Objectives
1-To define congestive heart failure(C.H.F).2-To summarize the causes and pathophysiology of (C.H.F).
3-To make a plan for the diagnosis and treatment of (C.H.F).
4-To outline the important steps and drugs in managing (C.H.F).
Congestive Heart Failure
DefinitionCongestive heart failure (CHF) is a clinical syndrome in which the heart is unable to pump enough blood to the body to meet its needs, to dispose of systemic or pulmonary venous return adequately, or a combination of the two
Causes
By far the most common causes of CHF in infancy are congenital heart diseases (CHDs).Beyond infancy, myocardial dysfunctions of various etiologies are important causes of CHF.
Tachyarrhythmias and heart block can also cause heart failure at any age
Among the rare causes of CHF are metabolic and endocrine disorders, anemia, pulmonary diseases, collagen vascular diseases, systemic or pulmonary hypertension, neuromuscular disorders, and drugs such as anthracclines.
Symptoms:-
In infants poor feeding, failure to thrive, tachypnea, and diaphoresis with feeding.
Older children may present with shortness of breath, easy fatigability, and edema.
Physical examination
Findings depend on whether pulmonary venous congestion, systemic venous congestion, or both are present. Tachycardia, a gallop rhythm, and thready pulses may be present with either cause.
If left-sided failure is predominant, tachypnea, orthopnea, wheezing, and pulmonary edema are seen.
If right-sided failure is present, hepatomegaly, edema, and distended neck veins are present.
Investigations
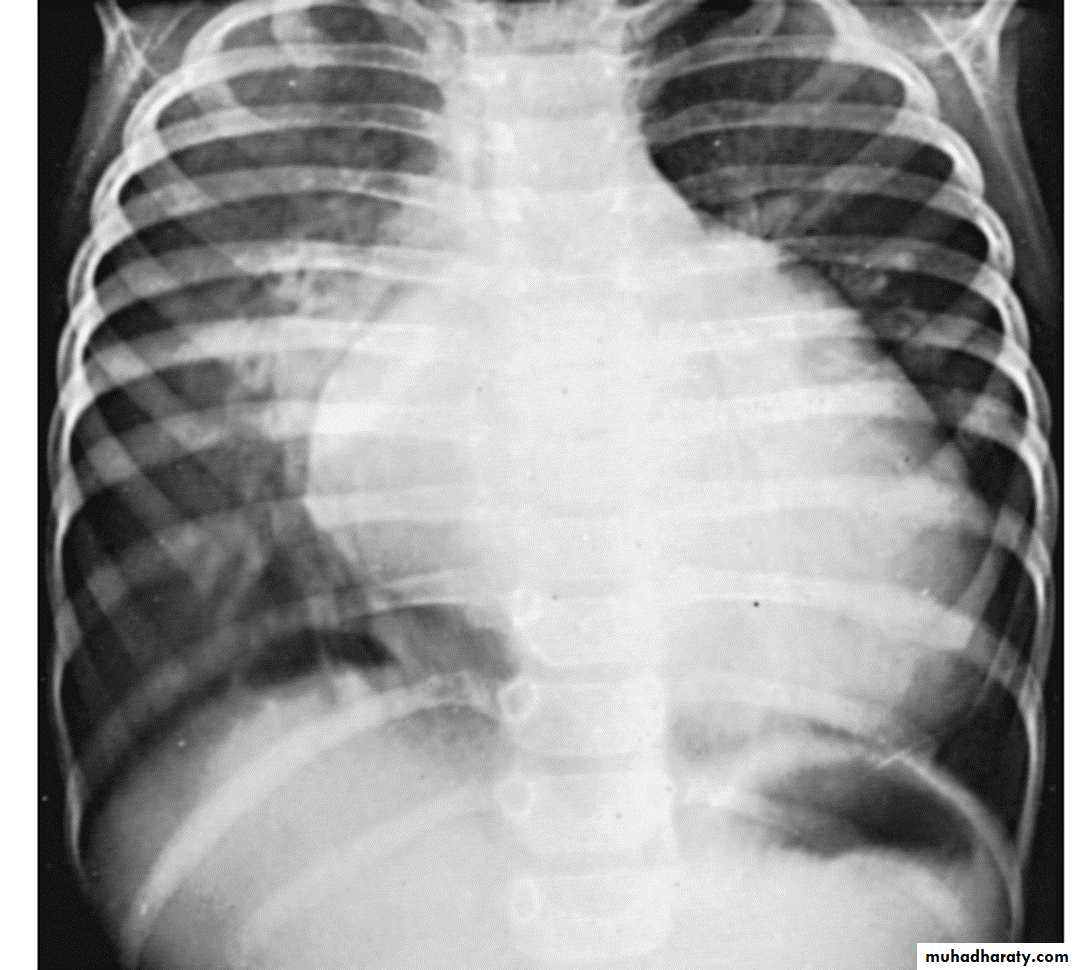
1- Chest-X ray show cardiac enlargement. Pulmonary vascularity is variable and depends on the cause of the heart failure. The cardiothoracic ratio (C/T ratio) is higher than the normal for age.Normal C/T ratios
Infants < 55 %
Older children < 50%
2- Electrocardiography
It is not helpful in
deciding whether CHF is
present or not but it
helps in determining the cause
cause of heart failure.
T
C2
C1
C=C1+C2
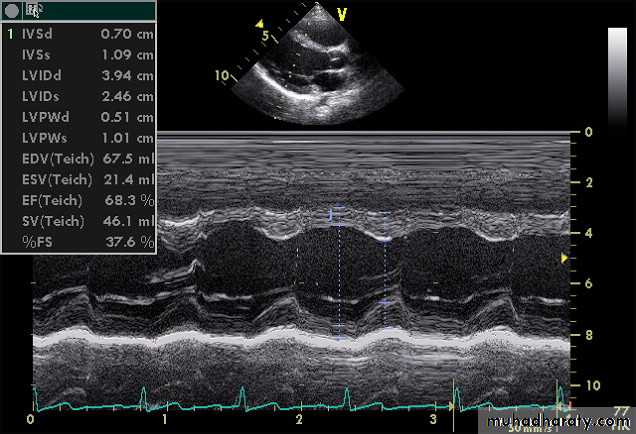
3-ECHOCARDIOGRAPHYEcho studies may confirm enlargement of ventricular chambers and impaired LV systolic function(low fractional shortening or ejection fraction) as well as impaired diastolic function by the use of Doppler techniques.
A more
important
role of echo
may be due
to its ability
to determine
the cause of
CHF. Echo is
also helpful
in serial
evaluation of
the efficacy of
therapy.
Management
A-TRMENT OF UNDTREAERLYING CAUSES OR CONTRIBUTING FACTORs1. When surgically feasible, treatment of underlying congenital heart defects and valvular heart disease is the best approach for complete cure
2. If hypertension is the underlying cause of CHF, antihypertensive treatment should be given
3. If arrhythmias or advanced heart block is the cause of or a factor contributing to heart failure, antiarrhythmic agents or cardiac pacemaker therapy is indicated.
4. If hyperthyroidism is the cause of heart failure, this condition should be treated.
5. Fever should be controlled with antipyretics.6. When there is a concomitant infection, it should be treated with appropriate antibiotics.
7. For anemia, packed cell transfusion is given to raise the hematocrit to 35% or higher.
B- GENERAL MEASURES
1. A “cardiac chair” or“infant seat” is used to keep
infants ina semiupright
position torelieve respiratory
distress.
2. Oxygen (40% to 50%) with humidity is given to relieve hypoxia.
3. Adequate calories (150 to 160 kcal/kg/day ) and fluid should be provided to permit appropriate weight gain. Infants in CHF.
4. In older children, salt restriction (<0.5 g/day) and avoidance of salty snacks (chips, pretzels) and table salt are recommended.
5. Bed rest remains an important component of management. The availability of a television screen and computer games for entertainment ensures bed rest in older children
6. If respiratory failure accompanies cardiac failure, intubation and positive-pressure ventilation are occasionally required. Respiratory failure usually signifies that surgical intervention will be needed for CHDs when the patient is stabilized.
7. Daily weight measurement is essential in hospitalized patients.
.
C-DRUG THERAPY
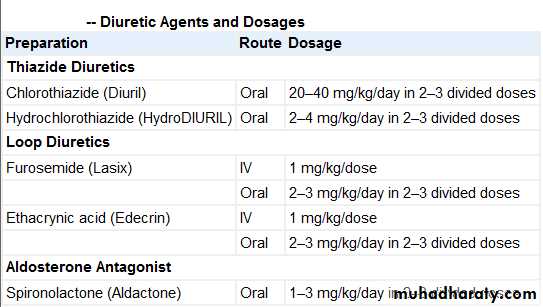
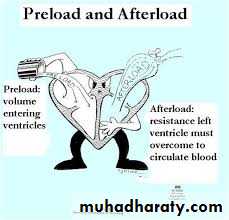
1-DiureticsDiuretics reduce preload and improve congestive symptoms but do not improve cardiac output or myocardial contractility .
2-Digitalis Glycosides
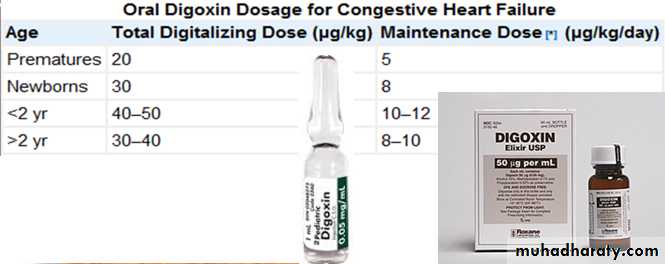
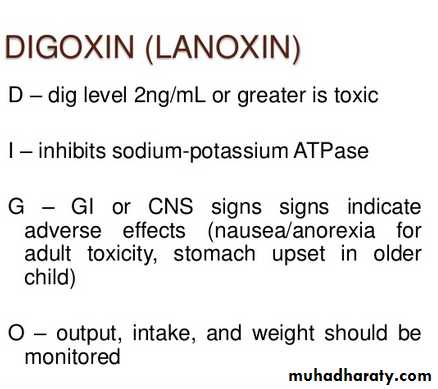
Digoxin is the digitalis glycoside used most often in pediatric patients. Its half-life of 36 hr is long enough to allow daily or twice-daily use. Rapid digitalization of infants and children in heart failure may be carried out intravenously. The dose depends on the patient's age . The recommended digitalization schedule is to give half the total digitalizing dose immediately and the succeeding two one-quarter doses at 12 hr intervals later.
The electrocardiogram must be closely monitored and rhythm strips obtained before each of the three digitalizing doses. Digoxin should be discontinued if a new rhythm
disturbance is noted.
Prolongation of the P-R
interval is not necessarily an
indication to withhold
digitalis, but a delay in
administering the next dose
or a reduction in the dosage
should be considered.
Maintenance digitalis therapy is started ≈12 hr after full digitalization. The daily dosage is divided in two and given at 12 hr intervals for more consistent blood levels and more flexibility in case of toxicity. The dosage is one quarter of the total digitalizing dose. For patients who are initially given digitalis intravenously, maintenance digoxin can be given orally once oral feedings are tolerated. Because absorption from the gastrointestinal tract is less certain, the oral maintenance dose is usually 20–25% higher than when digoxin is used parenterally.
D
G
I
O
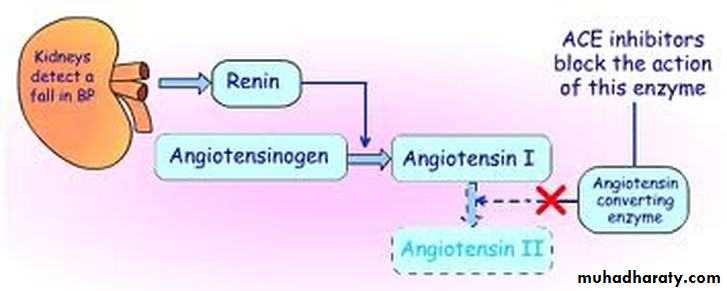
3-Afterload-Reducing Agents and ACE Inhibitors
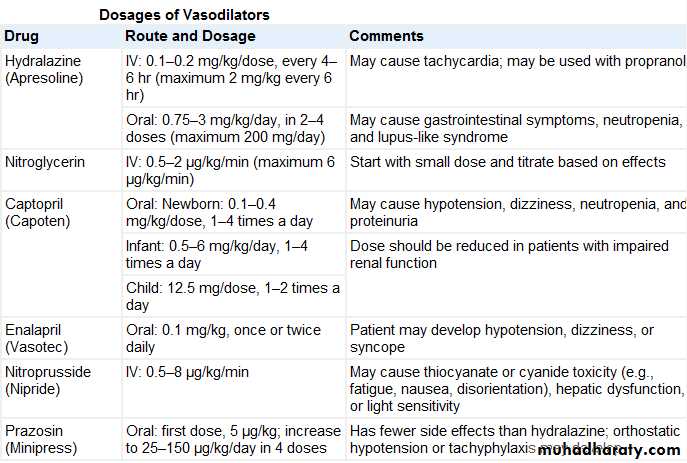
Reducing afterload tends to augment the stroke volume without a great change in the contractile state of the heart and therefore without increasing myocardial oxygen consumption . When a vasodilator is used with an inotropic agent, the degree of improvement in the inotropic state as well as in congestive symptoms is much greater than when a vasodilator alone is used.Decreasing afterload the SV
After load reducing agents types
1. Arteriolar vasodilators (hydralazine) augment cardiac output by acting primarily on the arteriolar bed.2. Mixed vasodilators include ACE inhibitors (captopril, enalapril), nitroprusside, and prazosin. These agents act on both arteriolar and venous beds.
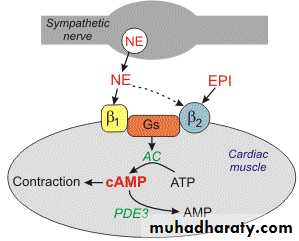
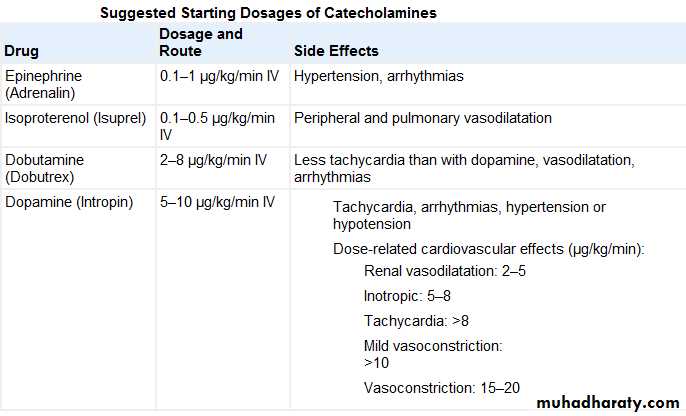
4-α-and β-Adrenergic Agonists(Rapidly Acting Inotropic Agents.)
These drugs are usually administered in an intensive care setting, where the dose can be carefully titrated to hemodynamic response. These agents possess inotropic and vasodilator actions and thus are useful in acute situations. Inotropic agents increase the contractile property of the myocardiumtoward the normal curve.
Amrinone is a
noncatecholamine agent
that exerts its inotropic
effect and vasodilator effects
by inhibiting
phosphodiesterase enzyme.
X
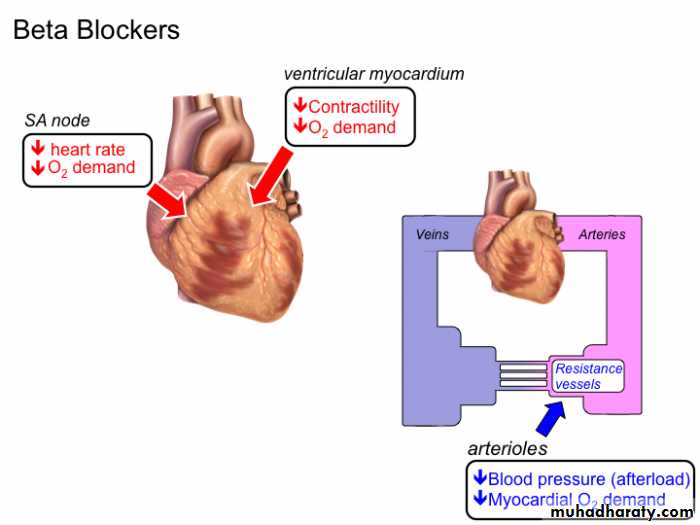
5-β-adrenergic blocking agents
The agents most often used are metoprolol, a β1-adrenergic receptor selective antagonist, and carvedilol, an agent with both α- and β-adrenergic receptor blocking as well as free radical scavengingeffects. β blockers
are used for
the chronic tre-
atment of patients
with heart failure
and should not be
administered
when patients
are still in the
acute phase of
heart failure .