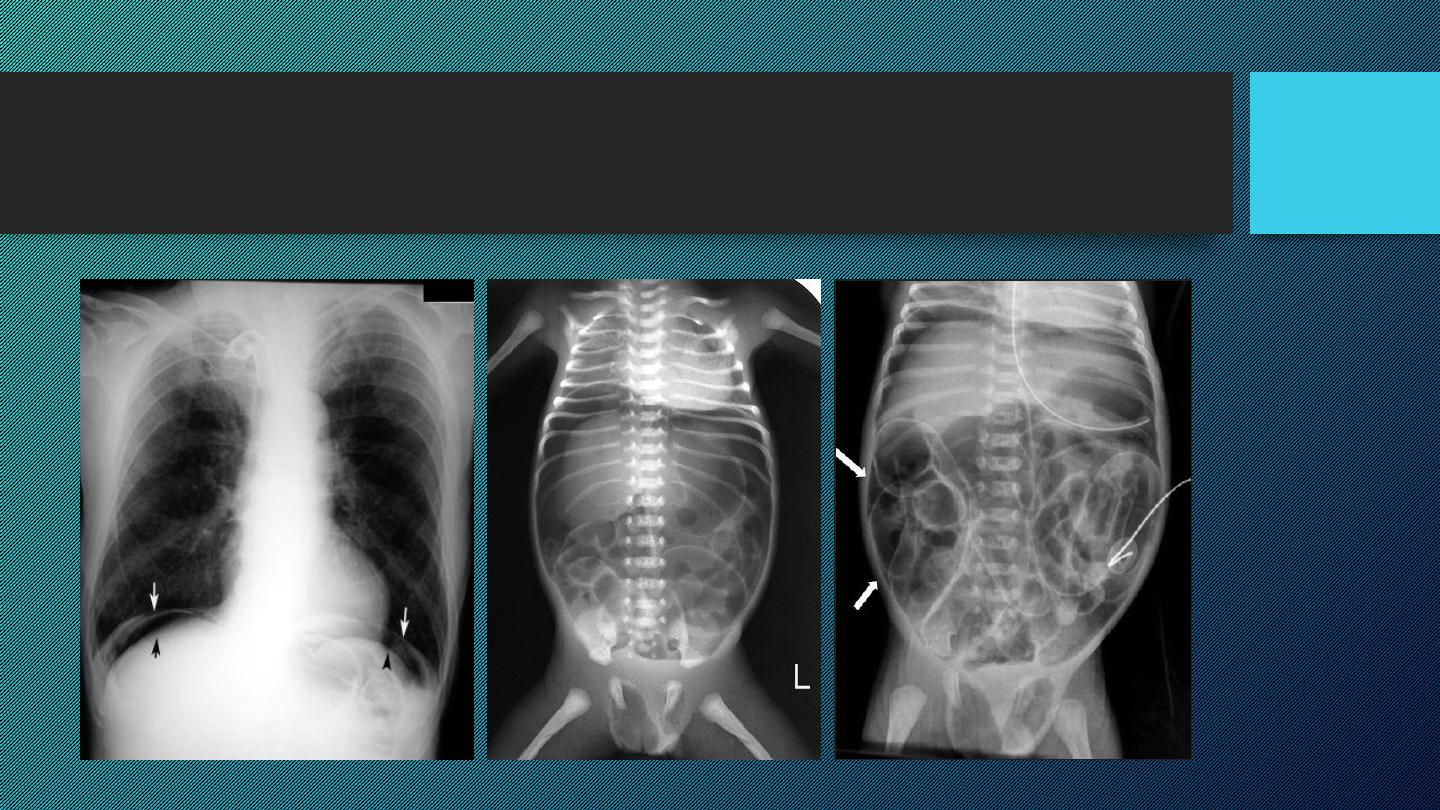
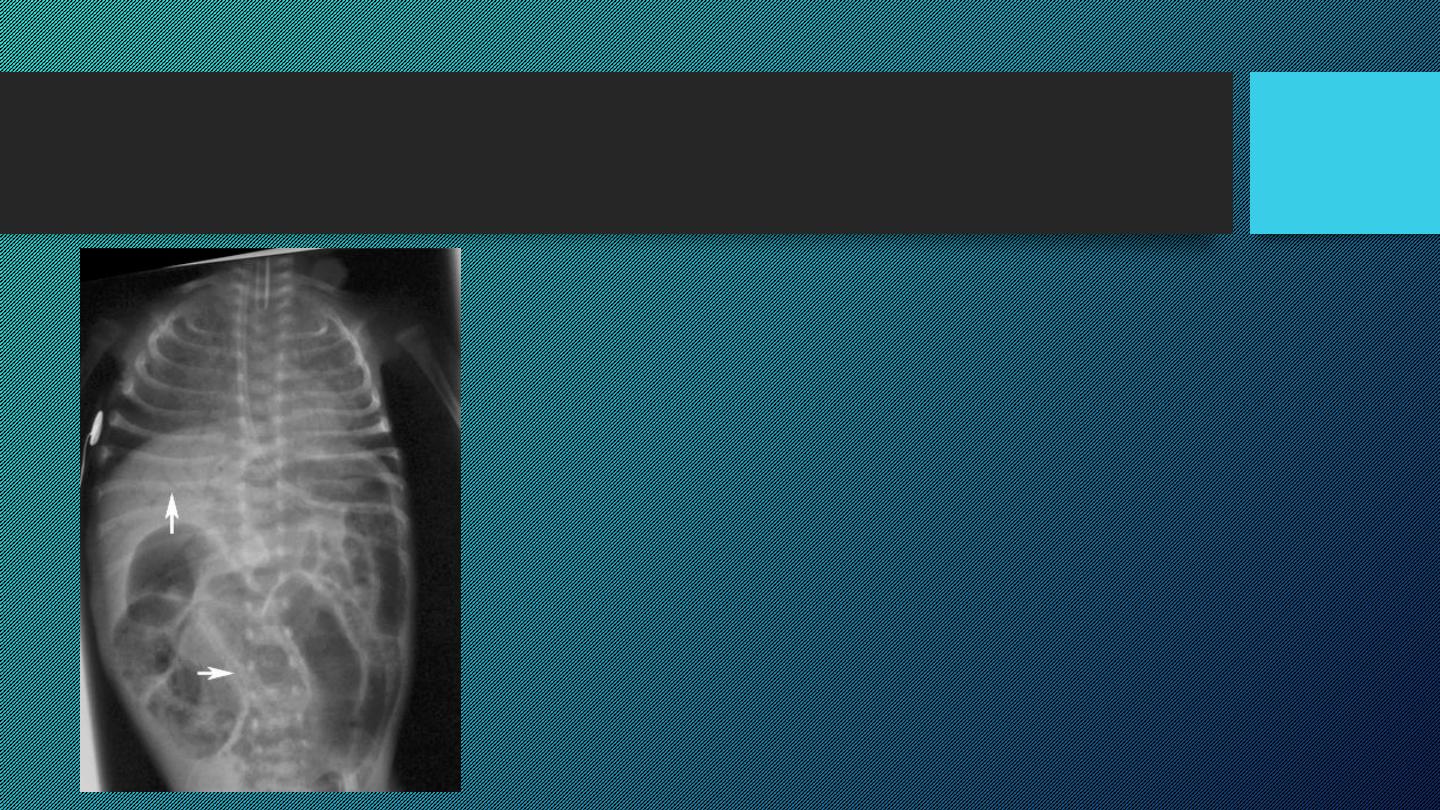
Gas in the wall of the bowel
• Spherical or oval bubbles
of gas are seen in wall of LB in adults in
pneumatosis coli
• Linear streaks
of intramural gas usually indicate
infarction
of the bowel wall
• Gas in the wall of bowel in neonates, whatever its shape, is diagnostic of
necrotizing enterocolitis
Gas in the wall of the bowel
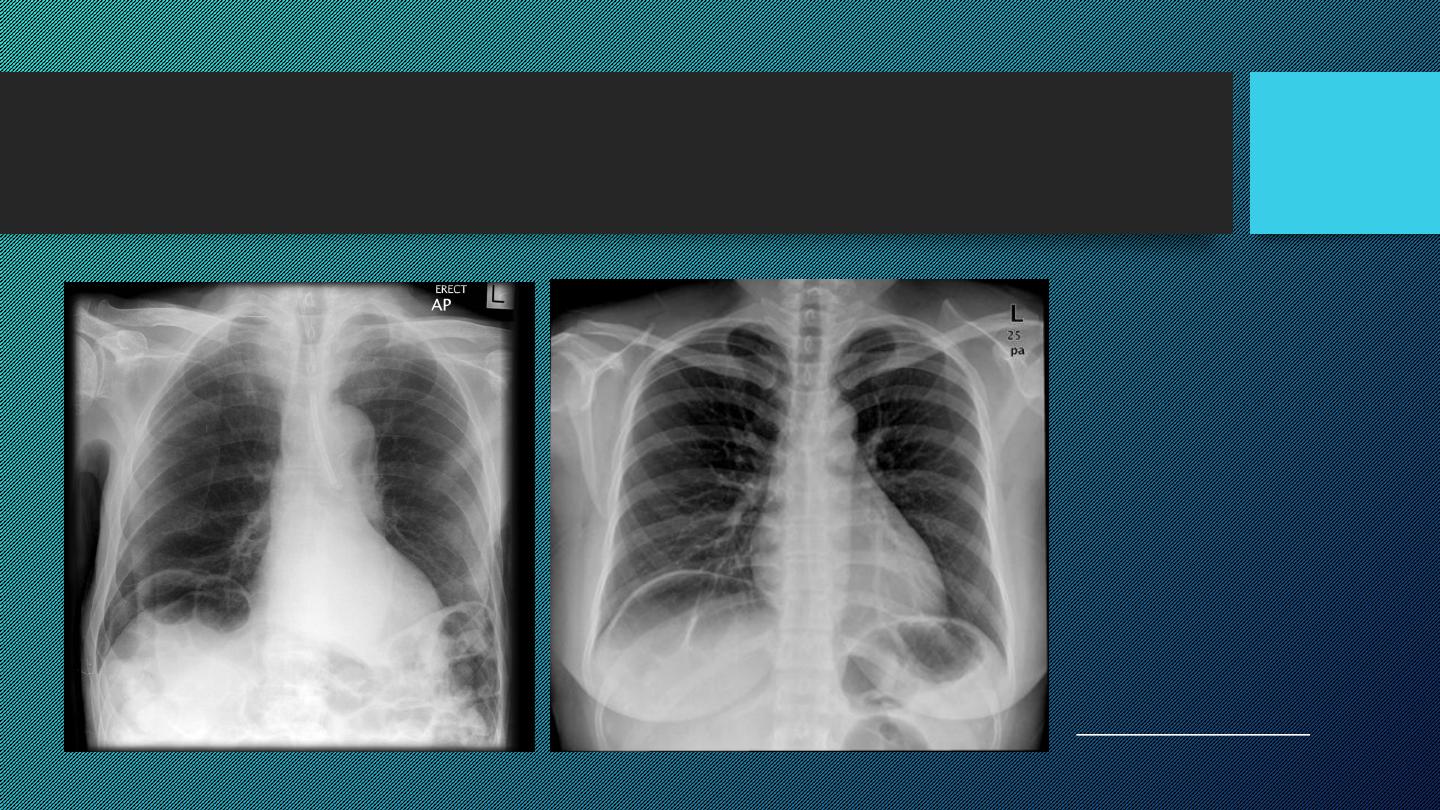
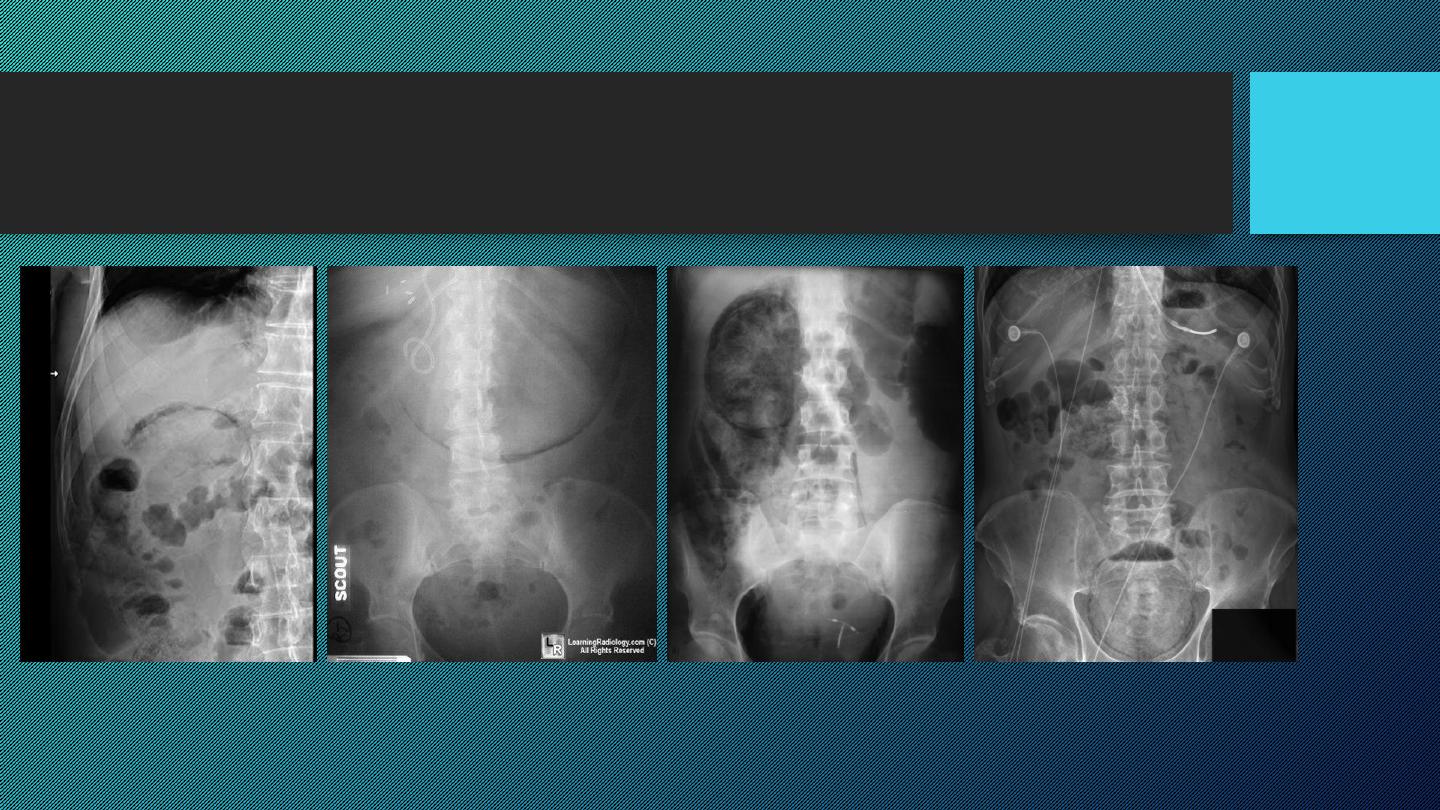
Pneumoperitoneum
• Defined as free gas in the peritoneal cavity
• The commonest cause is
perforated peptic ulcer
and
two-thirds
of such cases are recognizable radiologically
• Free intraperitoneal air is a normal finding after a laparotomy or laparoscopy.
• In adults, the air is usually absorbed within 7 days .
• In children, the air absorbs much faster ,usually within 24 hours.
• An increase in the amount of air on successive films indicates continuing leakage of air.
• Pneumoperitoneum under the right hemidiaphragm is usually easy to recognize, but free gas under the left
hemidiaphragm is difficult to recognize because of the overlapping gas shadows of the stomach and splenic flexure.
• Gas under the diaphragm is much easier to diagnose on an
erect chest film
than on an upright abdominal film
Pneumoperitoneum
Pseudopneumoperitoneum
Chilaiditi syndrome
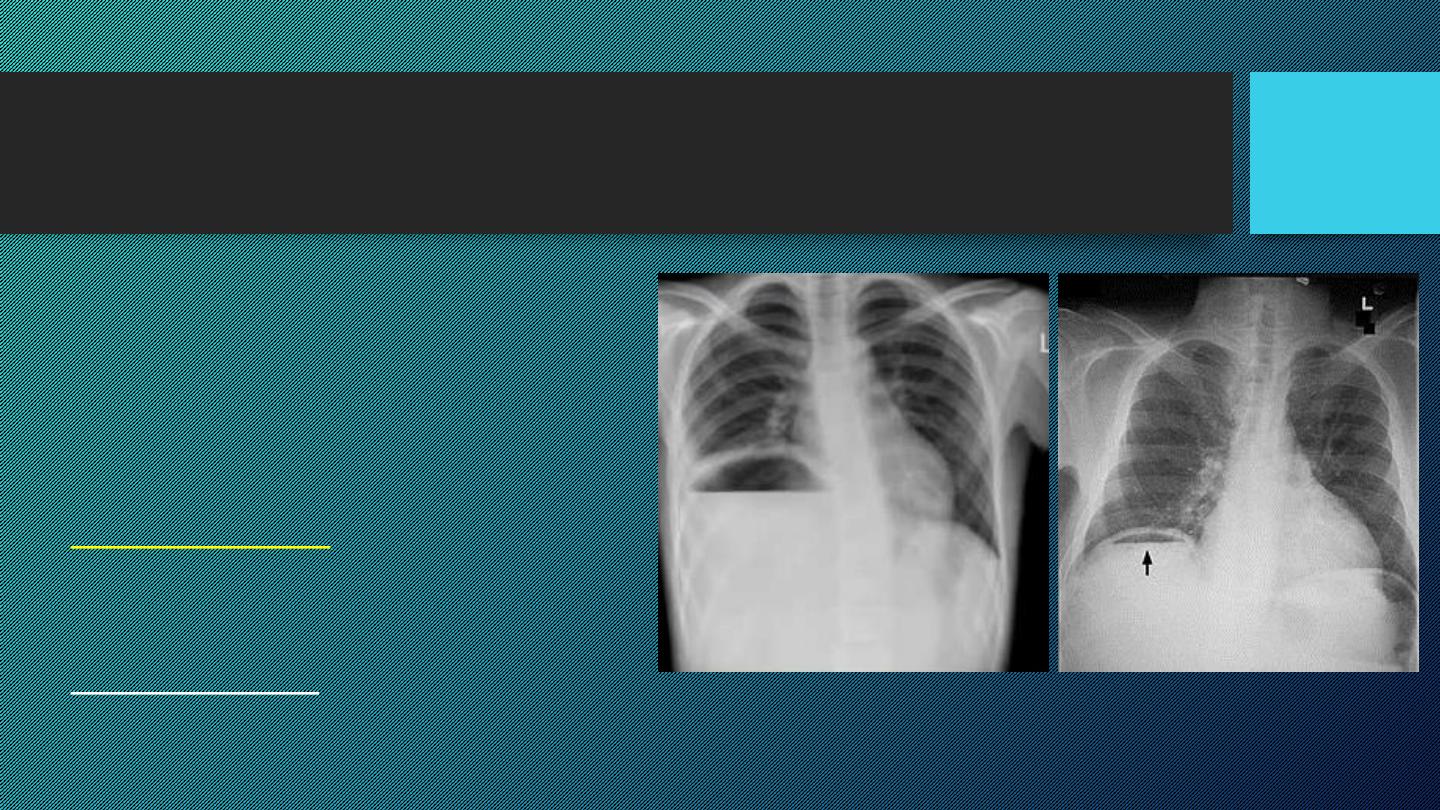
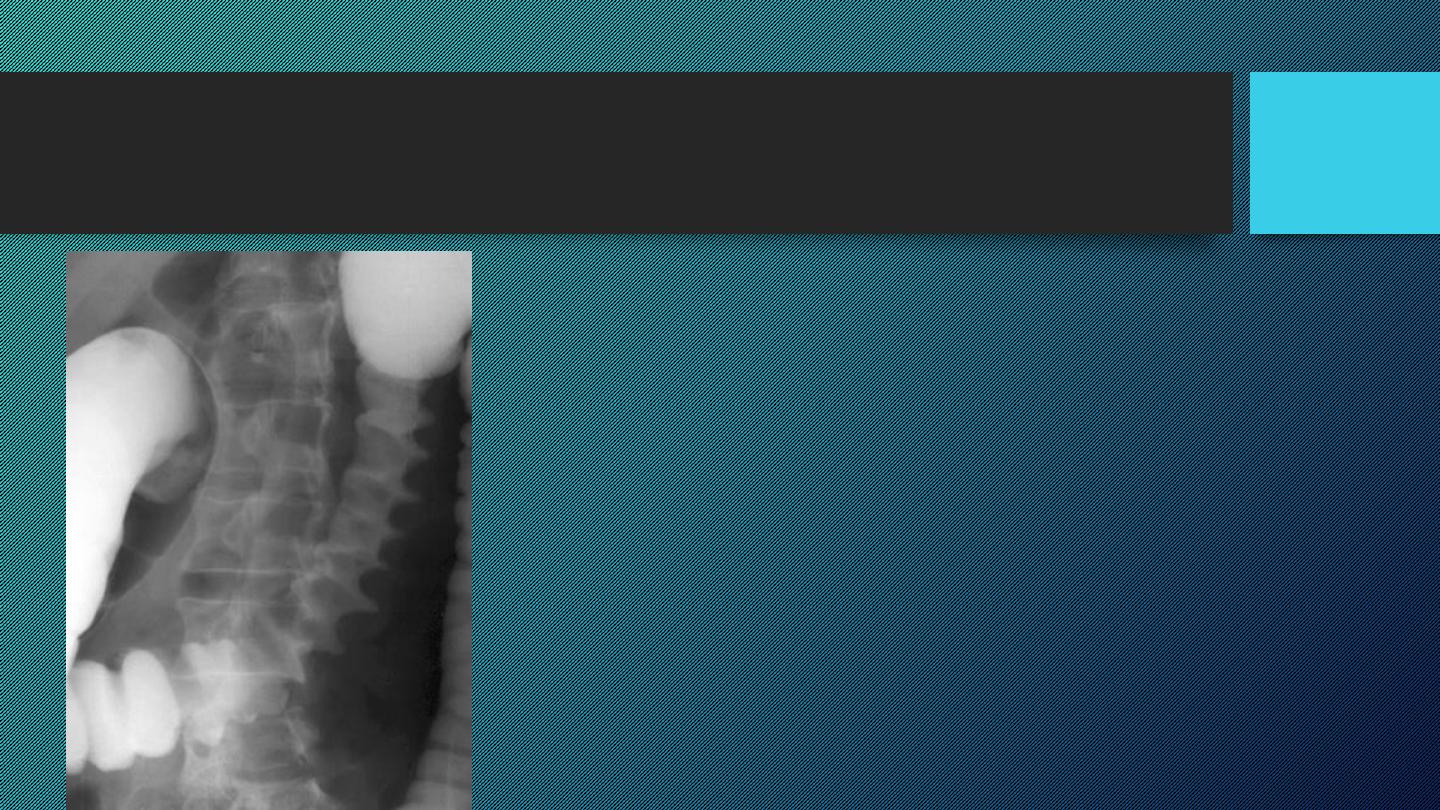
Gas in an abscess
It may form either small bubbles or larger
collections of air , both of which could be
confused with gas within the bowel.
Fluid levels in abscesses may be seen on a
horizontal x-ray film.
Subphrenic abscess
cause elevation of the
diaphragm, pleural effusion and pulmonary
collapse/consolidation
Ultrasound and CT are extensively used to
evaluate abdominal abscesses
Gas in the biliary system
Gas in the portal vein
Tissue emphysema
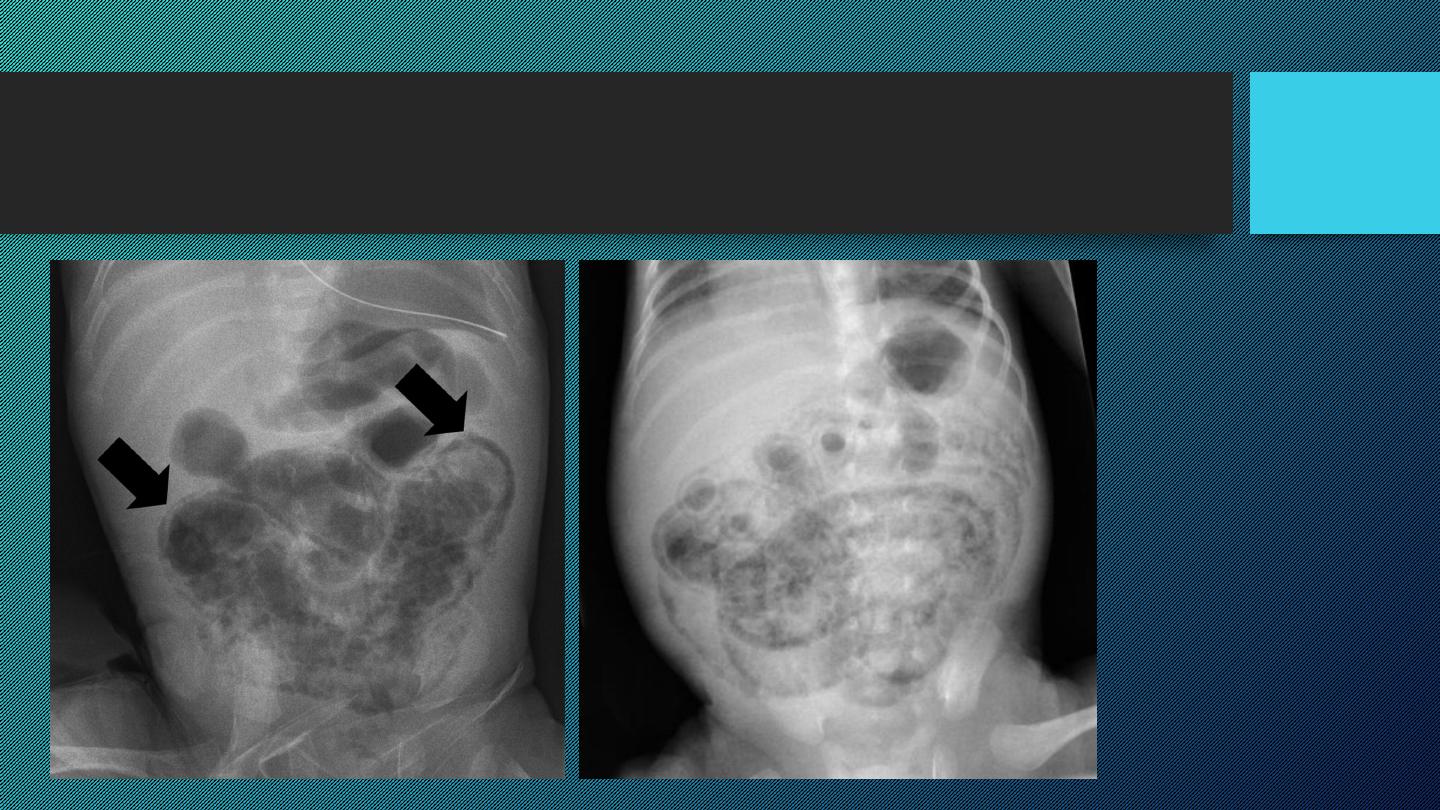
ISCHEMIC COLITIS

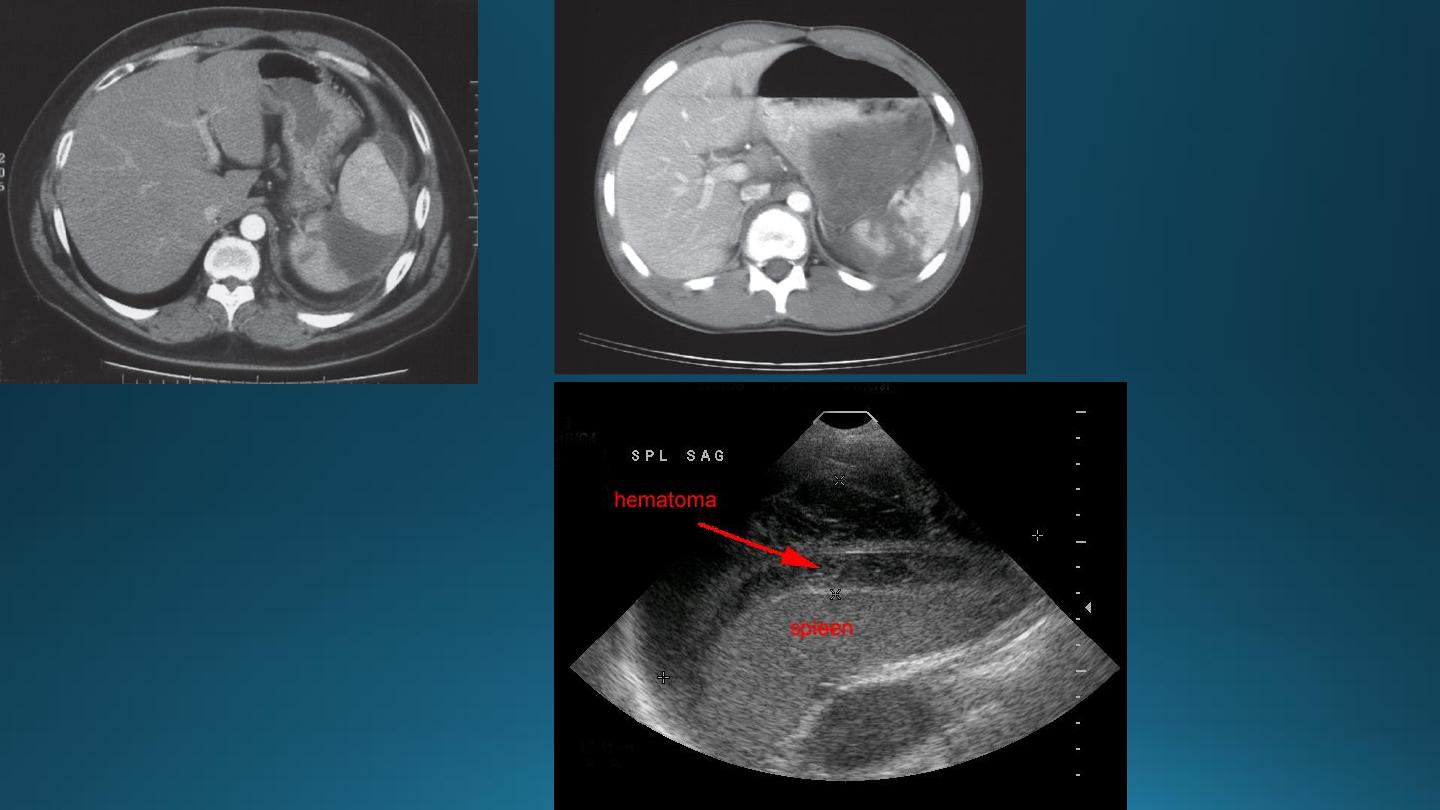
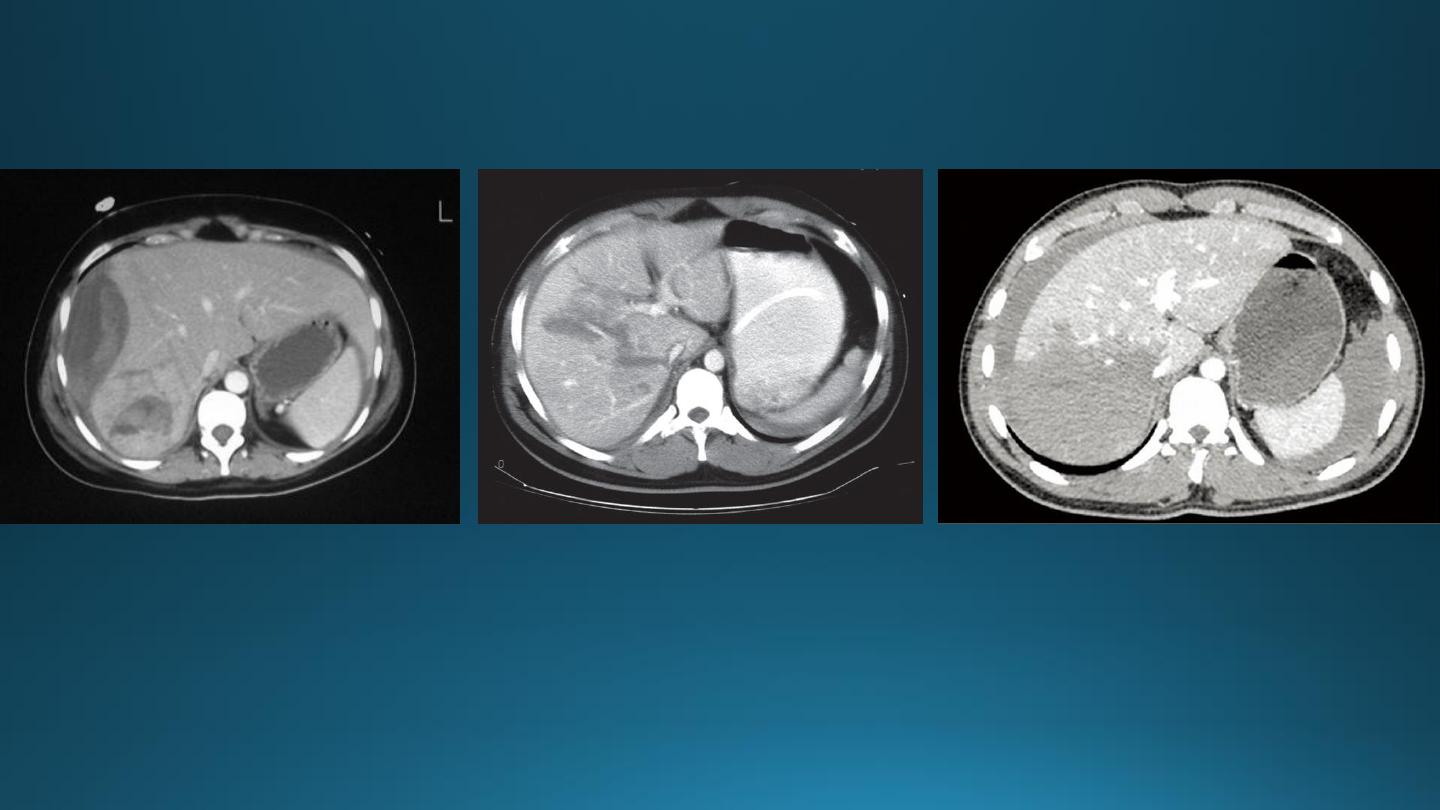
LIVER TRAUMA
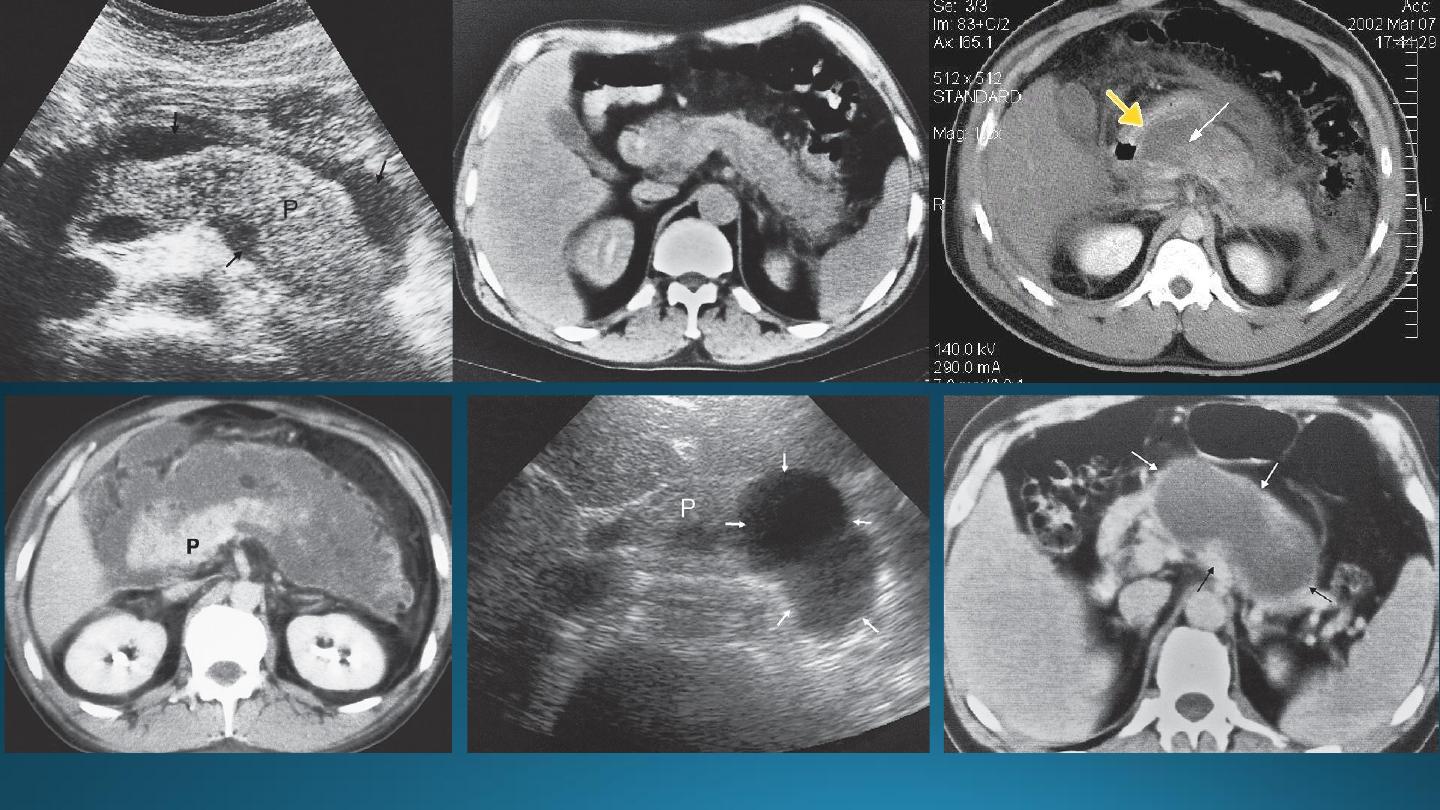
Trauma to the liver is the commonest abdominal injury that leads to death.
Parenchymal lacerations are the most frequent injury, often accompanied by subcapsular and intrahepatic hematoma.
US has become part of the standard assessment.
Focused Assessment with Sonography for Trauma "(FAST scan)
It is a rapid bedside examination which examines four areas for free fluid:
• Perihepatic and hepatorenal space
• Perisplenic
• Pelvis
• Pericardium
CT
• It is more sensitive and specific.
• Lacerations and hematomas are recognized as low density areas relative to the normal intact, enhanced
parenchyma.
• Leakage of contrast indicate active bleeding
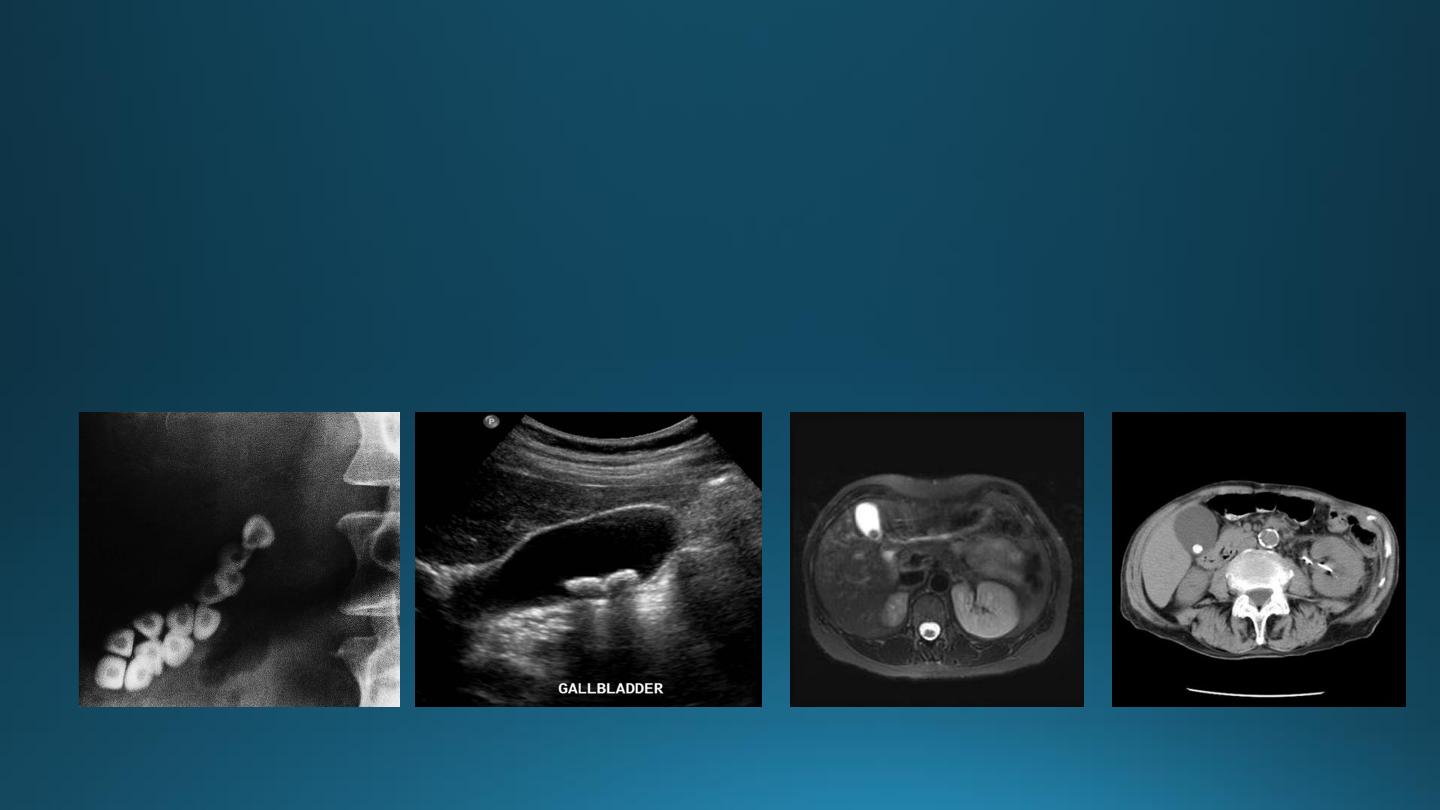
GALL STONES
• Gall stones are more frequent in middle age females.
• 20% of gall stones are visible on plain film.
• On US, stones are strongly echogenic with acoustic shadow (which is not seen with polyps).
• US is not reliable for detecting stones in CBD which are better demonstrated by MRCP
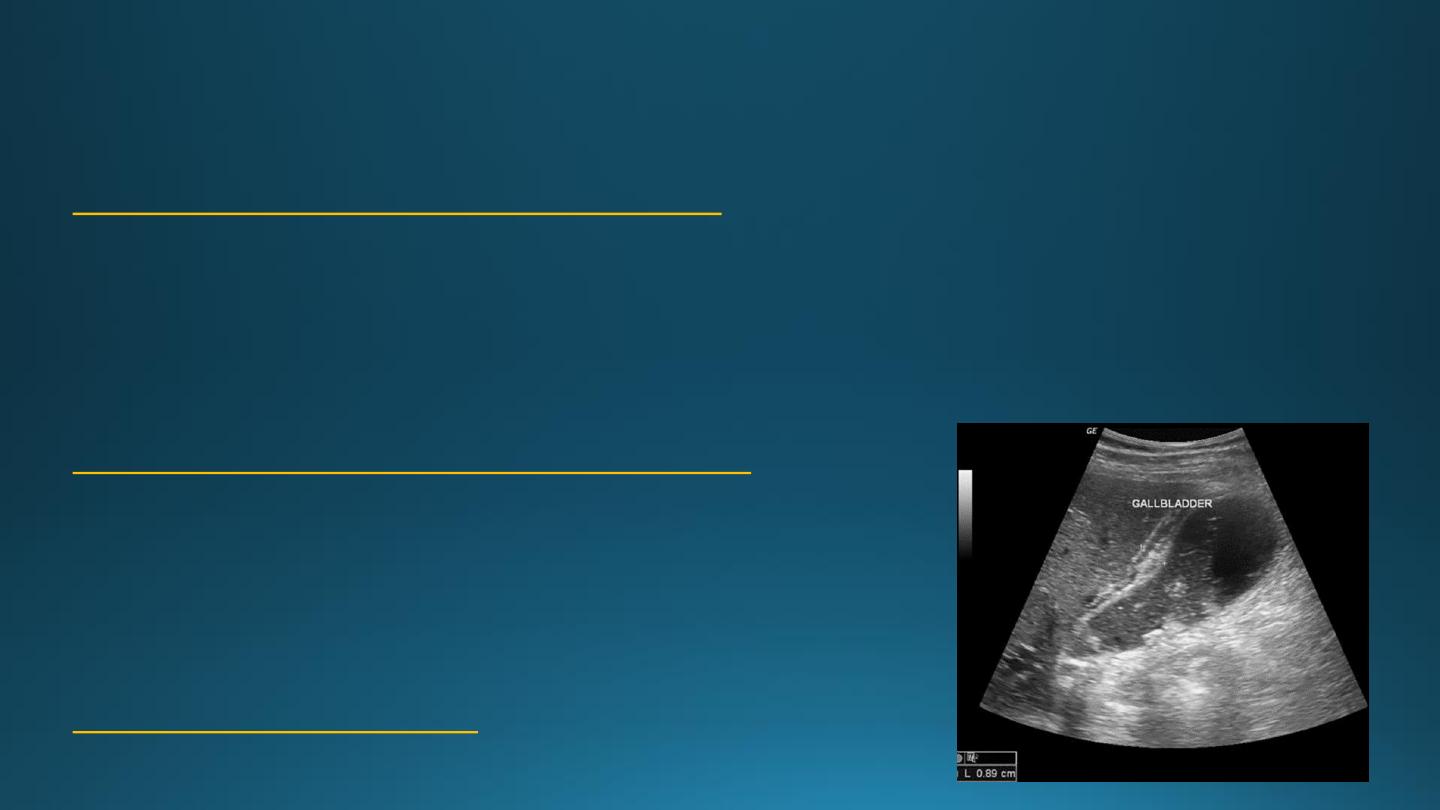
CHOLECYSTITIS
US features of early or uncomplicated acute cholecystitis:
1. Gall stones (which may be impacted in the GB neck or cystic duct)
2. Gall bladder wall thickening
3. Gall bladder distension
4. Positive sonographic Murphy's sign (focal tenderness over the GB when compressed by the US transducer)
US features of advanced or complicated acute cholecystitis:
1. Pericholecystic fluid collection
2. Striated appearance of the thickened GB wall
3. Intraluminal membranes caused by sloughed GB mucosa
4. Gas in GB wall or lumen resulting in emphysematous cholecystitis
US features of chronic cholecystitis
are thick wall and GB contraction
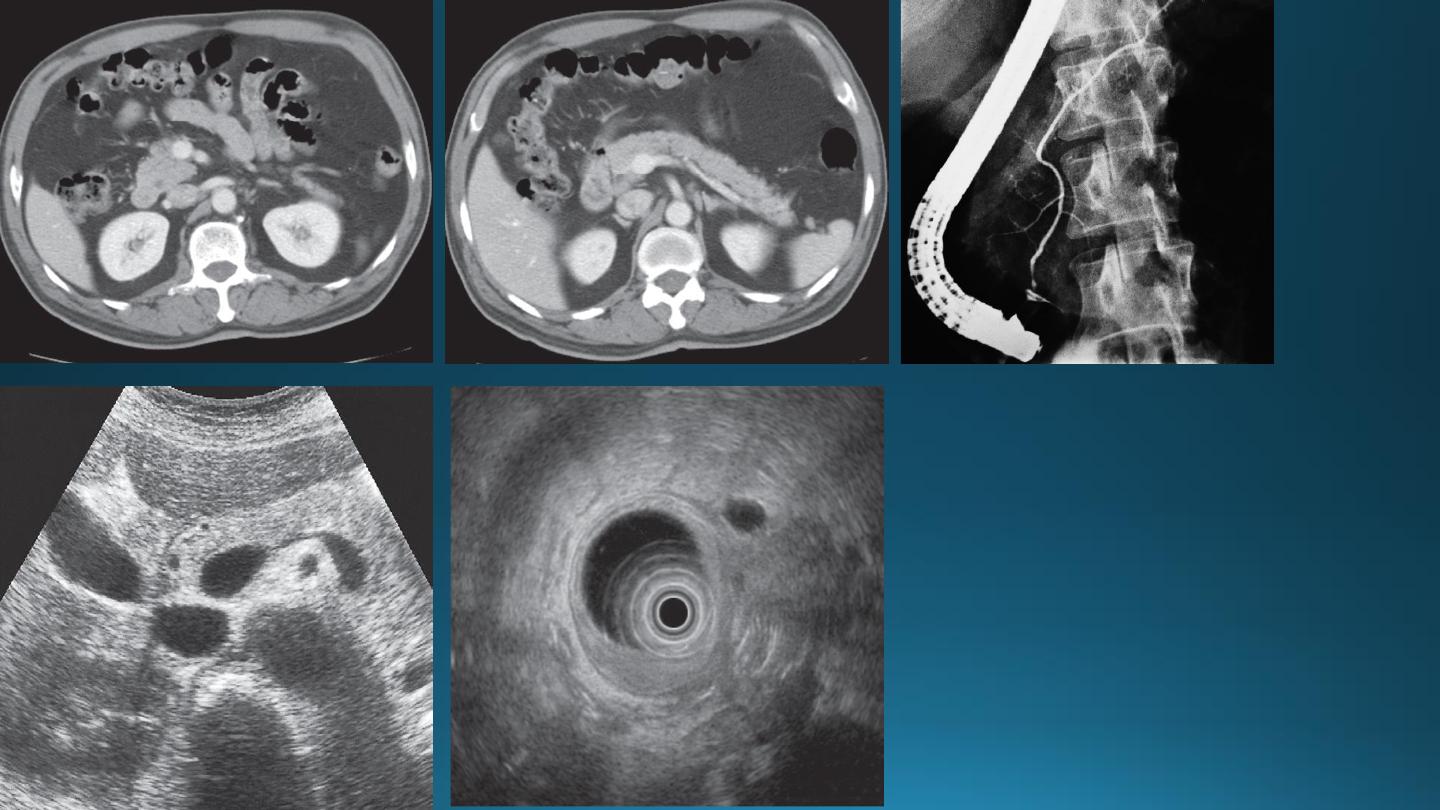
ACUTE PANCREATITIS
The pancreas is usually enlarged, often diffusely with irregular outlines due to extension of inflammatory process
into the surrounding fat. There may be low density areas at CT or echo-poor areas at US (edema and necrosis)
The diagnosis is usually made on clinical and biochemical grounds
The purpose of CT is to assess the severity and complications:
1. Pancreatic necrosis (areas with no enhancement)
2. Abscess appear as fluid collection which may contain gas
3. Vascular complications e.g. Splenic vein thrombosis, arterial erosion & pseudoaneurysm
4. Pseudocysts occur as a result of leak of pancreatic secretions that are contained in a cyst like manner within
and adjacent to the pancreas.
They can be demonstrated with CT or US as thick or thin walled cysts of variable sizes.
Many pseudocysts resolve in the weeks following an attack of acute pancreatitis, some persist and may need
surgical or percutaneous drainage.
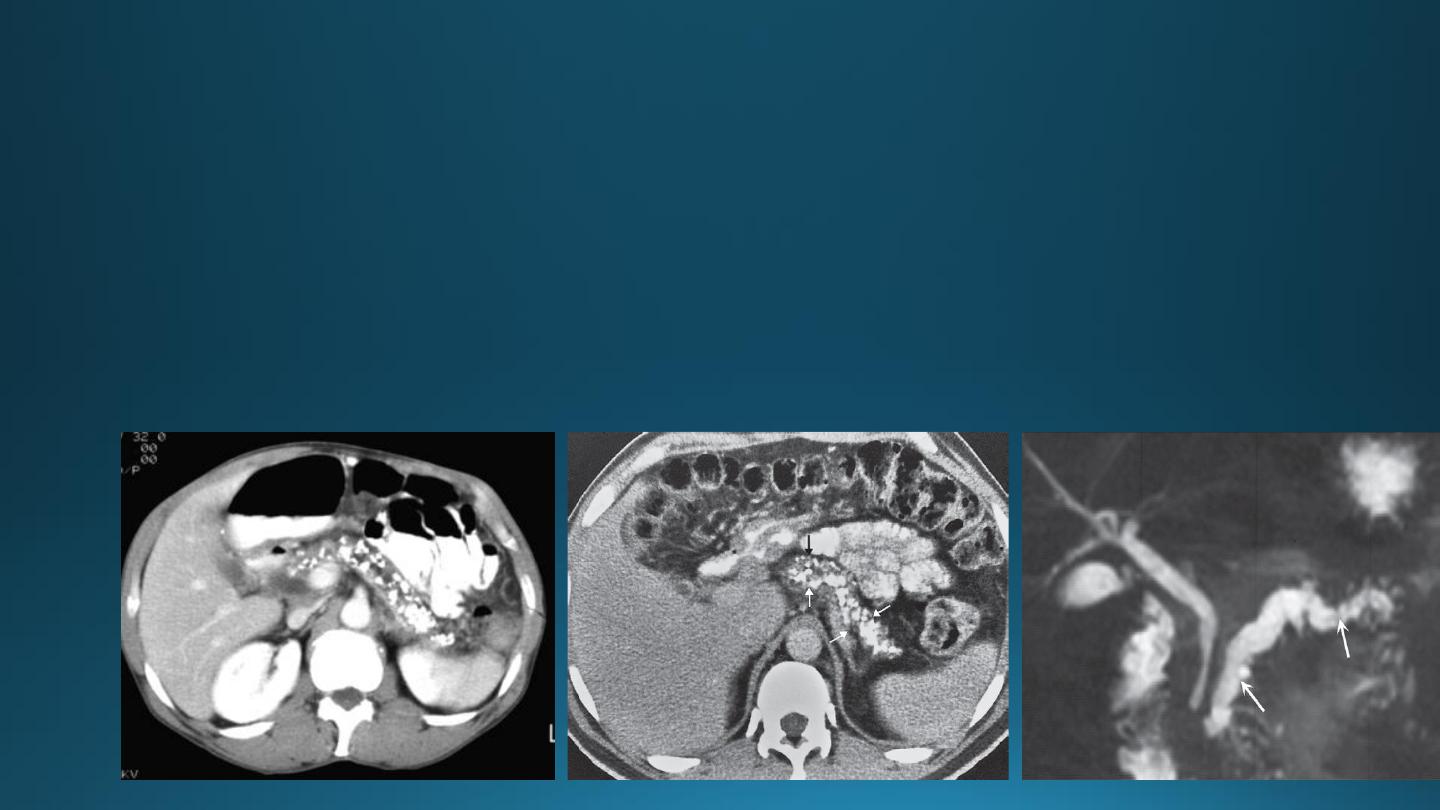
CHRONIC PANCREATITIS
• It result in fibrosis, calcifications, and ductal stenosis and dilatation.
• Pseudocysts are seen.
• The calcification often recognizable on plain x ray film, but more obvious on CT.
• The gland may enlarge focally or generally.
• The gland may atrophied.
• The pancreatic duct may be enlarged and irregular.
SPLEEN
Splenic infarction
• Secondary to severe pancreatitis
• Pancreatic carcinoma
• Sickle cell and trauma
It show focal or complete loss of normal enhancement following IV contrast
Splenic trauma
• The spleen is the most commonly injured organ in blunt trauma.
• CT is the superior method of investigation.