1
Fifth stage
Pediatric
Lec. 1
.د
ايمان
9
1 /4/2017
Pediatric Poisonings
Definition of Poisoning:
Exposure to a chemical or other agent that adversely affects functioning of an
organism.
• Circumstances of Exposure can be: -Intentional, accidental, environmental, medicinal
or recreational.
• Routes of exposure can be:-
Ingestion, injection, inhalation or cutaneous exposure.
• usually it involves children younger than 6 yrs
“All substances are poisons...the right dose separates poison from a remedy.”
Important history points
• What toxic agent/medications were found near the patient?
• What medications are in the home?
• What approximate amount of the “toxic” agent was ingested?
How much was available before the ingestion?
How much remained after the ingestion?
• When did the ingestion occur ?
• Were there any characteristic odors at the scene of the ingestion?
• Was the patient alert on discovery?
Has the patient remained alert since the ingestion?
How has the patient behaved since the ingestion?
• Does the patient have a history of substance abuse?

2
SPECIFIC management:
ABC’s of Toxicology:
• Airway
• Breathing
• Circulation
• Drugs:
Resuscitation medications if needed
Universal antidotes
• Draw blood:
chemistry, coagulation, blood gases, drug levels
• Decontaminate
• Expose / Examine
• Full vitals / Foley / Monitoring
• Give specific antidotes / treatment
Decontamination:
1. Ocular:
– Flush eyes with saline
2. Dermal:
– Remove contaminated clothing
– Brush off
– Irrigate skin
3. Gastro-intestinal:
– Activated charcoal:
May Prevent /delay absorption of some drugs/toxins
Almost always indicated Only in the 1
st
hour !!!!
– Naso/oro-gastric Lavage
– Bowel Irrigation:

3
Used in recent ingestions
In awake alert patient
By using 500 cc NS Children / 2000cc adults
Orally / Nasogastric tube
A. Asymptomatic child
1) If the toxin is known, the potential danger can be assessed .
Risk assessment will generally take into account the following:
1. the dose ingested (mg/kg)
2. the time interval since ingestion
3. the presence of any clinical signs
2) Observe the Child usually 4-6 hours & consider evaluation of the home situation.
B. Symptomatic child
Management is based on four general principles:
a. Supportive care
b. Preventing or minimizing absorption
c. Enhancement of excretion
d. Administration of antagonist
Attention to the ABCs is always the first priority.
Treat the patient, not the poison!!!
Ongoing assessment and serial vital signs are particularly important.
4
A: Establish a patent airway
B: Provide supplemental oxygen and assist ventilations, if needed.
C: Monitor the circulation:
1. Establish a large-bore IV line and draw blood (CBC with platelets, basic metabolic
profile, serum CO2, toxicology screen, and specific drug levels if indicated).
2. Blood pressure
a. Hypotension
Regardless of the etiology, most hypotensive children respond to10-20 cc/kg
boluses of Ringer's Lactate or Normal Saline.
b. Hypertension should be treated in order to prevent intracranial hemorrhage or
hypertensive encephalopathy.
Treat with Na nitroprusside with or without esmolol or propranolol.
3. Monitoring: Place the child on a cardiorespiratory monitor
a. Arrhythmias are often caused by hypoxia or electrolyte imbalances.
1) For ventricular tachycardias…………lidocaine
2) For sympathomimetic-induced tachycardias…………esmolol
3) For wide complex tachycardias……………NaHCO3
b. Assess the child's mental status. Use the Glasgow coma scale.
The most common cause of death in the comatose child is respiratory failure.
In all comatose or convulsing children, check blood glucose and administer 2-4 cc/kg 25%
DW if needed.
c. Temperature
1. Hyperthermia may be caused by a variety of drugs or toxins.
Treat it aggressively with skin cooling.
2. Hypothermia : it may result from particular agents or be related to environmental
exposure.
Gradual warming with warm blankets, and warmed IV fluids utilizing devices.
5
d. Urine
1. Observe urine output & color
2. Send urine specimens to the lab for urinalysis, toxicology.
X-rays
1. Chest – Evaluate for infiltrates, possible aspiration, and pulmonary edema.
2. Abdominal - Look for radiopaque materials, such as iron .
GI Decontamination
The goal of gastric decontamination is to minimize exposure of the toxin by removing it
from the GIT, or by binding it to a non-absorbable agent.
Ipecac-induced emesis - Syrup of ipecac may be of some value if given within a few minutes
after ingestion. In the ED, ipecac usage is reduced since its efficacy is diminished if
administered 60min or more after ingestion.
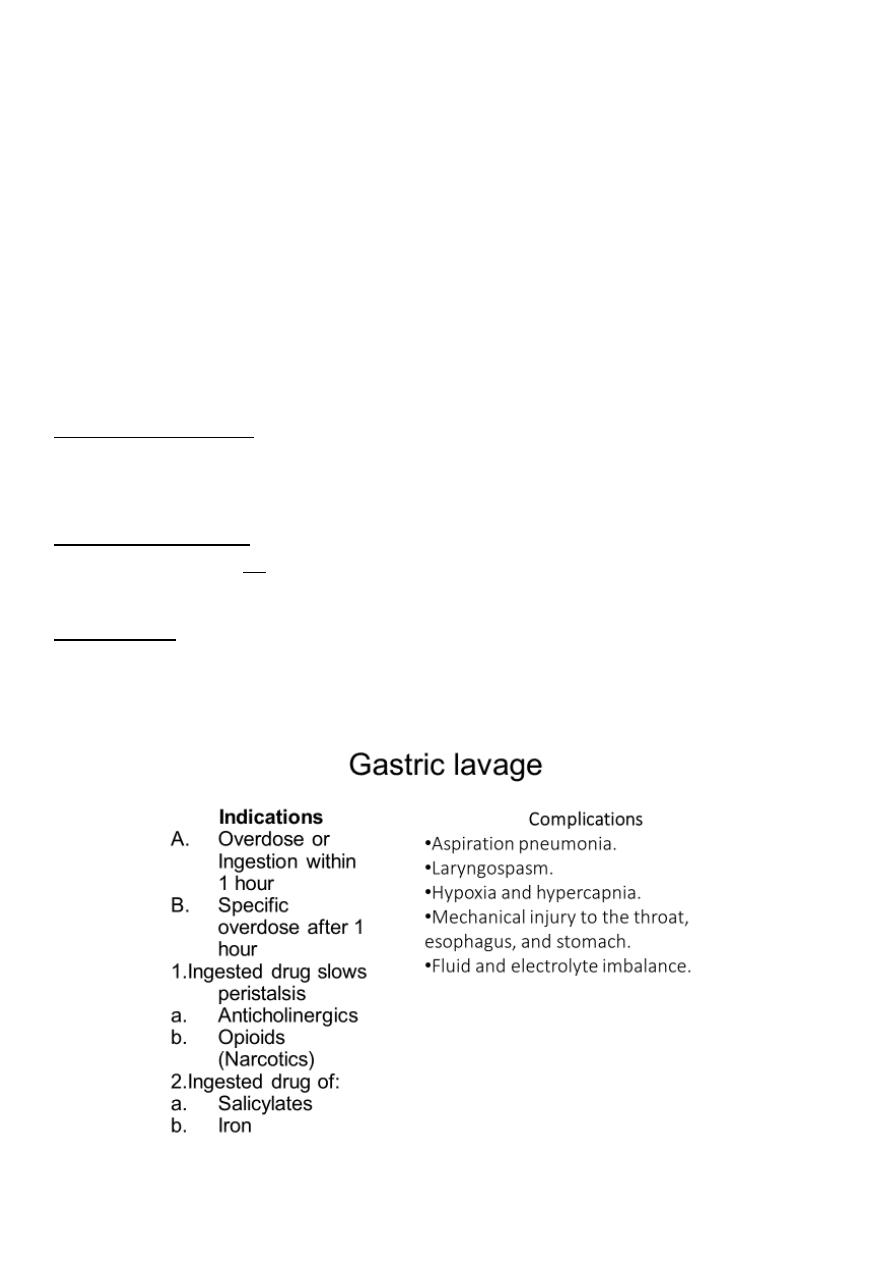
Gastric lavage - gastric lavage appears to be slightly more effective than induced emesis.
Its used when vomiting is contraindicated as a child with a depressed level of
consciousness, seizures, compromised gag reflex, respiratory distress, or ingestion of a
petroleum distillate.
6
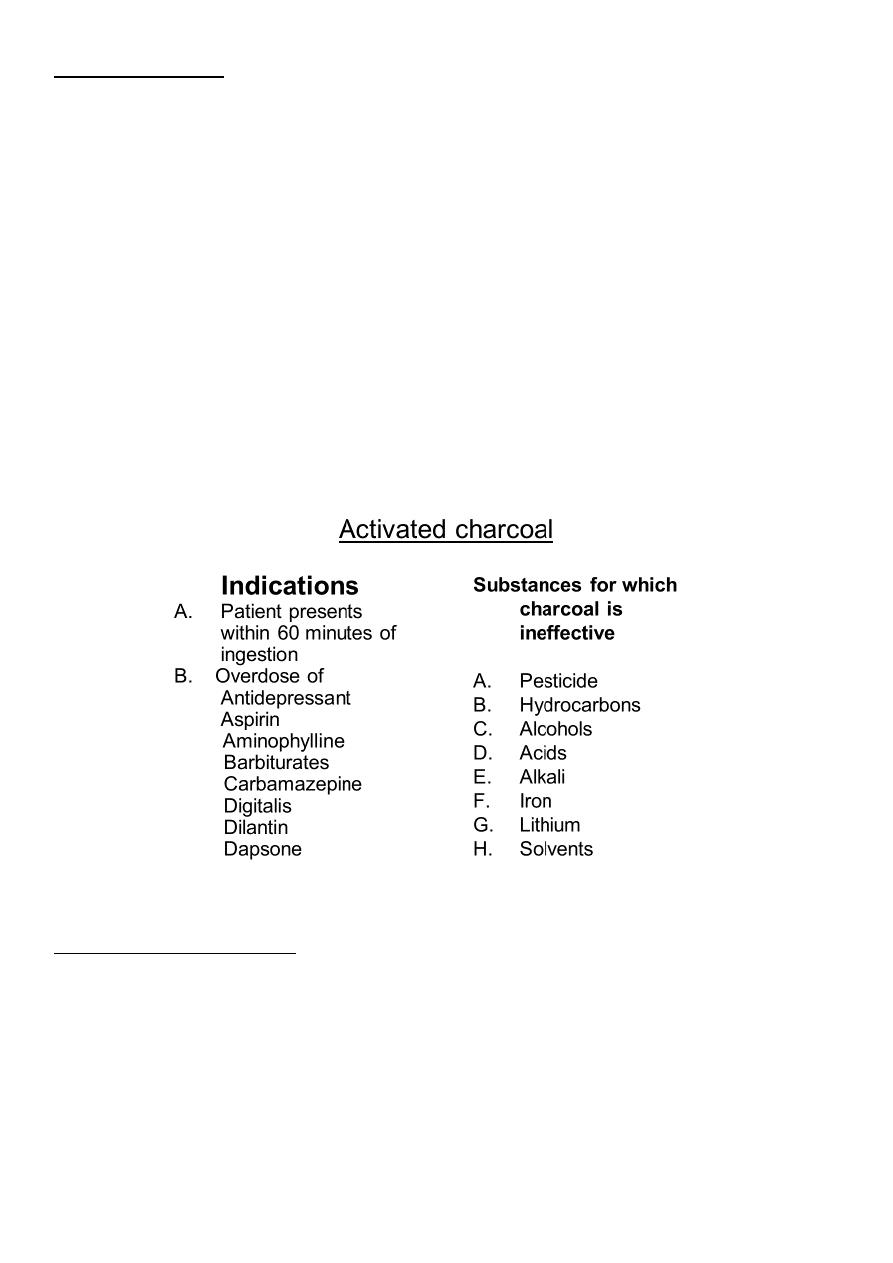
Activated Charcoal:
Decrease or prevent the intestinal absorption of a few drugs and toxins as well as enhance
the elimination of drugs already absorbed and present within the systemic circulation .
specially prepared to have a very large adsorptive surface area.
Many, but not all, toxins are adsorbed onto its surface.
Dose of 10–50 g (≈1 g/kg) for a child and 50–100 g for an adolescent or an adult is
administered. In practice.
Airway reflexes must be preserved or the airway
protected by endotracheal intubation.
Many children will not drink the needed dose; therefore, it may be necessary to administer
activated charcoal via NG tube.
Whole bowel irrigation WBI
uses polyethylene glycol solution ( Colyte) in large volumes at rapid rates to mechanically
cleanse the GI tract.
Enhancing elimination
Forced diuresis: using I.V. fluid & diuretic to increase GFR and enhances elimination.

7
Urinary alkalinization
Administering sodium bicarborate i.v results in an alkaline urine
Hemodialysis:
Renal dialysis effectively removes select drugs.
Exchange transfusion:
a. severe Methemoglobinemia b.Hemolysis
