OPERATIVE OBSTETRICS
FORCEPS DELIVERYComponents of Forceps
Blade
cephalic curve
pelvic curve
Shank
parallel
crossing
Lock
Handle
Classification of Forceps Delivery
Outlet ForcepsLow Forceps
Midforceps
High Forceps
no place in modern obstetrics
Classification of Forceps Delivery According to Station and Rotation
Outlet Forceps
1. Scalp is visible at the introitus without separating the labia
2. Fetal skull has reached the pelvic floor
3. Sagittal suture is in anteroposterior diameter or right or left occiput anterior or posterior position
4. Fetal head is at or on perineum
5. Rotation does not exceed 45 degrees
Low Forceps
1. Leading point of fetal skull is at station >/= +2 cm, and not on the pelvic floor
2. Rotation is 45 degrees or less (LOA/ROA to OA or LOP/ROP to OP)
3. Rotation is greater than 45 degrees
Midforceps
1. Station above +2 but head is engaged
High Forceps
not included in classification
Kinds of Forceps
Simpson forceps
Has a fenestrated blade and wide shank in front of the English-style lock
Used to deliver the fetus with a molded head, as is common in nulliparous women
Tucker-Mc Lane forceps
The blade is solid and the shank is narrow
Used for the fetus with a rounded head, which more characteristically is seen in multiparas
Kielland forceps
Characterisitc features are the sliding lock, minimal pelvic curvature, and light weight
More specialized forceps
Used in cases of deep transverse arrest with the fetal head in the transverse position well down in the pelvis with the occiput below the spines
Piper forceps (Laufe forceps)
Used to deliver the aftercoming head of the breech-presenting fetus
Uses of forceps
1. Maternal or fetal indications
2. Prophylactic
3. Elective
Vaginal Operations: Forceps Delivery
Indications
any condition threatening the mother or fetus that is likely to be relieved by delivery
Maternal Indications
1. heart disease
2. pulmonary compromise or injury
3. intrapartum infection
4. certain neurological conditions
5. exhaustion
6. prolonged second stage
Fetal indications
1. prolapse of umbilical cord
2. premature separation of the placenta
3. non-reassuring fetal heart rate pattern
Vaginal Operations: Forceps Delivery
Pre-requisites for application
head engaged
presentation vertex or chin anterior
position known
cervix completely dilated
membranes ruptured
no disproportion between head & pelvis
: prerequisites for instrumental delivery
Fully dilated cervix
One-fifth or nil palpable abdominally
Ruptured membranes
Contractions present
Empty bladder
Presentation and position known
Satisfactory analgesia
Morbidity
A. Maternal
1. episiotomy & lacerations
2. urinary and rectal incontinence
3. febrile morbidity
B. Fetal
1. apgar scores
2. cephalhematoma
3.caput
4. trauma
5. bilirubin
retinal hge 6-
Long term morbidity
?cerebral palsy? I.Q.
Summary
1. Forceps delivery, when performed inappropriately, can result in maternal and fetal adverse effects.
2. Outlet & low-forceps operations of 45°or less can be safely performed if the basic guidelines are met.
Trial Forceps
Operator attempts delivery with the full knowledge that vaginal delivery may not be successful.
If application cannot be achieved, it is abandoned and delivery accomplished either by CS or vacuum extraction
Failed Forceps
Successful application with gentle pulls made but no descent is achieved.
The procedure is then abandoned and cesarean section is performed.
Vaginal Operations: Vacuum Extraction
Principle
Creation of an artificial caput by attaching a traction device by suction to the fetal scalp
Indications & pre-requisites
Same as in forceps delivery
Technique
Center of the cup should be over the sagittal suture about 3 cm. in front of the posterior fontanelle
The pressure is slowly raised 0.1 kg/cm/min. until it reaches
0.8 kg/cm. The Total time taken should be about 8 minutes.Contraindications
Malpresentation (face, brow, breech transverse lie)
More than borderline CPD (trial of VE)
Cx insufficiently dilated to permit application of a 50mm cup
Uncooperative patient
Suspected fetal coagulopathy
In experienced accoucheur
Advantages of vacuum
Easy rotation of fetal head from OP or OT to OA position (Auto rotation)
Relatively low trauma rate to mother and fetus.
Maternal
Infant
Vaginal and cervical laceration
Episiotomy
Perineal tears
Post partum haemorrhage
Infections in the peuperium
Subgaleal haemorhage
Intracranial haemorrhage
Cephalhaematoma
Neonatal jaundice
Cerebral irritation and asphyxia
Scalp effects (Chignon, necrosis and scars) retinal haemorrhage
Complications from use of vacuum
DESTRUCTIVE VAGINAL OPERATIONS
Done usually as a sequalae to difficult and obstructed labour when the fetus is deadAlways an emergency procedure done to relieve an obstruction in maternal interest
Obstruction may be due to CPD malpresentation or malposition
They are often not done in this country for many reasons
a-Acceptability
b-Experience
c-Associated complication
d-Decling rate of obstructed labour
e-Safety of c/s
f- literacy level
Types of D operation done:
Craniotomy 61%
Decapitation 32%
Cleidotomy 7%
Embryotomy 0.9%
Describe each procedure
Morbidity associated with destructive operation:
Peuperal sepsis
Post partum haemorrhage
Vaginal/cervical laceration
Perineal tear
Ruptured uterus
Bladder laceration
VVF
RVF
Endotoxic shock
Peurperal psychosis
Maternal death
Symphysiotomy:
Alternative to c/s when there is CPD or to prevent the entrapment of the after coming head of breech
Artificial separation of the sympysis pubis with a scalpel blade in order to enlarge the pelvic diameter to facilitate the process of birth
Complications Associated with Symphysiotomy
Vesicovaginal Fistula
Osteitis Pubis
Retropubic Abscess
Stress Incontinence
Long Term Walking Disability / Pain
Indications
CPD with vertex presentation and a live fetus
Failed trial of vacuum extraction /forceps in 2nd stage of labour
Breech presentation to prevent entrapment of the after coming head
INJURIES TO SOFT TISSUE
INJUR TO VULVA:
MINOR TEAR OF LABIA MINORA, FOURCHETTE COMMON NO TREATMENT
VULVAL HEMATOMA:
BLEEDING FROM PARAVAGINAL VEINS
TENSE, BLUISH & TENDER
LARGE: INCISION & CLOTS REMOVED
HAEMATOMAS
Vulval and paravaginal haematomas
Definition
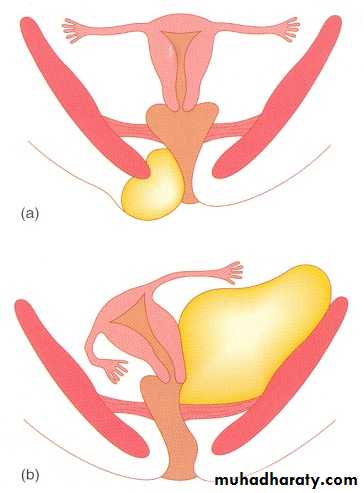
1. Infralevator haematomas include those of the vulva and perineum, as well as paravaginal haematomas and those occurring in the ischiorectal fossa
2. Supralevator haematomas spread upwards and outwards beneath the broad ligament or partly downwards to bulge into the walls of the upper
vagina.
These haematomas can also track backwards into the retroperitoneal space.
VULVAL & PARAVAGINAL HAEMATOMAS
(a) Vulval
(b) Para vaginal haematomasVULVAL & PARAVAGINAL HAEMATOMAS
Incidence and associationsAn acceptable definition would be any haematoma >4cm in diameter. The incidence of these is approximately 1:1000 deliveries.
The injury if frequently related to
episiotomy
Intact perineum
Diagnosis
Although a vulval haematoma is usually obvious, a paravaginal haematoma may be missed, with no symptoms until shock develops. In general, the symptoms depend upon the size and rate of haematoma formation. Some genital haematomas may be up to 15cm in diameter.
Management
1. Resuscitative measure
2. Surgical evacuation of the haematoma
- haematoma is <5cm in diameter
- not expanding
Observation to limit haematomas
1. Ice packs
2. Pressure dressings
3. Appropriate analgesia
Need for surgical interventions
1. Haematomas >5cm in diameter
2. Rapidly expanding
Technique
The incision should be made via the vagina. If a figure of eight suture does not achieve haemostasis, either a drain or a pack can be used.
MANAGEMENT OF HAEMATOMAS
A trap for the unwary – beware occult
haemorrhage in a 'collapsed' postpartum
patient
Large vulval haematomas benefit from
drainage:
- leave the wound open
- leave a drain
Broad ligament haematomas are usually
managed conservatively
INJURIES TO THE CERVIX
After a vaginal delivery, the majority of women will have lacerations and/or bruising of the cervix.
Bleeding does not appear to be arising from the vagina or perineum and which continues despite a well-contracted uterus is an indication for examining the cervix.
Deep lacerations, and particularly those that involve the vaginal vault, need to be managed in theatre under anaesthesia.
A laceration into the vault could extend forward to the bladder or laterally towards the uterine artery at the base of the broad ligament.
Management
Prompt recognition of the injury and action to control the bleeding are essential
Repair
For repairing a cervical tear, good visibility using right-angle retractors is essential. Using two pairs of ring forceps applied to the cervix at any one time, it is possible to inspect the whole circumference accurately. Identification of the apex of the tear is essential before commencing repair.
CERVICAL LACERATION:
SEQUELAE:
INFECTION, PERSISTENT CERVISITIS
EXTENSIVE SCARRING
STERILITY
REPEATED ABORTION
PREMATURE LABOUR
DYSTOCIA
INJURIES TO THE CERVIX
Key Points
The cervix often looks damaged but is
very rarely associated with bleeding
Ventouse prior to full dilation has been
implicated in injury to the cervix
INJURIES TO SOFT TISSUE
PERINEAL TEARS:
GROSS INJURY IS DUE TO MISMANAGED 2ND STAGE OF LABOUR
ETIOLOGY:
OVER STRETCHING OF PERINIUM
RAPID STRETCHING OF PERINIUM
INELASTIC PERINIUM
PERINEAL TEARS:
DEGREES:
First-degree: involve the perineal skin, and vaginal mucosa
Second-degree: 1st degree and the fascia and muscles of the perineal body
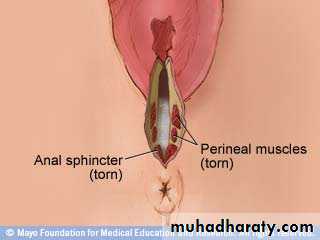
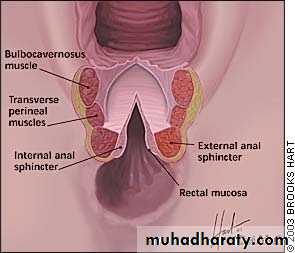
Third-degree: 2nd degree and involve the anal sphincter.
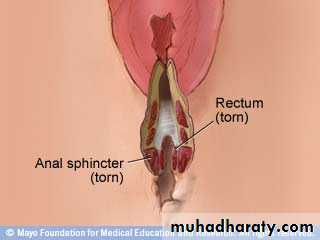
A fourth-degree: extends through the rectal mucosa to expose the lumen of the rectum.
THIRD DEGREE PERINEAL TEAR
FOURTH-DEGREE
PERINEAL TEARINJURIES TO SOFT TISSUE
PERINEAL TEARS:PREVENTION:
LIBERAL USE OF EPISIOTOMY
PROPER CONDUCT OF LABOUR DURING 2ND STAGE
PERINEAL SUPPORT DURING 2ND STAGE
PERINEAL TEARS:
TREATMENT:
SHOULD REPAIR IMMEDIATELY FOLLOWNG PLACENTAL DELIVERY
DELAYED BY 24 HRS DELAYED CLOSURE
DIAGNOSE THE DEGREE OF TEAR
GOOD LIGHT, EXPOSURE & ASSISTANCE
PERINEAL TEARS:
TREATMENT:
LITHOTOMY POSITION
INCOMPLETE TEAR: CONTINUOUS VAGINAL MUCOSA SUTURE
INTERRUPTED TO MUSCLE
MATTRESS TO SKIN
COMPLETE TEAR: TAKE FIRST THE RECTAL MUCOSA AND CONVERT TO INCOMPLETE TEAR
AFTER CARE:
LOW RESIDUE DIET
STOOL SOFTNER
ORAL ANTIBIOTICS: ANAEROBIC
ANALGESICS
VAGINAL LACERATION:
FORCEPS DELIVERIES OR BREECH EXTRACTIONS
OBSTRUCTED LABOUR
TREATMENT:
MINOR TEAR: NO SUTURING
MAJOR LACERATION: REPAIR USING ABSORABL SUTURE
RUPTURE OF UTERUS:
DISRUPTION IN THE CONTINUITY OF UTERINE WALL
INCIDENCE: 0.05% (1 IN 2000)
1-SPONTANEOUS: CONGENITAL MALFORMMATION, OBSTRUCTED LABOUR, GRAND MULTIPARITY
2-SCAR RUPTURE: PREVIOUS CS (1-2%), MYOMECTOMY
3-IATROGENIC: INJUDICIOUS USE OF OXYTOCIN, FORCIBLE ECV/ IPV, FALL OR BLOW OVER THE ABDOMEN, , FORCEPS or BREECH EXTRACTION
TYPES:
INCOMPLETE RUPTURE: PERITONIUM REMAINS INTACT
COMPLETE RUPTURE: SCAR IN UPPER SEGMENT- INVOLVES PERITONIUM
RUPTURE OF UTERUS:
DIAGNOSIS:
DURING PREGNANCY:
PAIN OVER LOWER ABDOMEN
TENDERNESS
SUDDEN ABDOMINAL DISTENSION
FEATURES OF SHOCK
FHS – IRREGULAR OR ABSENT
INJURIES TO SOFT TISSUE
RUPTURE OF UTERUS:
DIAGNOSIS:
DURING LABOUR:
BACKGROUND OF PROLONG OBSTRUCTED LABOUR
SHOCK, COLLAPSED STATE
WEAK & RAPID PULSE, LOW BP
FETAL PART EASILY FELT
INJURIES TO SOFT TISSUE
RUPTURE OF UTERUS:TREATMENT:
RESUSCITATION:
2 WIDE BORE IV CANULA / VENOUS CUT DOWN / CVP
IV FLUIDS: RL / HAEMACCEL
BLOOD CROSS MATCH & TRANSFUSE
MONITOR VITALS, CVP & UO
INJURIES TO SOFT TISSUE
RUPTURE OF UTERUS:TREATMENT:
LAPAROTOMY:
REPAIR: IN CASES OF SCAR RUPTURE WITH CLEAN MARGIN
REPAIR & STERILISATION:
HYSTERECTOMY: LOW GENERAL CONDITION, GRAND MULTIPARA, MORBID DISTORTION OF ANATOMY, INFECTED CASE
Episiotomy:
Episiotomy is a surgically planned incision on the perineum and the posterior vaginal wall during the second stage of labor.
It is also known as Perineotomy.
In modern times, these indications have declined and many obstetricians do not believe in routine use of episiotomy
Episiotomy:
-Eases delivery, protects the head of small baby from trauma – can
be quickly repaired than a ragged tear
Less liable to infection then a brush
-Types-Midline
-Mediolateral
-J-Shaped
Repairs
Problems
After care
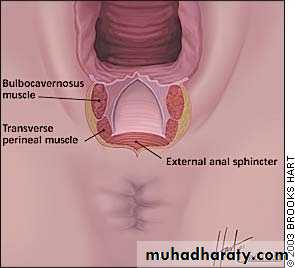
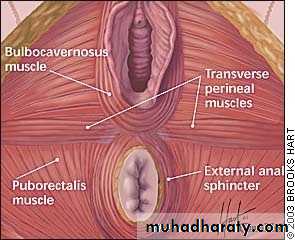
Muscles of perineal body
Episiotomy
A surgical incision into the perineum between the vagina and anus.Prior to instrumental delivery (forceps, vacuum) to widen the vagina
Objective of Episotomy:
To enlarge the vaginal introitus so as to facilitate easy and safe delivery of fetus.
To minimize overstretching and rupture of the perineal muscle and fascia.
To reduce the stress and strain on the fetal head(more for premature baby).
Indications:
1-In rigid/inelastic perineum- primigravida,old perineal scar of episiotomy
2. Anticipated perineal tear- Primi, big baby, face to pubis or face delivery, narrow pubic arch, breech delivery
3. Operative procedure- forcep or vaccum delivery
4.To shorten the second stage-
Heart diseases, severe pre-eclampsia or pre-eclampsia, post C/S cases, postmaturity
5. Foetal Interest- foetal distress, premature baby, breech delivery
Timing of episiotomy:
Bulging thinned perineum during contraction just prior to crowning is the ideal time
Advantages:
A. Maternal – 1.Easy to repair
2.Prevent prolapse
3.Prevent lacerations extending to rectum.
4.Shortening of 2nd stage of labour
B. Foetal- 1.Minimise intracranial injuries in premature baby
2. Reduces foetal asphyxia and acidosis
Following structures are cut from inside – outwards.
a) The posterior vaginal wall
b) The deep and the superficial transverse perineal muscle,the bulbospongiosus and part of the levator ani muscle.
c) The fascia covering the muscle
d) Transverse perineal branches of the pudendal vessels and nerves.
e) The subcutaneous tissue and the skin.
Procedure:
Cleaning and drapingAnesthesia
Incision
- Site and timing
- Technique
Repair:
- Timing and Methods
Post operative care:
Clean wound with clean water after each urination and defaecation.Keep area dry
Apply clean pads
Analgesics if needed
Peri-care and peri-light
Suture removal on 7th -10th post op day if silk is applied.
F/U after 6 wks if no complication
Complications:
Immediate:
- Extension of incision to involve the anal sphincter
- Hemorrhage
- Vulval haematoma : the apex of the incision is not included in the stich.
The dead space in not obliterated properly.
The sprouting vessels if not ligated.
- Wound infection
- Wound dehiscence
- Retention of urine
Remote:
- Dyspareunia
- Rectvaginal fistula, - scar endometriosis
3. Bartolin cyst- if the duct of the bartholins gland is included in the episiotomy wound.
4. Scar endometriosis.
5. Deficient perineum
Prevention of perineal tear:
Well support of the perineum at the time of delivery of head
Delivery by early extension is to be avoided
Spontaneously forcible delivery is to be avoided
To deliver the head in between contraction
To perform timely epsiotomy
To take care during delivery of shoulder
Controversy of Routine Episiotomy
Dorsens incision
Incision made on the cervix at 5 and 7 O’clock or 2 and 8 O’clock to effect the delivery of the after coming head of the breech trapped by the cervix
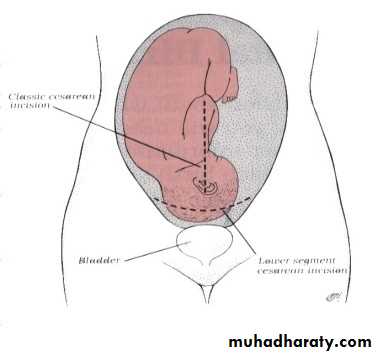
Abdominal Operations: Cesarean Delivery
Birth of a fetus through incisions in
the abdominal wall (laparotomy) and
the uterine wall (hysterotomy).
CESAREAN SECTION CS
TYPES OF CS
Lower segment CS
Classical CS
Indications for classical CS
Transverse lie back down (with SROM)
Structural abnormality that makes lower segment approach difficult (Fibroids)
Anterior Placenta Previa & abnormally vascular lower segment
Poorly developed lower segment in Very preterm fetus in breech presentation
Cervical cancer
INDICATIONS FOR ELECTIVE CS
Repeat CS
Placenta previa
VV fistula repair
HIV (poor controlled)
Active herpes
Fetal macrosomia > 4500 gm
Uterine surgery eg. Hystrotomy, myomectomy
Severe IUGR
Breech
Multiple pregnancy
Transverse lie
Ca of the Cx/ TR obstructing the birth canal
INDICATIONS FOR EMERGRENCY CS
Severe PETAbruptio placenta (APH)
Fetal distress
Failure to progress in the first stage of labour
Cord prolapse
Obstructed labour
Failed induction
Malpresentation brow, chin post, shoulder & compound presentations, breech
Compromised fetus 2ry to DM, HPT, isoimmunization
TIMING OF ELECTIVE CS
Usually at 38-39 wksBefore Emergency CS
Explain to the Pt & husband & obtain consent
Inform anesthetist, OR staff, ped
100% oxygen mask in case of fetal distress
Sodium citrate 20 ml , metoclopramide 10 mg IV
Transfer to the theatre, IV , take blood for Hb, x-match 2 U of blood
Preferable to use spinal or epidural anaethesia
Catheterize the bladder
Tilt the mother 15 º by using wedge
Pneumatic inflatable boots or Ted stockings
Prophylactic Ab ↓↓ incidence of infection
Inform ped if the mother had opiates in the last 4 hrs
Halothane should not be used uterine relaxation & bleeding
COMPLICATIONS
INTRAOPERATIVE
Bleeding & the need for bl transfusion
Hysterectomy
Complications of anaesthesia
Damage to the bladder, ureter, colon , retained placental tissue
Fetal injury
COMPLICATIONS
POSTOPERATIVEParalytic ileus
Wound dehiscence & infection
Infectins UTI, pnemonea
DVT & pulmonary embolism
Fistula
Death
POSTNATAL CARE
V/S & blood loss must be monitered
Uterine fundus palpated
Effective parentral analgesics
Deep breathing & coughing encouraged
Early mobilization
Fluid therapy &diet
Bladder & bowel function
Wound care
Lab
Breast care
Prophylaxis for thrombembolism
MODE OF DELIVERY IN NEXT PREGNANCY
CRITERIA FOR VBAC
Pt must agree to the procedure
A low transverse uterine incision
Non recurrent cause of the previous CS
No macrosomia, malposition, multiple gestation, breech
MODE OF DELIVERY IN NEXT PREGNANCY
Contraindication
Previous classical CS
2 or more previous CS
Previous other uterine surgery
Hx of scar rupture
Placentaprevia or transverse lie
Risk of SCAR RUPTURE
O.5% for LSCS
4-9% for classical
SCAR RUPTURE
Signs OF SCAR RUPTURE
Fetal distress
Ease of fetal palpation
Cessation of contractions
Elevation of presenting part
Scar pain
Bleeding / shock
Abdominal operations: Cesarean Delivery
Criteria for timing of repeat cesarean:
FHT have been documented for 20 weeks by fetoscope or 30 weeks by doppler.
36 wks. Since a +serum or urine HcG
US with CRL at 6-11 wks compatible with 39 wks.
US at 12-20 wks compatible with 39 weeks determined by clinical Hx & PE
Abdominal Incisions
1-Vertical Incision
quickest to make
greater chance of dehiscence
2. Pfannenstiel Incision
cosmetically better, stronger
less chance of dehiscence
exposure not as good
Abdominal Operations: Cesarean Delivery
Types of uterine incisions
1-Classical
vertical incision into the body of uterus
Indications:
a. Lower segment cannot be exposed
b. transverse lie
c. placenta previa, anteriorly located
d. Lower segment not formed
2. Low Segment Transverse
easier to repair
located at a site least likely to rupture in a subsequent pregnancy
Does not promote adherence of bowel or omentum to the incisional line
Abdominal operations: Cesarean Delivery
Abdominal Operations: Postpartum Hysterectomy
IndicationsIntrauterine infection
Grossly defective scar
Markedly hypotonic uterus
Laceration of major vessels
Large myomas
Severe cervical dysplasia
Carcinoma in situ
Placenta previa, accreta
Abdominal Operations: Postpartum Hysterectomy
Major deterrents to CS-hysterectomy:
Increased blood loss
Urinary tract damage
Abdominal Operations: Postpartum Hysterectomy
Morbidity is increased if CS-hys is done
on an emergency basis.
Abdominal Operations: Postpartum Hysterectomy
Techniques1-Total Hysterectomy
more extensive mobilization of the bladder medially and laterally is necessary
2. Supracervical Hysterectomyamputate the body of the uterus above the level of the cervix
Version
Presentation of the fetus is altered artificially
Substitute one pole of a longitudinal presentation for the other
Convert oblique or transverse into a longitudinal presentation
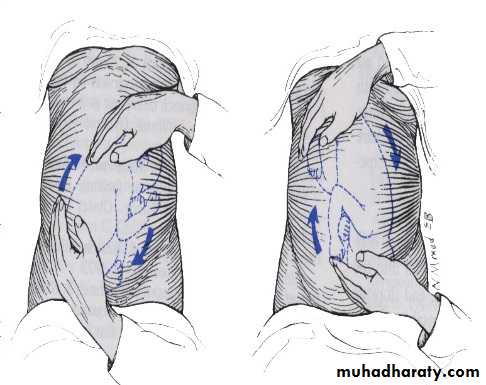
External Version
Manipulations are performed
exclusively through the abdominal
wall.
External Version
External Cephalic Version
IndicationsBreech presentation
Shoulder presentation
There should be NO marked CPD nor placenta previa
Risks
Maternal mortalityPlacental abruption
Uterine rupture
Fetomaternal hemorrhage
Preterm labor
External Cephalic Version
Prerequisites
Presenting part has not descended into the pelvis
There is normal amount of amniotic fluid
Fetal back not posterior
Woman not obese
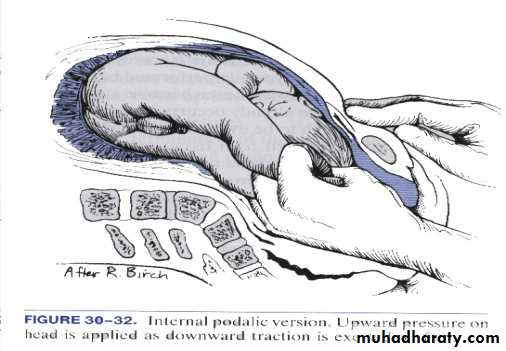
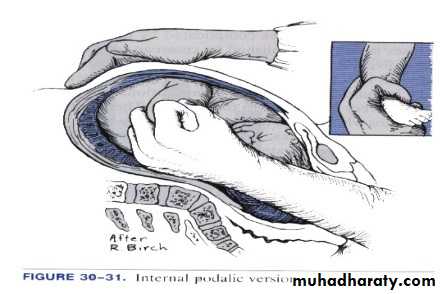
Internal Podalic Version
Entire hand is introduced into the
uterine cavity.
Internal Podalic Version
Indication
delivery of a second twin