
Bacterial Skin Infections

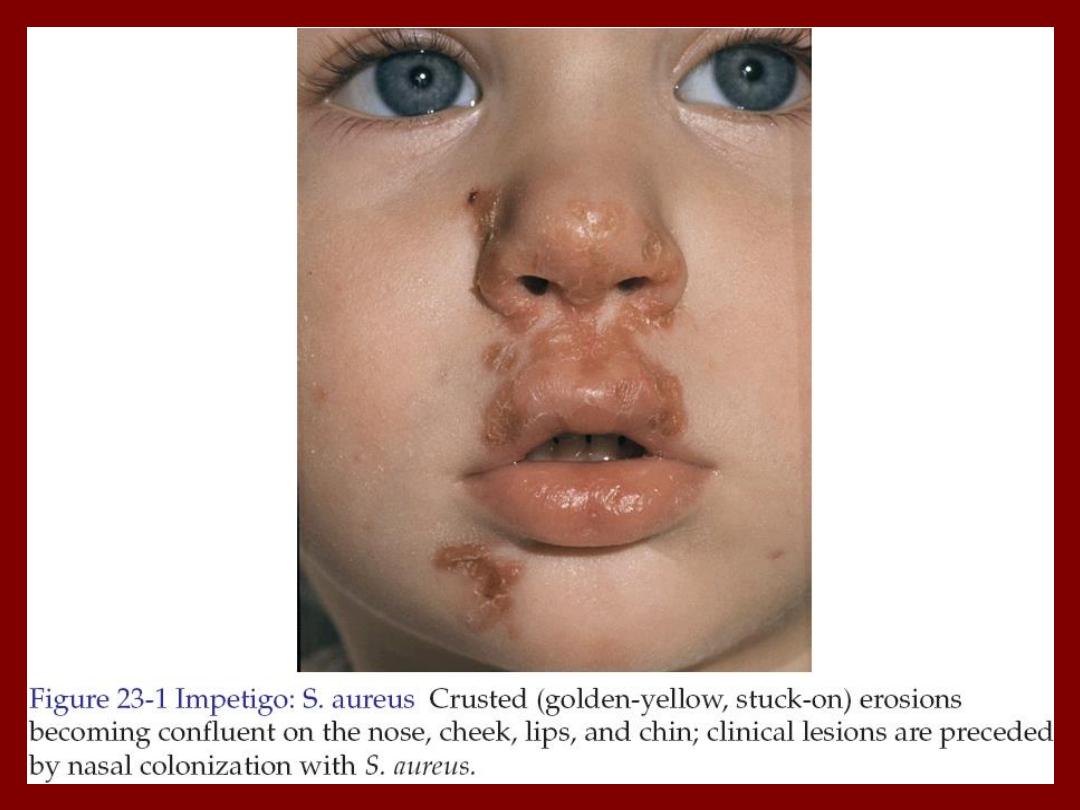
Impetigo Contagiosa
• It is a common superficial skin infection.
• There are two forms:
– Bullous impetigo.
– Non-bullous impetigo.
• Both begin as vesicles with a very thin fragile
roof consisting of only stratum corneum.
• The lesions are asymptomatic.
• Bullous impetigo is caused by staphylococcus
aureus.

• Non-bullous impetigo in majority caused by S. aureus
but occasionally caused by group A beta hemolytic
streptococci or both.
• In both the disease is common in children.
• In bullous form, one or more vesicles enlarge rapidly
to form bullae then the center of the thin roofed bulla
collapses to form a thin flat honey yellow colored crust
appear in the center. The face is common site of
involvement.
• In non-bullous impetigo the small vesicle or pustule
ruptures to expose a red moist base (erosion). A
honey-yellow to brown firmly adherent crust
accumulates as the lesions extend radially. The skin
around nose, mouth and the limbs are commonly
involved.

Impetigo (Pustules)

Impetigo Contagiosa

The complications of impetigo
• Post-streptococcal glomerulonephritis usually
develop 1-3 weeks following acute infection
with specific nephritogenic strains of group A
beta hemolytic streptococci.
• Lymphadenitis is common with streptococcal
infections.
• Urticaria.
• Erythema multiforme.

Treatment
• If the area is solitary and small use topical
antibiotics like fusidic acid.
• If the infection is widespread, severe or
accompanied by lymphadenopathy then oral
antibiotics are indicated like flucloxacillin.
• Removal of infected crusts by washing with
soap and water is bacteriologically and
cosmetically helpful.
• Lesions heal without scarring.

Ecthyma(ta)
• Ecthyma is a deep bacterial infection that involves the
dermis. It is caused by streptococci, staphylococci or
both.
• It characterized by punched out ulcer that is covered
by adherent crust surrounded by erythema.
• Buttocks, thighs and legs are common sites.
• Poor hygiene, immunosuppression, and malnutrition
are a predisposing factors.
• Treatment is by systemic antibiotics.
• Healing occurs in few weeks with scarring.

Ecthyma


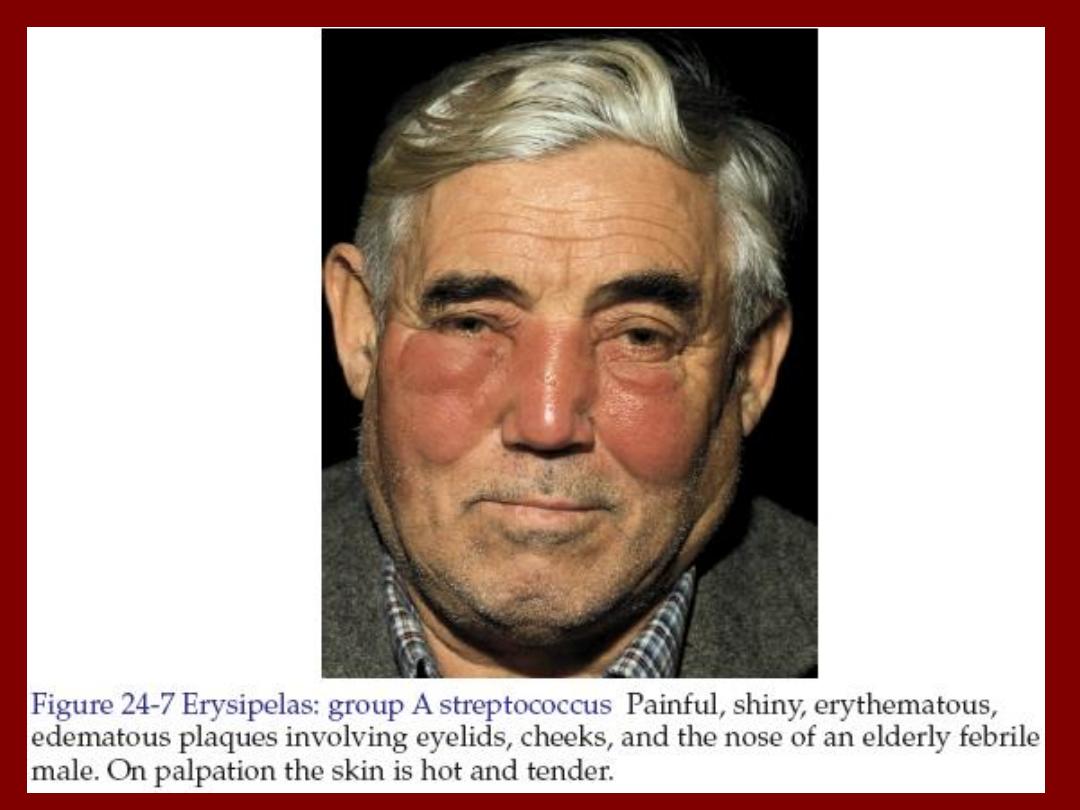
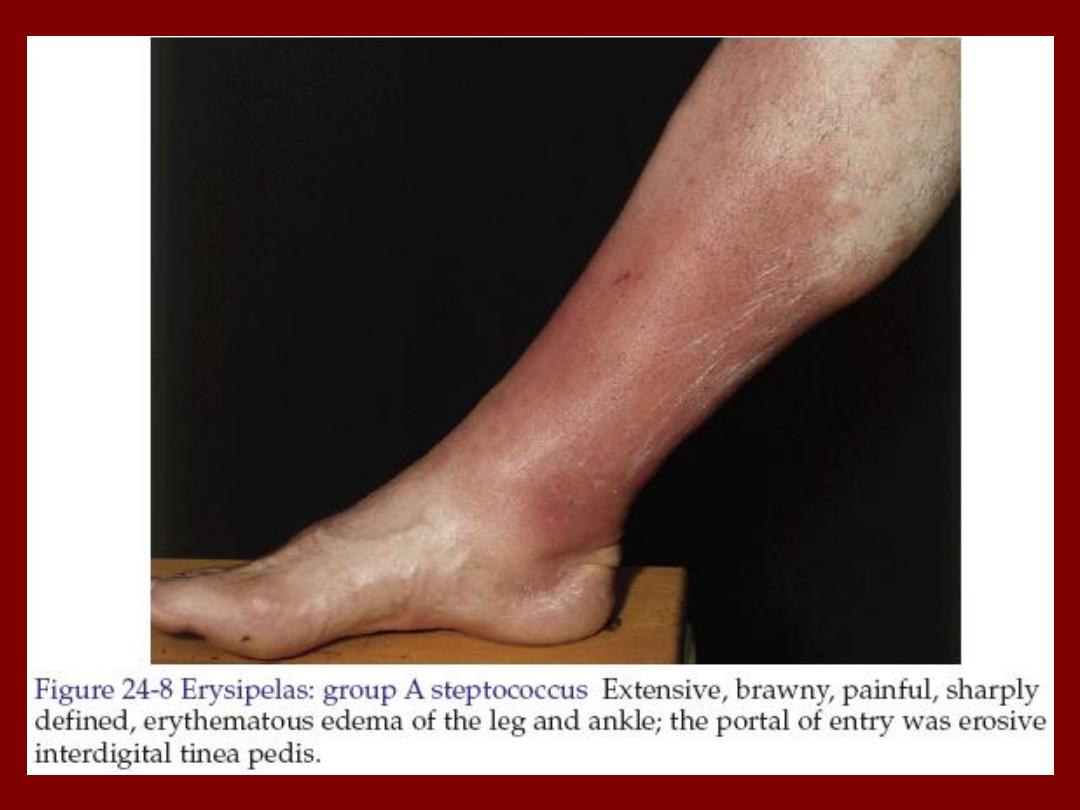
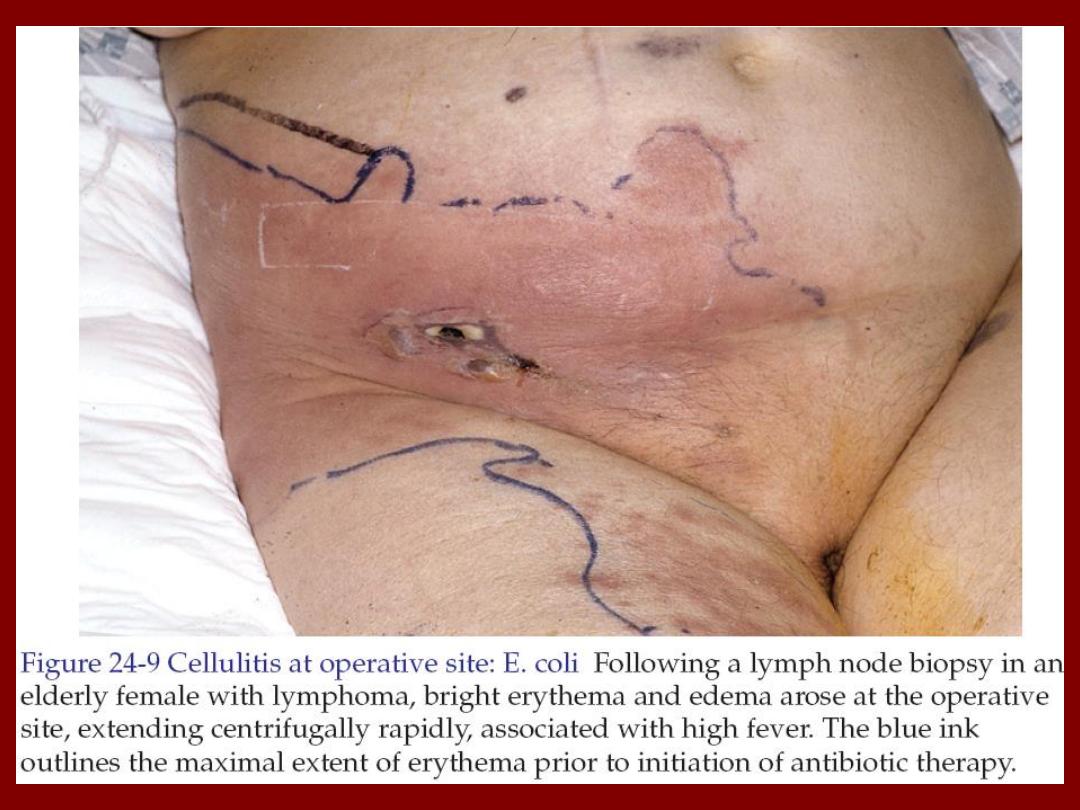
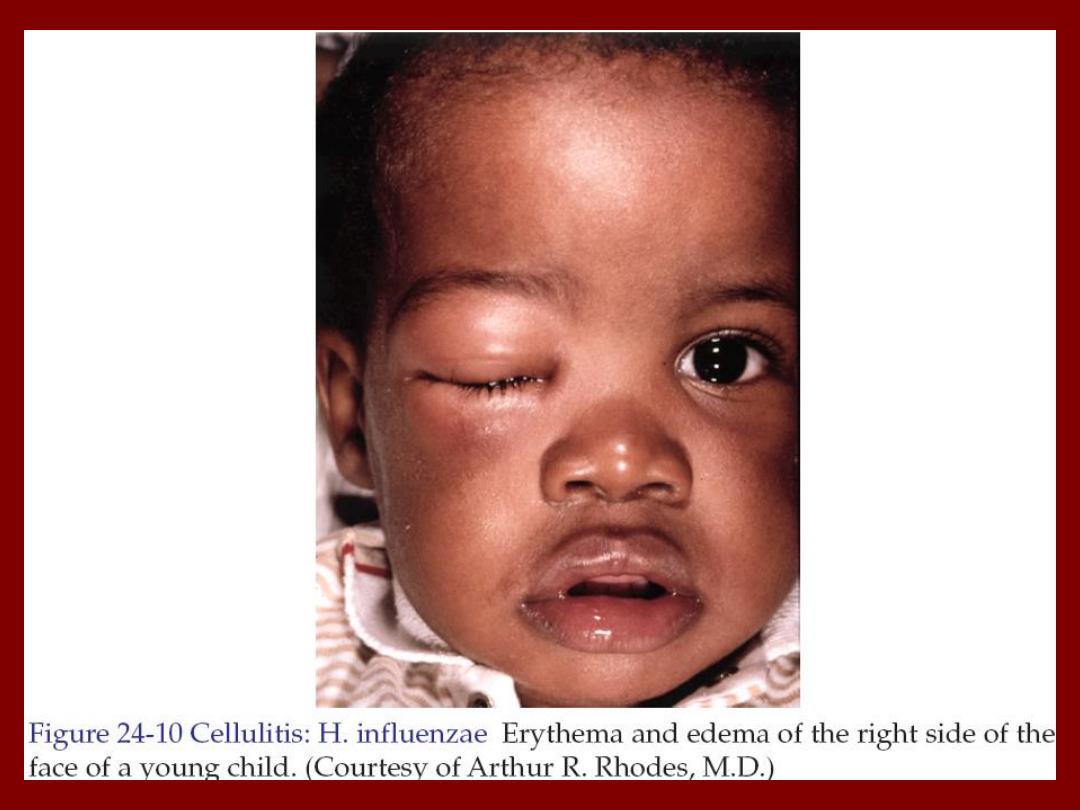
Cellulitis and Erysipelas
• Both are skin infections characterized by
erythema, edema and pain.
• In most instances there is fever.
• Both may be accompanied by lymphangitis and
lymphadenitis.
• Pathogens enter at the site of local trauma or
abrasions and psoriatic, eczematous or tinea
lesions.
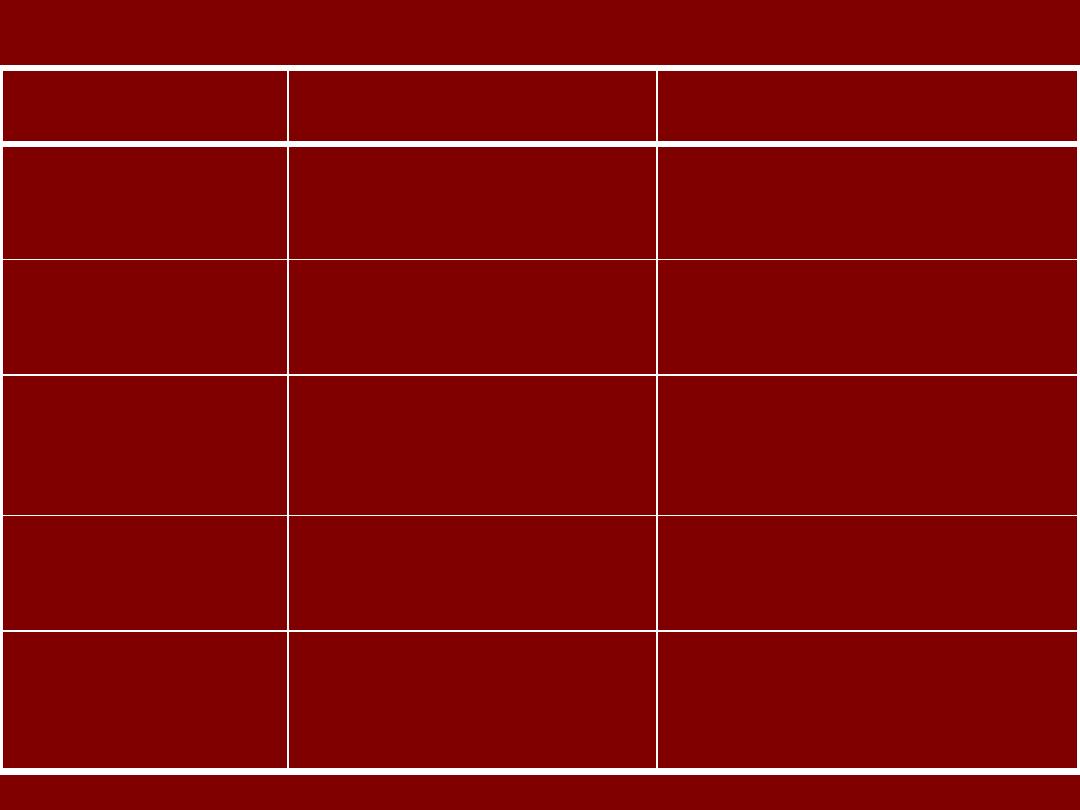
Cellulitis
Erysipelas
Feature
Dermis and
subcutaneous tissues
Dermis
Pathology site
Streptococci, S. aureus,
H. influenzae and others
Usually streptococci
Cause
Indistinct
Distinct
Margin between
involved and
uninvolved skin
Any site
Lower legs, face and
ear
Common sites
Not prominent
Prominent
Lymphatic
involvement
(streaking)
Table shows the differences between erysipelas and cellulitis

Treatment
• Flucloxacillin (penicillinase resistant penicillin)
500 mg every 6 hours orally for 10 days.
Or
• Cephalexin 500 mg every 6 hours orally for 10
days.
Or
• Gentamycin 80 mg 2-3 times daily for 7 days if
gram-negative infection is suspected.

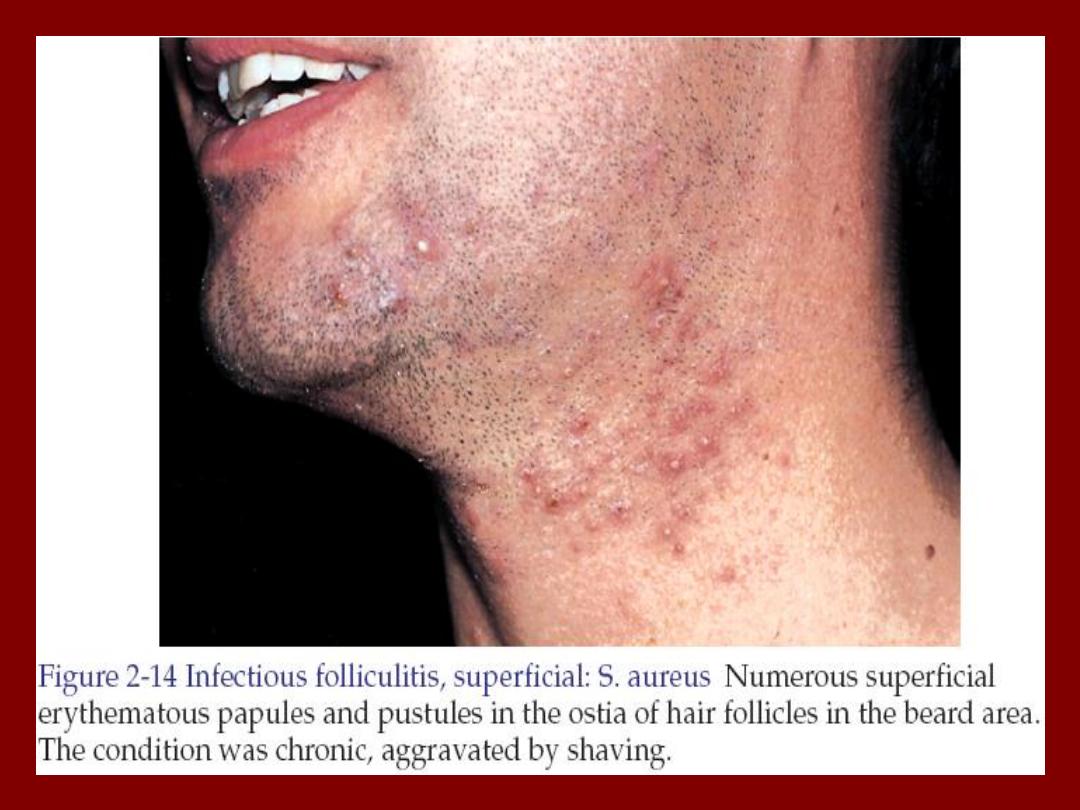
Folliculitis
• Folliculitis is inflammation of the hair follicle
caused by infection, chemical irritation or
physical injury.
• In superficial folliculitis, the inflammation is
confined to the upper part of the hair follicle. It
manifested as a painless or tender pustule that
eventually heals without scarring.
• In deep folliculitis, the inflammation involves the
deeper portion of the hair follicle or the entire
follicle. The lesions are painful and may heal
with scarring.
Deep folliculitis
Superficial folliculitis
Furuncle and Carbuncle
Staphylococcal folliculitis
Sycosis barbae
Pseudofolliculitis barbae
(from shaving)
Diseases initially manifesting as folliculitis

Staphylococcal folliculitis
• It occur because of injury, abrasion, nearby
surgical wounds or draining abscesses.
• It may also be a complication of occlusive
topical steroid therapy.
• Oral antistaphylococcal antibiotics like
flucloxacillin is used in the treatment.

Staphylococcal folliculitis (Bockhart's Impetigo)

Pseudofolliculitis barbae
• It is a foreign body reaction to hair. The
condition occurs on the cheeks and neck in
individuals who are genetically inclined to have
tightly curled spiral hair, which become ingrown.
• Secondary bacterial infection may supervene.
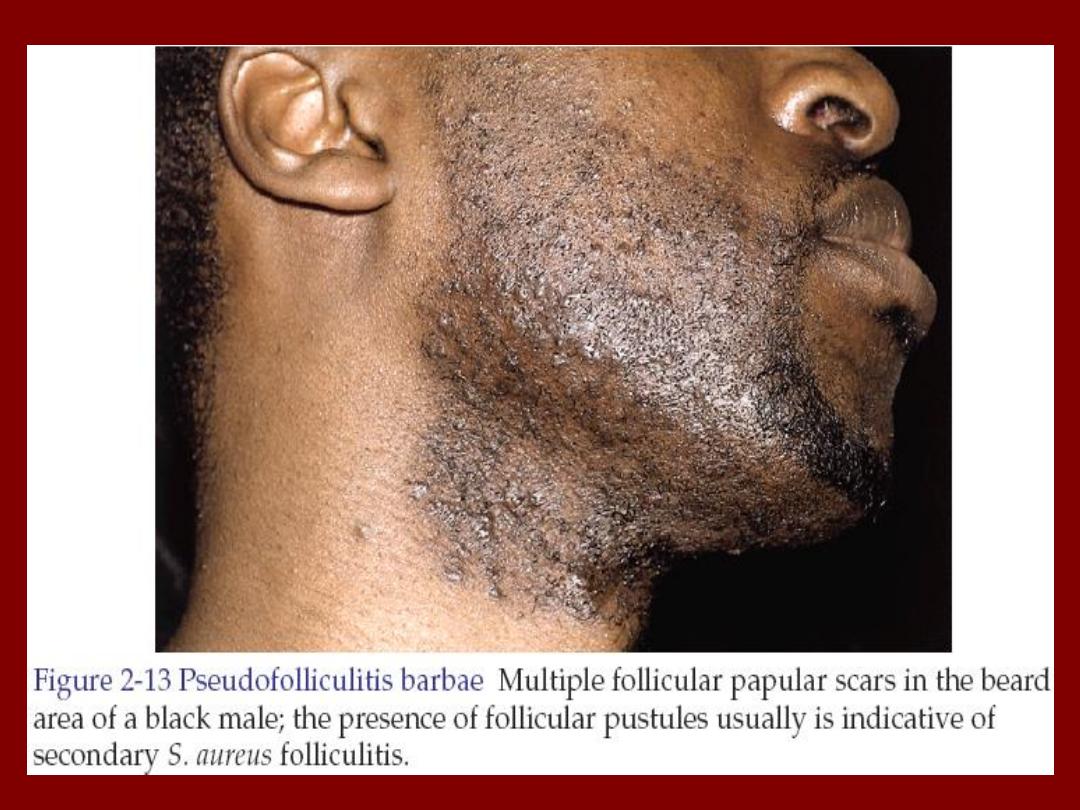

Pseudofolliculitis barbae

Treatment
• Stop shaving.
• Dislodge embedded hair shafts by inserting a
firm pointed instrument such as syringe needle
under the hair loop and firmly elevating it.
• A short course of antibiotics may hasten
resolution.
• Corticosteroid (prednisone at 40-60 mg/day for
5-10 days) may be used in moderate to severe
cases to reduce inflammation around the hair
follicles until the hair grows and is no longer an
aggravating factor.

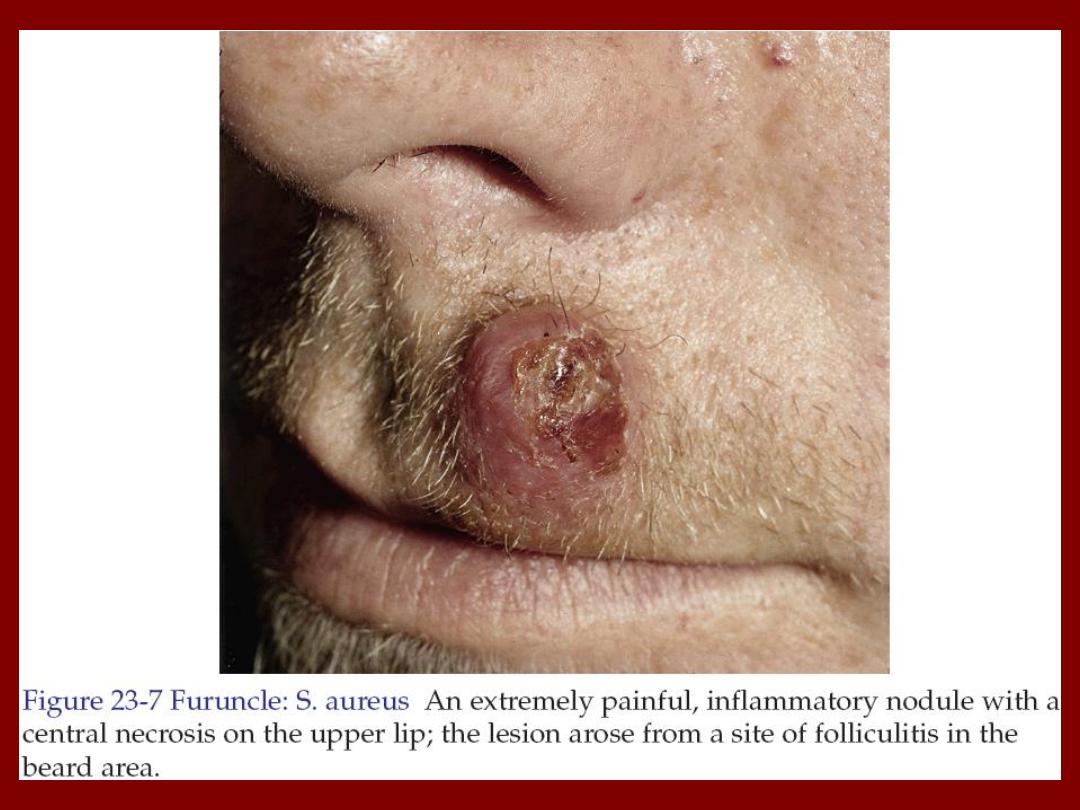
Furuncles and Carbuncles
• Furuncle is a walled-off collection of pus that
is a painful, firm or fluctuant nodule or
abscess that evolves from folliculitis.
• Staphylococcus aureus is the most common
pathogen.
• Lesions favor areas prone to friction or minor
trauma such as underneath a belt, buttocks
or axillae.
Furuncle (Boil)

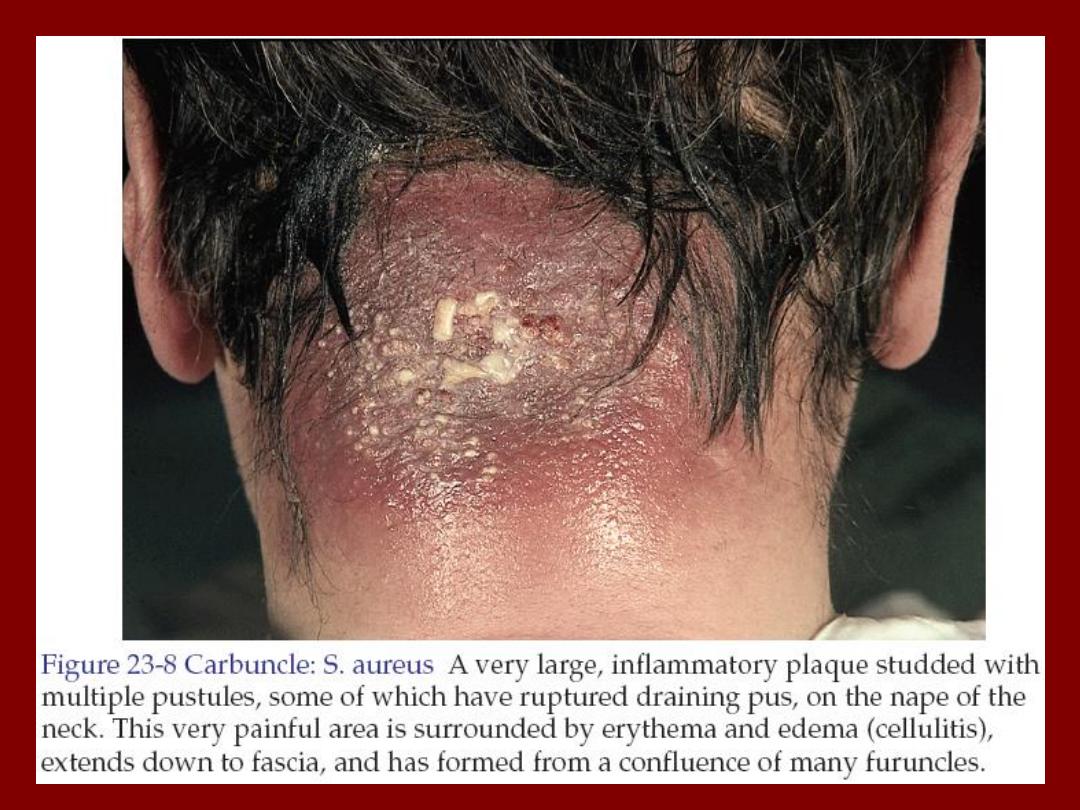
• Carbuncle is an aggregate of infected
follicles.
• The infection originates deep in the dermis
and the subcutaneous tissue consisting of
interconnecting abscesses usually arising in
several contiguous hair follicles forming a
broad red swollen deep painful mass that
points and drains through multiple openings.
Carbuncle

Abscess
• An abscess is a circumscribed collection of pus
appearing as an acute or chronic localized
infection and associated with tissue destruction.
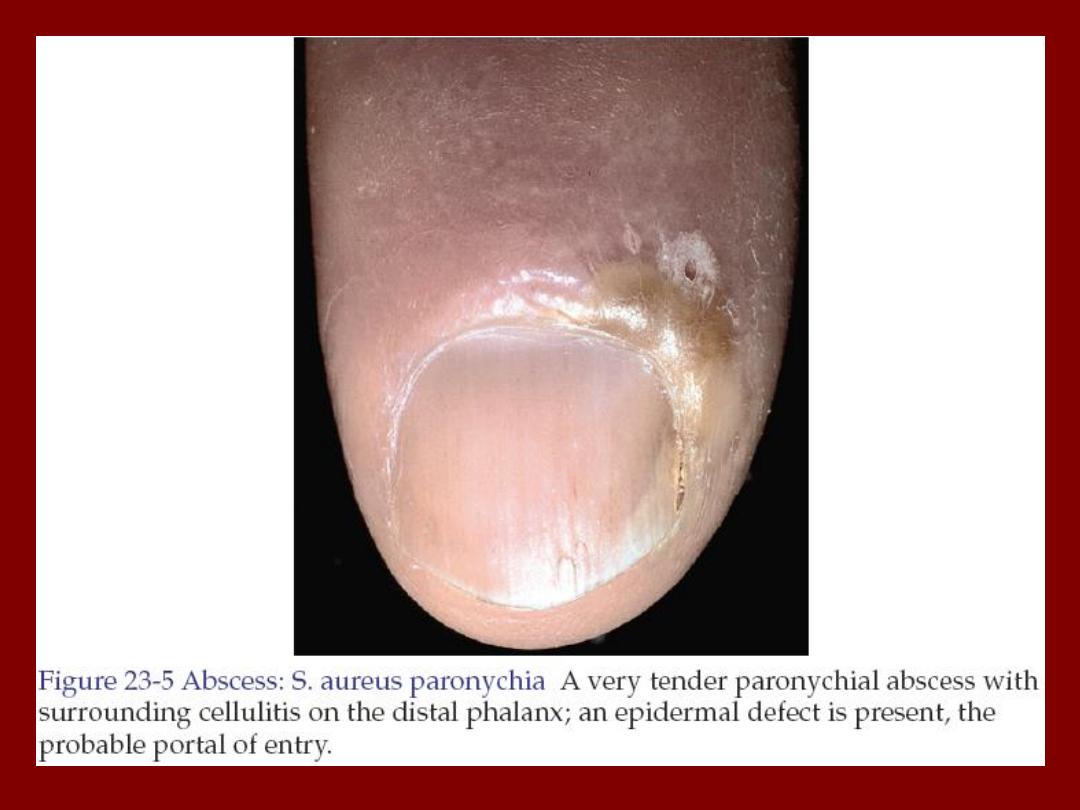
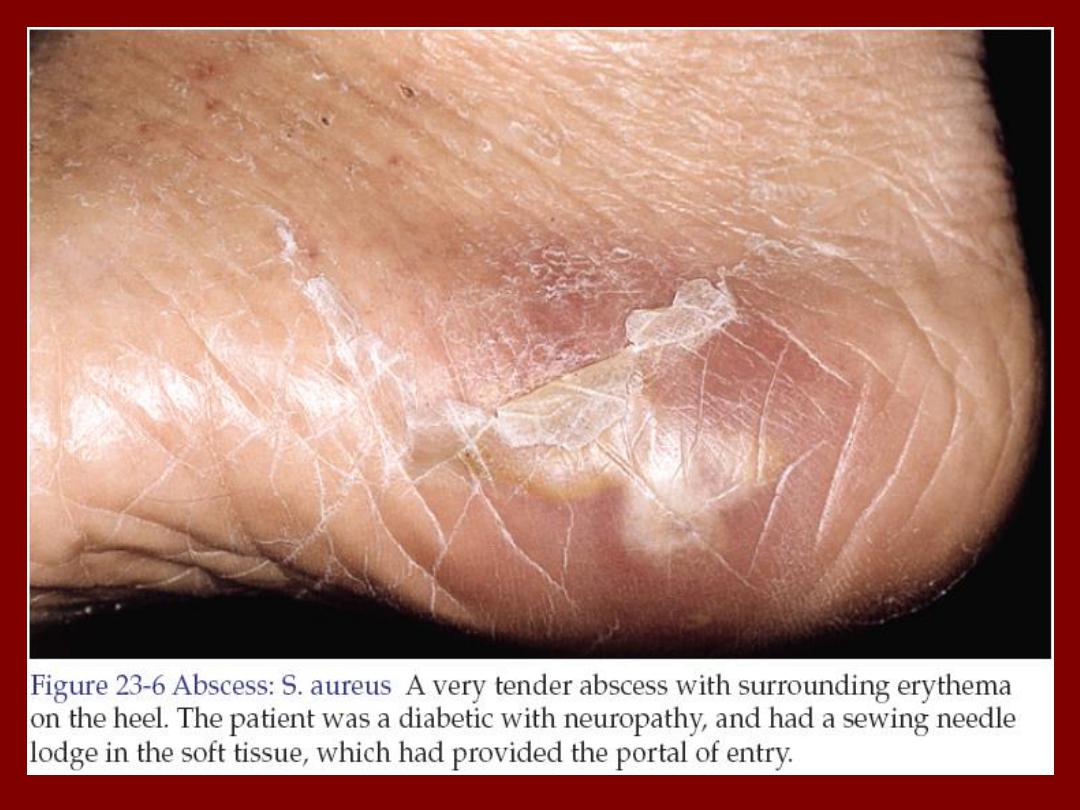

Treatment
• Many furuncles are self-limited and respond
well to frequent applications of a moist warm
compress.
• The primary management of cutaneous
abscesses should be incision and drainage.
The abscess is not ready for drainage until the
skin has thinned and the underlying mass
becomes soft and fluctuant.
• Antistaphylococcal antibiotics for 5-10 days
like cloxacillin, or flucloxacillin.

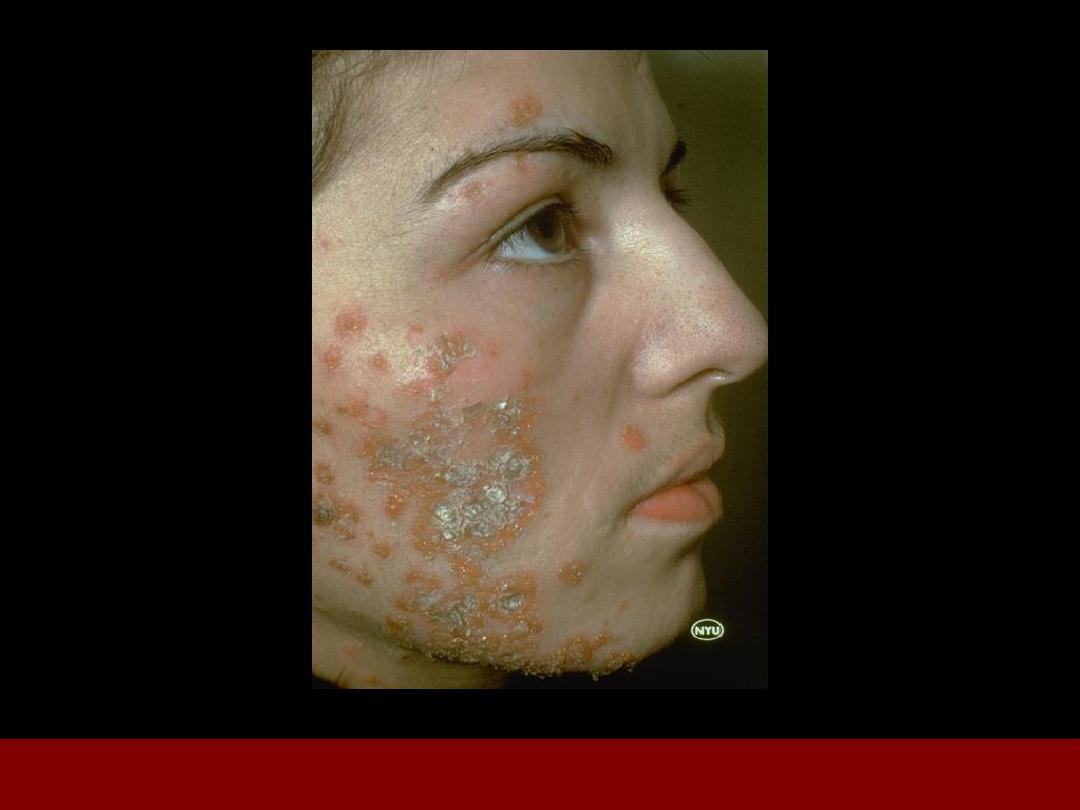
Sycosis barbae
• It implies subacute or chronic pyogenic infection
of the entire depth of the hair follicle in the
beard and moustache areas.
• Staphylococcus aureus is the most common
pathogen.
• It begins with appearance of papules and
pustules and rapidly becomes more diffuse as
shaving continues. They may coalesce to form
plaques studded with pustules.

• The condition should differentiated from tinea
barbae which is a dermatophyte fungal
infection.
– Fungal infections tend to be more severe,
producing deeper and wider areas of inflammation
while bacterial infections usually present with
discrete papules and pustules.
– Hair pulling is easy in fungal infections while difficult
and painful in bacterial infections.
– Hair should be removed and examined for fungi by
KOH examination and the purulent material should
be cultured and examined by gram stain.
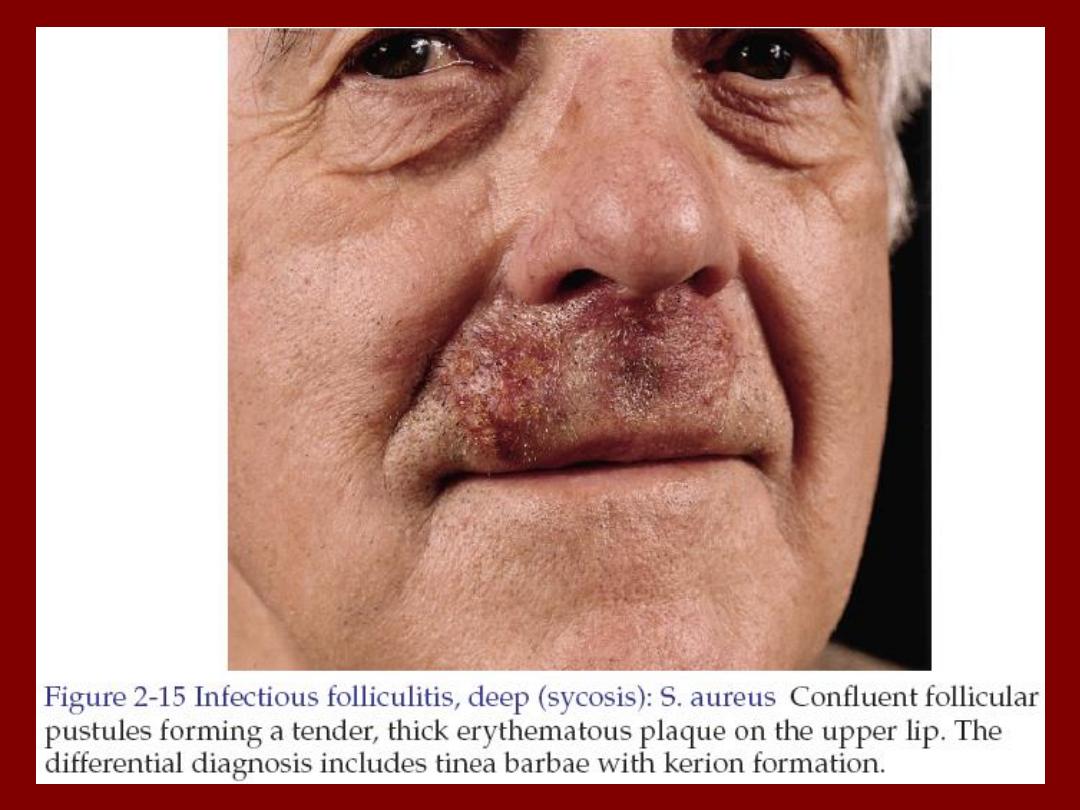

Treatment
• Localized inflammation is treated with topical
antibiotics like fucidic acid cream.
• Extensive disease is treated with oral
antibiotics like cephalexin 500 mg 6 hourly
orally for at least 2 weeks.

Erythrasma
• It is a mild, chronic, localized superficial
infection of the skin caused by bacteria known
as Corynebacterium minutissimum.
• It affects mainly toe clefts, groins, axillae,
intergluteal and submammary flexures.
• There are irregular sharply marginated red-
brown patches. Either smooth in new lesions or
finely creased or scaly in older ones.
• Usually the lesions are symptomless or with
occasional itching.
• Gives coral-red fluorescence under wood’s light

Erythrasma
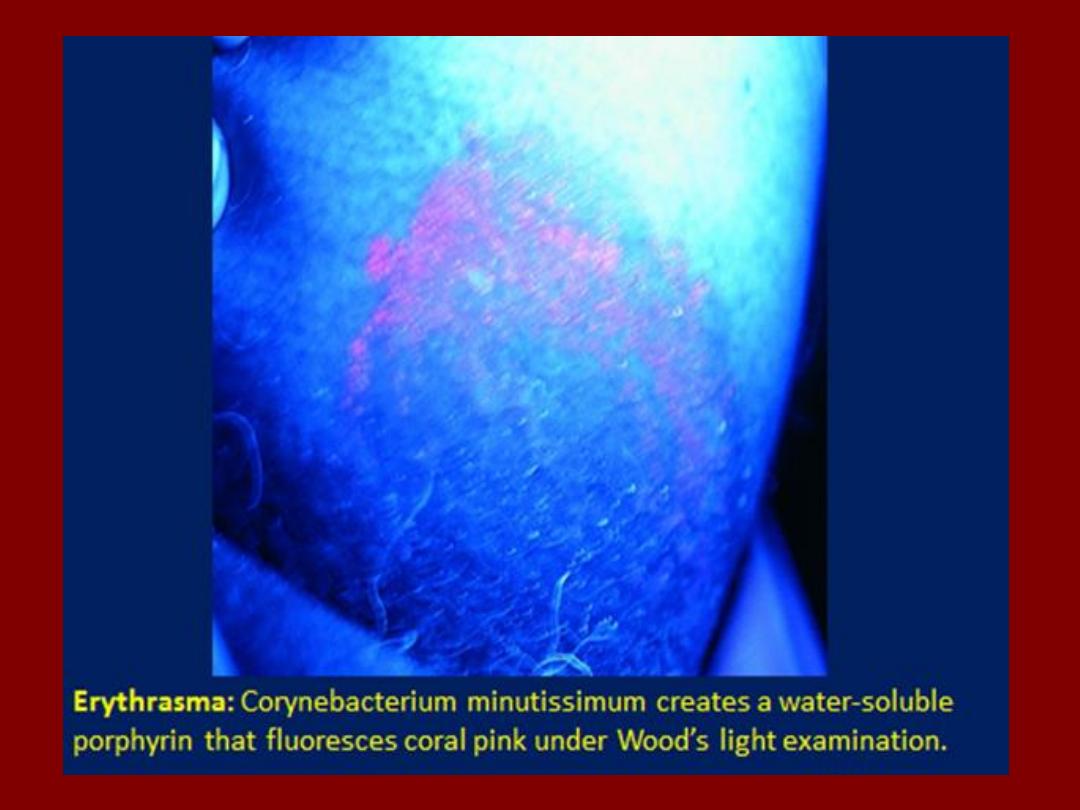

Treatment
• Topical erythromycin for 2 weeks.
Or
• For extensive lesions erythromycin orally
250mg 6 hourly for 10 days.

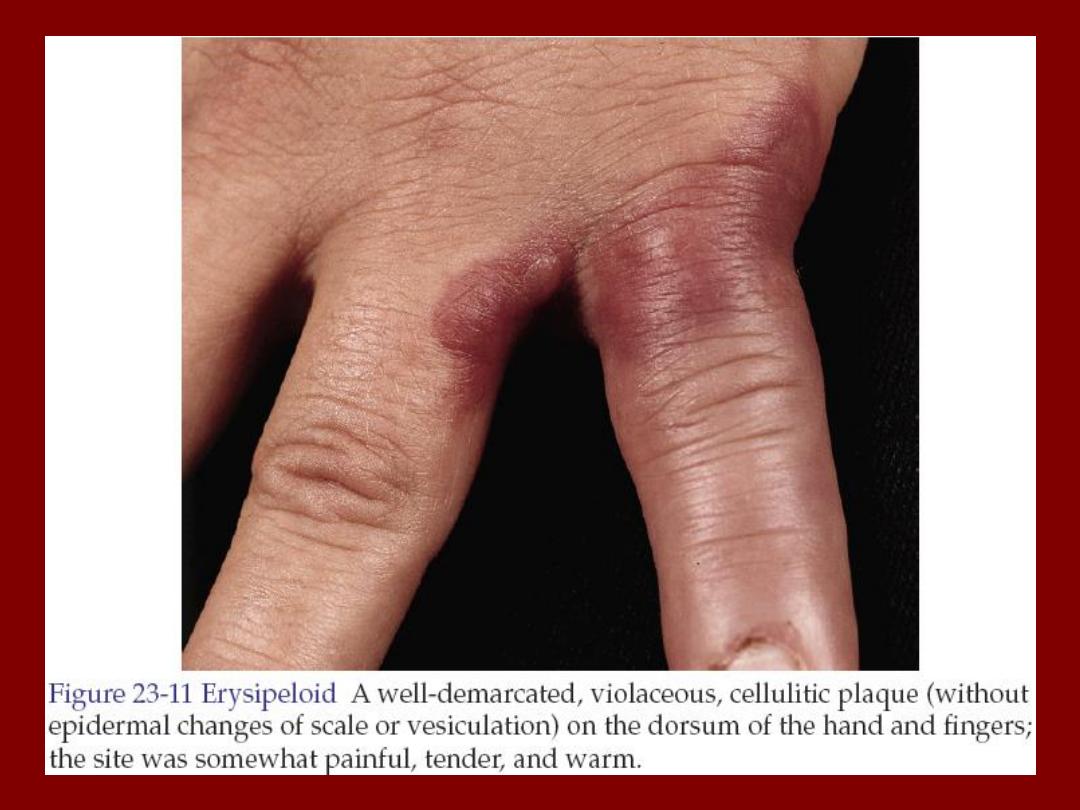
Erysipeloid
• It is an acute infection of skin with Erysipelothrix
rusiopathiae.
• The disease is transmitted from animals so it is
common in butchers, cooks, fishermen, farmers
and veterinary surgeons.
• In the localized cutaneous type, there is
violaceous and tender erythema on the
inoculation site with extending irregular sharp
border. Hands, fingers and forearm are
common sites.

Treatment
• It is self-limited disease heals without sequel
within 2 weeks.
• In rare severe systemic infection erythromycin
or ciprofloxacin.

Good luck
