Anatomy of Female Reproductive Organs
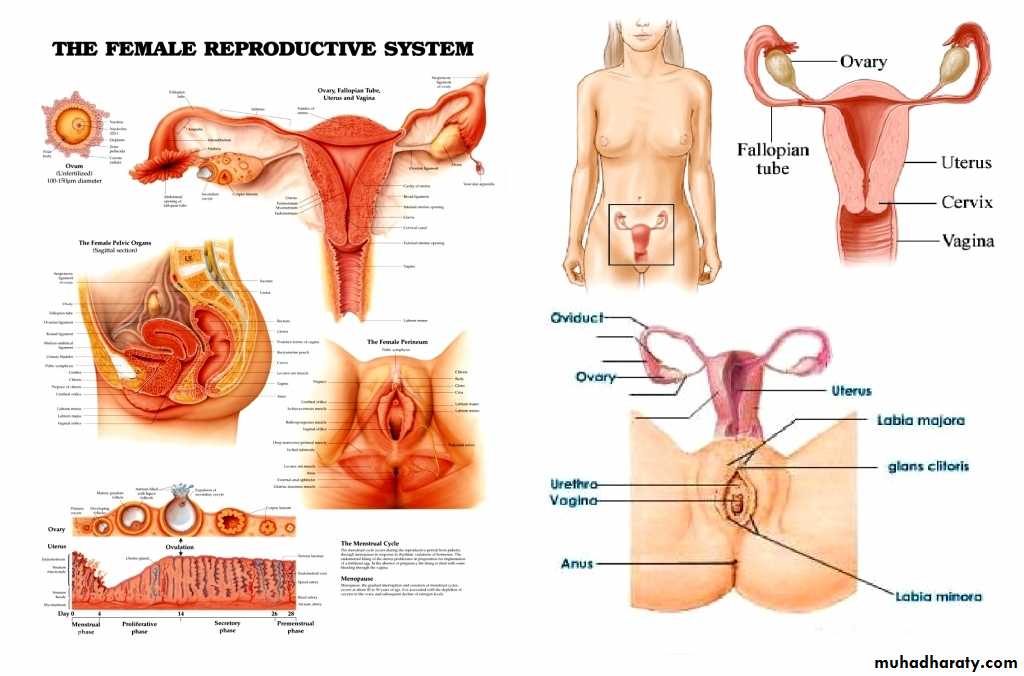
The reproductive organs in female are those which are concerned with copulation, fertilization, growth and development of the fetus and its subsequent exit to the outer world.EXTERNAL GENITALIA
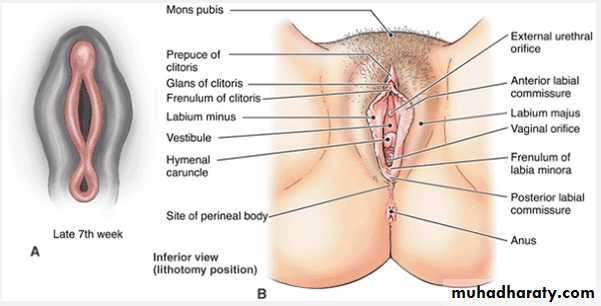
The vulva or pudendum includes all the visible external genital organs in the perineum
Vulva consists ofthe following
The mons pubis, labia majora, labia minora, hymen, clitoris, vestibule, urethra and Skene’s glands, Bartholin’s glands and vestibular bulbs . It is therefore bounded anteriorly by mons pubis, posteriorly by the rectum, laterally by the genitocrural fold.
MONS VENERIS (MONS PUBIS): It is the pad of subcutaneous adipose connective tissue lying in front of the pubis and in the adult female is covered by hair
LABIA MAJORA: The vulva is bounded on each side by the elevation of skin and subcutaneous tissue which form the labia majora. . The skin on the outer convex surface is pigmented and covered with hair follicle. The thin skin on the inner surface has sebaceous glands but no hair follicle. The labia majora are covered with squamous epithelium and contain sweat glands.. The round ligament terminates at its upper border.
LABIA MINORA: They are two thin folds of skin, devoid of fat, on either side just within the labia majora. Anteriorly, they divide to enclose the clitoris and unite with each other in front and behind the clitoris to form the prepuce and frenulum respectively. The lower portion of the labia minora fuses across the midline to form a fold of skin known as fourchette. It is usually lacerated during childbirth. Between the fourchette and the vaginal orifice is the fossa navicularis. The labia minora contain no hair follicles or sweat glands. The folds contain connective tissues, numerous sebaceous glands, erectile muscle fibers and numerous vessels and nerve endings.
CLITORIS: It is a small cylindrical erectile body, measuring about 1.5–2 cm situated in the most anterior part of the vulva. It consists of a glans, a body and two crura. The clitoris consists of two cylindrical corpora cavernosa (erectile tissue).
VESTIBULE: It is a triangular space bounded anteriorly by the clitoris, posteriorly by the fourchette and on either side by labia minora. There are four openings into the vestibule.
(a) Urethral opening:
(b) Vaginal orifice and hymen: The vaginal orifice lies in the posterior end of the vestibule and is of varying size and shape. It is incompletely closed by a septum of mucous membrane, called hymen. The hymen is usually ruptured at the consummation of marriage.
(c) (c) Opening of Bartholin’s ducts: There are two Bartholin glands (greater vestibular gland), one on each side. They are pea-sized. During sexual excitement, it secretes abundant mucus which helps in lubrication. Each gland has got a duct which measures about 2 cm and opens into the vestibule outside the hymen at the junction of the anterior two-third and posterior one-third in the groove between the hymen and the labium minus.
(d) (d) Skene’s glands are the largest paraurethral glands. The two Skene’s ducts may open in the vestibule on either side of the external urethral meatus.
VESTIBULAR BULB: These are bilateral elongated masses of erectile tissues situated beneath the mucous membrane of the vestibule. Each bulb lies on either side of the vaginal orifice in front of the Bartholin’s gland
BLOOD SUPPLY: Arteries—(a) Branches of internal pudendal artery—
. (b) Branches of femoral artery—(C) superficial and deep external pudendal.
Veins—The veins form plexuses and drain into: (a) Internal pudendal vein (b) Vesical or vaginal venous
plexus and (c) Long saphenous vein.
NERVE SUPPLY:
ilio-inguinal and genital branch of genito-femoral nerve (L1and L2) and the posterior-inferior part by the pudendal branches from the posterior cutaneous nerve of thigh (S1.2.3). Between these two groups, the vulva is supplied by the labial and perineal branches of the pudendal nerve (S2.3.4).
LYMPHATICS: Vulval lymphatics have bilateral drainage. Lymphatics drain into—(a) Superficial inguinal
nodes, (b) Intermediate groups of inguinal lymph nodes—gland of Cloquet and (c) External and internal
iliac lymph nodes.
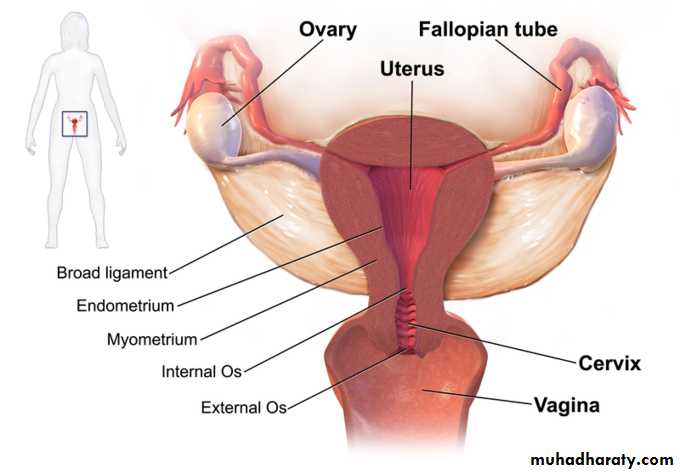
INTERNAL GENITAL ORGANS
The internal genital organs in female include vagina, uterus, Fallopian tubes and the ovariesVAGINA
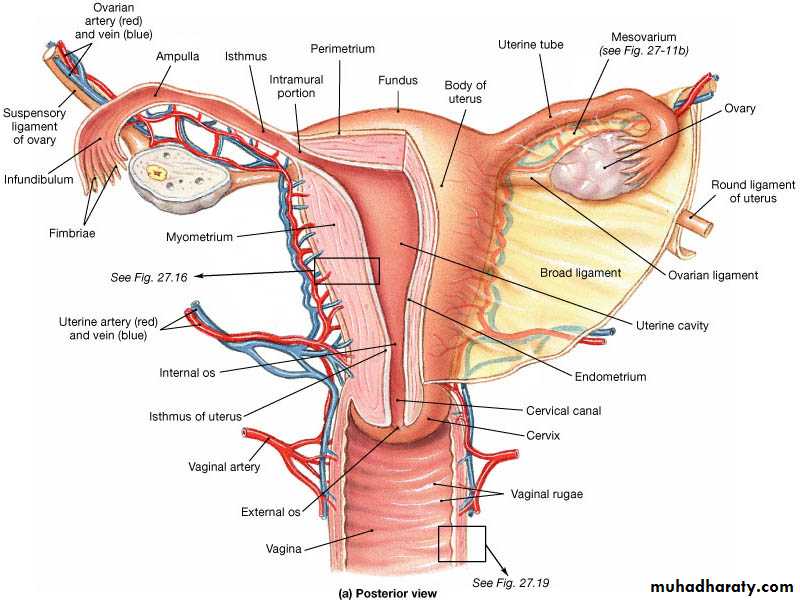
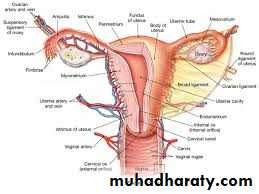
The vagina is a fibromusculomembranous sheath communicating the uterine cavity with the exterior at the vulva.
It constitutes the excretory channel for the uterine secretion and menstrual blood. It is the organ of copulation and forms the birth canal of parturition. The canal is directed upwards and backwards
WALLS: Vagina has got an anterior, a posterior and two lateral walls. The anterior and posterior walls are
apposed together but the lateral walls are comparatively stiffer specially at its middle, as such, it looks ‘H’ shaped on transverse section. The length of the anterior wall is about 7 cm and that of the posterior wall is about 9 cm.
FORNICES: The fornices are the clefts formed at the top of vagina (vault) due to the projection of the uterine cervix. There are four fornices—one anterior, one posterior and two lateral; .
RELATIONS:
Anterior—The upper one-third is related with base of the bladder and the lower two-thirds are with theurethra, .
Posterior—The upper one-third is related with the pouch of Douglas, the middle-third with the anterior
rectal wall and the lower-third is separated from the anal canal by the perineal body .
Lateral walls—The upper one-third is related with the pelvic cellular tissue at the base of broad ligament
in which the ureter and the uterine artery lie approximately 2 cm from the lateral fornices. The middle third is blended with the levator ani and the lower-third is related with the bulbocavernosus muscles, vestibularbulbs and Bartholin’s glands .
VAGINAL SECRETION: The vaginal pH, from puberty to menopause, is acidic because of the presence of
Doderlein’s bacilli which produce lactic acid from the glycogen present in the exfoliated cells. The pH varies with the estrogenic activity and ranges between 4–5.
BLOOD SUPPLY: The arteries involved are—(1) Cervicovaginal branch of the uterine artery (2) Vaginal
artery—a branch of anterior division of internal iliac or in common origin with the uterine (3) Middle
rectal and (4) Internal pudendal. These anastomose with one another and form two azygos arteries—
anterior and posterior.
Veins drain into internal iliac veins and internal pudendal veins.
LYMPHATICS: On each side, the lymphatics drain into—(1) Upper one-third—internal iliac group, (2) Middle one-third up to hymen—internal iliac group (3) Below the hymen—superficial inguinal group.
NERVE SUPPLY: The vagina is supplied by sympathetic and parasympathetic from the pelvic plexus. The
lower part is supplied by the pudendal nerve.
(2)Isthmus is a constricted part measuring about 0.5 cm, situated between the body and the cervix. It is limited above by the anatomical internal os and below by the histological internal os (Aschoff). Some consider isthmus as a part of the lower portion of the body of the uterus.
(3) Cervix is cylindrical in shape and measures about 2.5 cm. It extends from the isthmus
and ends at the external os which opens into the vagina after perforating its anterior wall. The part lying above the vagina is called supravaginal and that which lies within the vagina is called the vaginal part.
CAVITY: The cavity of the uterine body is triangular on coronal section with the base above and the apex below. It measures about 3.5 cm. There is no cavity in the fundus. The cervical canal is fusiform and measures about 2.5 cm. Thus, the normal length of the uterine cavity is usually 6.5–7 cm.
RELATIONS Anteriorly—Above the internal os, the body forms the posterior wall of the uterovesical pouch. Below the internal os, it is separated from the base of the bladder by loose areolar tissue. Posteriorly—It is covered with peritoneum and forms the anterior wall of the pouch of Douglas containing coils of intestine. Laterally—The double fold of peritoneum of the broad ligament are attached between which the uterine artery ascends up. Attachment of the Mackenrodt’s ligament extends from the internal os down to the supravaginal cervix and lateral vaginal wall. About 1.5 cm away at the level of internal os, a little nearer on the left side is the crossing of the uterine artery and the ureter..
STRUCTURES Body — The wall consists of 3 layers from outside inwards: — Parametrium: It is the serous coat which invests the entire organ except on the lateral borders.
— Myometrium: It consists of thick bundles of smooth muscle fibers held by connective tissues and are arranged in various directions. During pregnancy, however, three distinct layers can be identified—outer longitudinal, middle interlacing and the inner circular.
— Endometrium: The mucous lining of the cavity is called endometrium.
As there is no submucous layer, the endometrium is directly apposed to the muscle coat.
. Cervix—The cervix is composed mainly of fibrous connective tissues.. Mucous coat lining the gland is non-ciliated secretory columnar cells. The vaginal part of the cervix is lined by stratified squamous epithelium. The squamo-columnar junction is situated at the external os.
BLOOD SUPPLY: Arterial supply — The blood supply is from the uterine artery one on each side. The other sources are ovarian and vaginal arteries
Veins: The venous channels correspond to the arterial course and drain into internal iliac veins. LYMPHATICS: Body—pre-aortic and lateral aortic groups of glands ,superficial inguinal gland and external iliac groups
Cervix—external iliac, obturator lymph nodes either directly or through para-cervical lymph nodes, (2) internal iliac groups and (3) sacral groups.
NERVES: Sympathetic components are from T5 and T6 (motor) and T10 to L1 spinal segments (sensory). The somatic distribution of uterine pain is that area of the abdomen supplied by T10 to L8 . The parasympathetic system is represented on either side by the pelvic nerve which consists of both motor and sensory fibers from S2 , S3 , S4.
FALLOPIAN TUBE
Synonyms: Uterine tube, oviduct The uterine tubes are paired structures, measuring about 10 cm.PARTS: There are four parts. From medial to lateral are—(1) intramural or interstitial lying in the uterine wall and measures 1.25 cm in length and 1 mm in diameter, (2) isthmus—almost straight and measures about 3–4 cm in length and 2 mm in diameter, (3) ampulla—tortuous part and measures about 5 cm in length which ends in, (4) wide infundibulum measuring about 1.25 cm long with a maximum diameter of 6 mm.
STRUCTURES: It consists of 3 layers—(1) Serous: consists of peritoneum on all sides except along the line of attachment of mesosalpinx, (2) Muscular: arranged in two layers outer longitudinal and inner circular, (3) Mucous membrane has three different cell types and is thrown into longitudinal folds. Mucous membrane is lined by: (i) Columnar ciliated epithelial , (ii) Secretory columnar cells (iii) Peg cells are found in between the above two cells. They are the variant of secretory cells.
FUNCTIONS: The important functions of the tubes are—(1) Transport of the gametes, (2) To facilitate fertilization and survival of zygote through its secretion.
BLOOD SUPPLY: Arterial supply is from the uterine and ovarian. Venous drainage is through the pampiniform plexus into the ovarian veins.
LYMPHATICS: The lymphatics run along the ovarian vessels to para-aortic nodes.
NERVE SUPPLY: The nerve supply is derived from the uterine and ovarian nerves.
THE OVARY
The ovaries are paired sex glands or gonads in female which are concerned for (i) germ cell maturation, storage and its release and (ii) steroidogenesis. Each gland is oval in shape and pinkish gray in color and the surface is scarred during reproductive period. It measures about 3 cm in length, 2 cm in breadth and 1 cm in thickness. Each ovary presents two ends-tubal and uterine, two borders-mesovarium and free posterior and two surfaces —medial and lateral. The ovaries are intraperitoneal structures. the ovary lies in the ovarian fossa on the lateral pelvic wall. The ovary is attached to the posterior layer of the broad ligament by the mesovarium, to the lateral pelvic wall by the infundibulopelvic ligament and to the uterus by the ovarian ligament.RELATIONS: Mesovarium or anterior border—A fold of peritoneum from the posterior leaf of the broad ligament is attached to the anterior border through which the ovarian vessels and nerves enter the hilum of the gland.
Posterior border is free and is related to the tubal ampulla. It is separated by the peritoneum from the ureter and the internal iliac artery.
Medial surface is related to fimbrial part of the tube.
Lateral surface is in contact with the ovarian fossa on the lateral pelvic wall. The fossa is related superiorly to the external iliac vein, posteriorly to the ureter and internal iliac vessels and laterally to the peritoneum separating the obturator vessels and nerves .
STRUCTURES: The ovary is covered by a single layer of cubical cell known as germinal epithelium. The substance of the gland consists of outer cortex and inner medulla.
Cortex—It consists of stromal cells which are thickened beneath the germinal epithelium to form tunica albuginea. During reproductive period (i.e. from puberty to menopause) the cortex is studded with numerous follicular structures. These are related to sex hormone production and ovulation.
Medulla—It consists of loose connective tissues, few unstriped muscles, blood vessels and nerves. There is a small collection of cells called “hilus cells”.
BLOOD SUPPLY: Arterial supply is from the ovarian artery, a branch of the abdominal aorta. Venous drainage is through pampiniform plexus, to form the ovarian veins which drain into inferior vena cava on the right side and left renal vein on the left side.
LYMPHATICS: Through the ovarian vessels drain to the para-aortic lymph nodes.
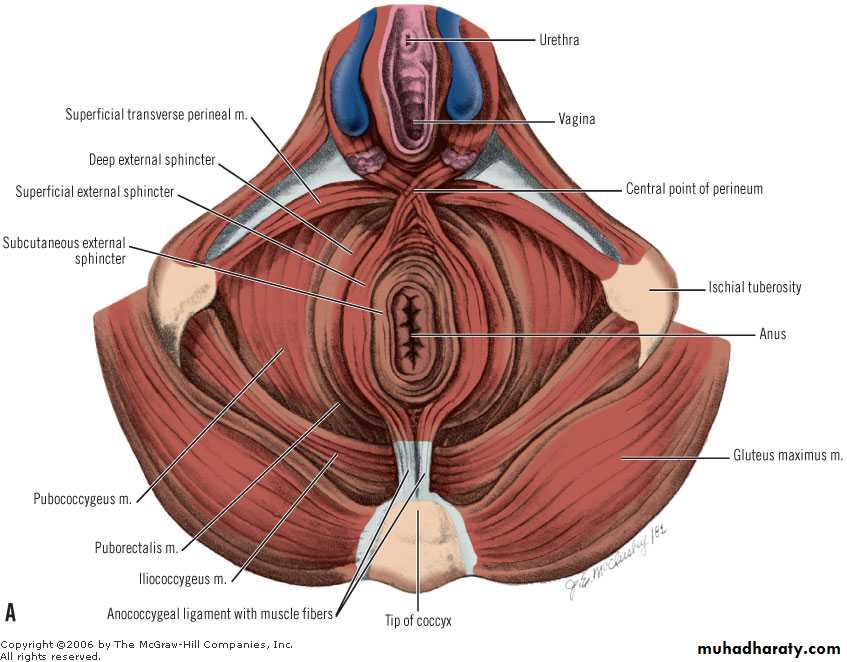
. MUSCLES IN RELATION TO THE PELVIC ORGANS The most important muscle supporting the +
pelvic organs is the levator ani which forms the pelvic floor. The small muscles of the perineum also have got some contribution.PELVIC FLOOR (Synomym: Pelvic diaphragm) Pelvic floor is a muscular partition which separates the pelvic cavity from the anatomical perineum. It consists of three sets of muscles on either side—pubococcygeus, iliococcygeus and ischiococcygeus and these are collectively called levator ani. Its upper surface is concave and slopes downwards, backwards and medially and is covered by parietal layer of pelvic fascia. The inferior surface is convex and is covered by anal fascia. The muscle with the covering fascia is called the pelvic diaphragm
STRUCTURES IN RELATION TO PELVIC FLOOR The superior surface is related with the following:
(1) Pelvic organs from anterior to posterior are bladder, vagina, uterus and rectum.(2) Pelvic cellular tissues between the pelvic peritoneum and upper surface of the levator ani which fill all the available spaces.
(3) Ureter lies on the floor in relation to the lateral vaginal fornix. The uterine artery lies above and the vaginal artery lies below it.
(4) Pelvic nerves. The inferior surface is related to the anatomical perineum.
NERVE SUPPLY: It is supplied by the 4th sacral nerve, inferior rectal nerve and a perineal branch of pudendal nerve S2,3,4.
FUNCTIONS:
(1) To support the pelvic organs—
(2) To maintain intra-abdominal pressure by reflexly responding to its changes.
(3) Facilitates anterior internal rotation of the presenting part when it presses on the pelvic floor.
(4) Puborectalis plays an ancillary role to the action of the external anal sphincter.
(5) Ischiococcygeus helps to stabilize the sacroiliac and sacrococcygeal joints.
(6) To steady the perineal body.
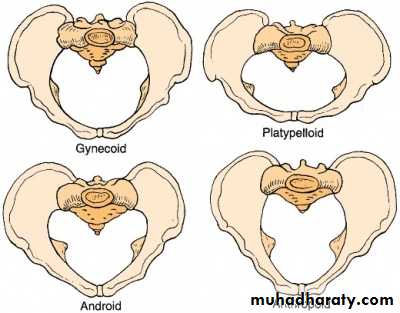
MUSCULOSKELETAL PELVIC ANATOMY ●
Pelvic Bones The pelvis is composed of four bones— the sacrum, coccyx, and two innominate bones. Each innominate bone is formed by the fusion of three bones—the ilium, ischium, and pubis . Both innominate bones are joined to the sacrum at the sacroiliac synchondroses and to one another at the symphysis pubis.Planes and Diameters of the Pelvis
The pelvis is described as having four imaginary planes:The plane of the pelvic inlet—the superior strait
. 2. The plane of the pelvic outlet—the inferior strait.
3. The plane of the midpelvis—the least pelvic dimensions.
4. The plane of greatest pelvic dimension—of no obstetrical significance.
• Pelvic Inlet, the pelvic inlet is also the superior plane of the true pelvis. it is bounded posteriorly by the promontory and alae of the sacrum, laterally by the linea terminalis, and anteriorly by the dfhhorizontal pubic rami and the symphysis pubis. During labor, fetal head engagement is defined by the fetal head’s biparietal diameter passing through this plane. Four diameters of the pelvic inlet are usually described: anteroposterior, transverse, and two oblique diameters. Of these, distinct anteroposterior diameters have been described using specific landmarks .
Midpelvis and Pelvic Outlet The midpelvis is measured at the level of the ischial spines, also called the midplane or plane of least pelvic dimensions. During labor, the degree of fetal head descent into the true pelvis may be described by station, and the midpelvis and ischial spines serve to mark zero station. The interspinous diameter is 10 cm or slightly greater, is usually the smallest pelvic diameter, and, in cases of obstructed labor, is particularly important. The anteroposterior diameter through the level of the ischial spines normally measures at least 11.5 cm. The pelvic outlet consists of two approximately triangular areas whose boundaries mirror those of the perineal triangle.
Pelvic Shapes
anatomical classification of the pelvis is based on shape, and its concepts aid an understanding of labor mechanisms. Specifically, the greatest transverse diameter of the inlet and its division into anterior and posterior segments are used to classify the pelvis as gynecoid, anthropoid, android, or platypelloid.1 .Gynaecoid Pelvis.
This is the most suitable female pelvic shape. This allow normal child birth with ease. It has round pelvic inlet and shallow pelvic cavity with short ischial spines. All these feature allow rapid birth of the baby. So Gynaecoid Pelvis is the most suitable pelvic shape for childbirth.2. Anthropoid Pelvis.
Anthropoid pelvis has oval shaped inlet with large anterio-posterior diameter and comparatively smaller transverse diameter. It has larger outlet. The problem in this pelvis is the inlet. The diameters of inlet favors the engagement of fetal head in occiput-posterior position that may slow down the progress of labor. If head engages in anterior position then labor progress normally in most of the cases.3. Android Pelvis.
Android shaped pelvis has triangular or heart-shaped inlet and is narrower from the front. It has prominent ishial spines and also has narrower transverse outlet diameter. Such pelvis is more likely to be present in tall women. African-Caribbean women are more at risk of having an adroid shaped pelvis. Child birth is difficult and more complicated in android shaped pelvis than gynaecoid pelvis. Women have to push harder, walk more often and chances of instrumental vaginal delivery are high. It may prolong the labor.4. Platypelloid Pelvis.
Platypelloid pelvis is has narrow anterio-posterior diameter of pelvic inlet. The pelvic inlet is specifically kidney shaped. The pelvic cavity is usually shallow and diameters of outlet are favorable for the process of labor. But platypelloid pelvis don’t allow the head to engage with ease. But if the head manage to engage then rest of the process of labor may occur normally but in most of the cases it is longer as compared to progress of labor in case of gynaecoid pelvis.Physiology of female reproductive organs
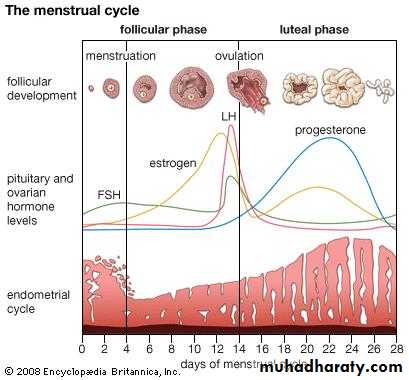
Menstrual cycle in the female reflects the physiological change of her reproductive organs.The most obvious manifestation of the normal menstrual cycle is the presence of regular menstrual periods.Menstruation is initiated in response to changes in steroids produced by the ovaries, which themselves are controlled by the pituitary and hypothalamus.Oogenesis: The formation and maturation of an oocyte.It starts with the growth of a primordial follicle to form a pre-antral follicle and ends with the final maturation of a pre-ovulation follicle.The formation of the preantral follicle takes 85 days in a human. The final maturation stage from the pre-antral follicle to the pre-ovulatory follicle takes 14 days to complete.
The physiological changes of the ovaries:
Within the ovary, the menstrual cycle can be dividedinto three phases:the follicular phase 2. ovulation 3. the luteal phase
1-Follicular phase: The development of the oocyte is the key event.The ovary contains thousands of primordial follicles that are in a continuous state of development from birth, through periods of anovulation, such as pregnancy, to the menopause. These initial stages of follicular development are independent of hormonal stimulation. In the absence of the correct hormonal stimulus, however, follicular development fails at the pre-antral stage, with ensuing follicular atresia.Development beyond the pre-antral stage is stimulated by the pituitary hormones (luteinizing hormone [LH] and follicle stimulating hormone [FSH]),
which can be considered as key regulators of oocyte development.At the start of the menstrual cycle, FSH levels begin to rise as the pituitary is released from the negative feedback effects of progesterone, oestrogen and inhibin.Rising FSH levels rescue a cohort of follicles from atresia, and initiate steroidogenesis Steroidogenesis The basis of hormonal activity in pre-antral to pre-ovulatory follicles is described as the 'two cell,two gonadotrophin' hypothesis. Steroidogenesis is compartmentalized in the two cell types within the follicle: the
theca and granulosa cells; these cells are responsive to the gonadotrophins LH and FSH respectively.Within the theca cells, LH stimulates the production of androgens from cholesterol. Within the granulosa cells, FSH stimulates the conversion of thecally derived androgens to oestrogens (aromatization) .FSH is also responsible for the proliferation of granulosa cells. Selection of the dominant follicle: Is the result of complex signalling between the ovary and the pituitary.The dominant follicle is the largest and most developed follicle in the ovary at the mid-follicular phase.
Such a follicle has the most efficient aromatase activity and the highest concentration of FSH induced LH receptors.Therefore produces the greatest amount of oestradiol and inhibin. Inhibin further amplifies LH-induced androgen synthesis, which is used as a substrate for oestradiolsynthesis.These features mean that the largest follicle therefore requires the lowest levels of FSH (and LH) for continued development.
Inhibin: was originally described as a testicular product that inhibited pituitary FSH production hence its name.However, inhibin is also produced by a variety of other cell types, including granulosa cells within the ovary; production is stimulated by FSH . In women, as in men, inhibin attenuates FSH production..
Activin :is a peptide that that is structurally related to inhibin.It is produced both by the granulosa cells of antral follicles and by the pituitary gland.The action is almost directly opposite to that of inhibin in that it augments pituitary FSH secretion and increases FSH binding to granulosa cells.
2-Ovulation: Late in the follicular phase, FSH induces LH receptors on granulosa cells.Oestrogen is an obligatory co-factor in this effect. As the dominant follicle develops further, follicular oestrogen production increases. Thus the production of oestrogen is sufficient for it to reach the threshold required to exert a positive-feedback effect on pituitary LH secretion. LH levels increase, at first quite slowly (day 8 to day 12 of the menstrual cycle) and then more rapidly (day 12 onwards).
• During this time, LH induces luteinization of granulosa cells in the dominant follicle, so that progesterone is produced. Progesterone further amplifies the positive-feedback effect of oestrogen on pituitary LH secretion, leading to a surge of LH.Ovulation occurs 36 hours after the onset of the LH surge.
3-Luteal phase: Is characterized by the production of progesterone from the corpus luteum within the ovary.The corpus luteum is derived both from the granulosa cells that remain after ovulation and from some of the theca cells that differentiate to become theca lutein cells.The granulosa cells of the corpus luteum have a vacuolated appearance associated with the accumulation of a yellow pigment, lutein, from where the corpus luteum derives its name.
• The production of progesterone from the corpus luteum is dependent on continued pituitary LH secretion.However, serum levels of progesterone are such that LH and FSH production is relatively suppressed. The low levels of gonadotrophins mean that the initiation of new follicular growth is inhibited for the duration of the luteal phase.The duration of the luteal phase is fairly constant, being around 14 days in most women.At the end of the luteal phase, in the absence of pregnancy, the corpus luteum regresses (luteolysis) that is controled by an obscure mechanism.
•
Hypothalamo-pituitary-ovanan axis showing positive and negative feedback of hormones The hypothalamo-pituitary-ovarian axis: The ovary, pitutary&the hypothlamus act in concerntto ensure the growth and development of (ideally) one ovarian follicle, and to maintain hormonal support of the endometrium to allow implantation.The output of LH and FSH from the pituitary gland is stimulated by pulses of gonadotrophin-releasing hormone (GnRH) produced by the hypothalamus and transported to the pituitary in the portal circulation
Production of GnRH has an effect alterations in the amplitude and frequency of GnRH pulsation throughout the cycle that are responsible for some fine tuning of gonadotrophin production. The response of the pituitary is not constant, but is modulated by ovarian hormones, particularly oestrogen and progesterone.Low levels of oestrogen have an inhibitor effect on LH (negative feedback), whereas high levels of oestrogen actually stimulate pituitary LH production (positive feedback).In the late follicular phase, serum levels of oestrogen are sufficiently high that a positive-feedback effect is triggered, thus generating the peri-ovulatory LH surge.
• The mechanism of action of the positive-feedback effect of oestrogen involves an increase in GnRH receptor concentrations and an increase in GnRH production.The mechanism of the negative-feedback effect of oestrogen is uncertain.Low levels of progesterone prior to ovulation have a positive-feedback effect on pitutary LH and FSH secretion and contribute to the LH surge. High levels of progesterone (luteal phase) inhibit pituitary gonadotrophin production.Negativefeedback effects of progesterone are generated both via decreased GnRH production and via decreased sensitivity to GnRH at the pituitary level.
• The physiological changes in the endometrium:
1-Menstruation: As the corpus luteum dies at the end of the luteal phase, circulating levels of oestrogen and progesterone fall precipitously.In an ovulatory cycle, where the endumetrium is exposed to oestrogen and then progesterone in an orderly manner, the endometrium becomes 'decidualized' during the second half of the cycle to allow implantation of the embryo.• Decidualizalion is an irreversible process, and if implantation does not occur, programmed cell death (apoptosis) ensues.Menstruation is the shedding of the 'dead' endometrium and ceases as the endometrium regenerates.
• 2-Proliferative/follicular phase: Once endometrial repair is completed, usually at around day 5-6 of the cycle, menstruation ceases.Within the endometrium, the remainder of the follicular phase is characterized by glandular and stromal growth - hence the name the proliferative phase.The epithelium lining the endometrial glands changes from a single layer of low columnar cells to pseudostratiffed epithelium withfrequent mitoses.The endometrial thickness increase from 0.5mm at menstruation to 3.5-5 mm at the end of the proliferative phase.
The secretory/luteal phase: Is characterized by endometrial glandular secretory activity - hence the name the secretory phase. Under the action of progesterone,. Some elements continue to grow, leading to increased tortuosity of both the glands and spiral arteries in order to fit into the endometrial layer
• Peak secretory activity' occurs at the time of implantation, 7 days after the gonadotrophin surge.Progesterone is essential for the induction of endometrial secretory changes and these changes are only seen after ovulation in the absence of exogenous steroid therapy.In the late secretory phase, progesterone inducts irreversible decidualization of the stroma. Histologically, decidualization is initiated around blood vessels.The surrounding stromal cells display increased mitotic activity and nuclear enlargement and a basement membrane is generated.Immediately prior to menstruation, three distinct zones of the endometriurn can be seen: 1-The basalis 2-Stratum spongiosum 3-Stratum compactum The basalis is the basal, which is retained during menstruation and shows few changes during the menstrual cycle.
• The normal menstrual cycle is 28 days long (from the start of one cycle to the start of"the next) ..Any cycle of between 21 and 35 days long can be regarded as normal.The length of the menstrual cycle is determined by the length of the follicular phase. Once ovulation occurs, luteal phase length is fairly fixed at 14 days in almost all women.The duration of menstrual flow also varies among women from 2 to 8 day; peaks on the first or second day of menstrnation. The normal volume of menstrual loss is 35 mL per month.