4rd stage Lec.1
Introduction Even healthy person has more than (1014) microbial cells reside different site of his body (skin, mouth, intestines…), that means 100-fold more than number of cells that make up the human body.
Most of these microbial cells (e-g : bacteria ) do not produce disease but achieve a balance with the host that ensure the survival, growth and propagation of both the bacteria and the host still many species of microorganisms (fungi, bacteria, viruses and parasites ) are pathogenic (have the ability to cause disease ).
Advances in microbiology especially in diagnosis, prevention and cure of infection have made key contribution to improve human health & life.
However, infection is far from defeated. In poor countries an estimated (10 million) young children die each year from infections diarrhea, measles, malaria, tetanus, diphtheria and whooping cough. Even in wealthy nations infections is still common at least a quarter of all illnesses for which patients consult their doctors in U.K. are infective, and around 1/10 patients acquire infection while in hospital, sometimes with multiresistant organisms.
An Outline History of Microbiology and Infection:
Ideas of infections & epidemics were recorded by Hippocrates B.C., but it was more than 2000 years before the early microscopists began to make observations on living creatures too small to be seen by the naked eye.
Before the formal establishment of Microbiology in the second half of the19th century, Edward Jenner (1749- 1823) established the concept of immunization by using cowpox inoculation showing that it was effective & safe for preventing smallpox.
Louis Pasteur (1822-1895) used the principle of attenuation (render microbes to be less virulent) to develop a successful vaccine against Anthrax for use in animals.
The British surgeon Joseph Lister (1827-1912) established antisepsis, aimed at destroying the microorganisms responsible for infection during surgery.
Robert Koch (1843-1910) established the principles & techniques required to isolate and propagate pure cultures of specific bacteria.
These principles, often referred to as Koch's Postulates, they are:-
1 - The organism is demonstrable in every case of the disease.
2 - It can be isolated and propagated in pure culture in vitro.3 - Inoculation of the pure culture by a suitable route into a suitable
host should reproduce the disease.4 - The organism can be re-isolated from the host.
In the century following Pasteur & Koch's work, the list of specific human pathogens has extended to include several hundred organisms. Fungal & protozoan pathogens were recognized.Technological breakthrough, including tissue culture and electron microscopy, were required to enable recognition of viruses.
Later, many further advances in technology provided more precise understanding of the nature and function of microbes, especially after the revolution in molecular biology that followed the elucidation of the DNA structure by Watson & Crick 1953.
Glossary:
Pathogen: A microorganism capable (has the ability) of causing disease.Non-pathogen: A microorganism that does not cause disease. May be part of the normal flora.
Pathogenicity: The ability of an infectious agent to cause disease.
Opportunistic pathogen: An agent capable of causing disease only When the host's resistance is impaired.Infection: Multiplication of an infectious agent within the body. multiplication of normal flora is generally not considered an infection.
Adherence: (adhesion, attachment): The process by which bacteria Stick to the surface of host cell. Once bacteria have Entered the body, adherence is a major initial step in The infection process.
Invasion: The process whereby bacteria & other microorganisms Enter host cells or tissues and spread in the body.
Toxigenicity: The ability of a micro-organism to produce a toxin that Contribute to the development of disease.
Virulence: The quantitative ability of an agent to cause disease.
Virulent agents cause disease when introduced into the host in small numbers.Carrier: A person or animal with asymptomatic infection that can be transmitted to another person or animal
4rd stage- Lec.2
"Bacterial Growth"
Most of what we know about bacteria derives from their growth.
Bacteria growth involves both an increase in the size of organisms and an increase in their number.The net effect is an increase in the total mass (biomass) of the culture.
When placed in a suitable environment and conditions (nutrient temperature) a bacterial cell begins to grow; when it has made about twice the amounts of component materials that it started with, it divides.
Growth is a central technique in bacteriology as it is used for:-
1) Detection and identification of bacteria.2) The assessment of antibiotic effects.
3) Produce the desirable products in biotechnology industries.
Types of growth:-
In the laboratory, bacterial growth can be seen in three main forms:-1- By the development of colonies, the macroscopic product of 20-30 cell divisions of a single cell.
2- By the transformation of a clear broth medium to a turbid suspension of 107- 109cell/ ml.
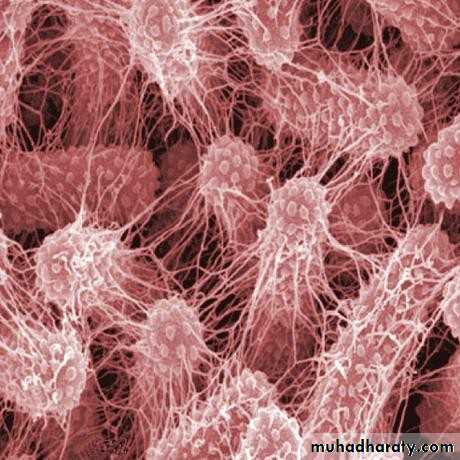
3- In biofilm formation, in which growth spread thinly (300-400µm) over the surface of the broth.
The Growth Curve: (Growth Phases in broth culture).
The Growth phase of pure culture of a single organism can be placed in 4 main phases, and those are:-
1- The lag phase:
Represents a period during which the number of cells in the broth culture appears to remain constant as cells are thought to be preparing for growth in the new environment, by forming and accumulating enzymes and intermediates to concentrations that permit growth to resume.
2- The exponential Stage:
During this phase, increase in cell number becomes detectable, its rates accelerates rapidly showing a linear increase in log cell number with time. This log- linear relationship is constant for a given bacterial strain under certain conditions & is referred to as "Doubling time" for that organism; it is between 13min for Vibrio cholerae and 24h for Mycobacterium tuberculosis. On this basis cholera is a disease that can kill within 12hr, whereas tuberculosis takes months to develop.Detection of the organism by culture takes one day for V. cholerae whereas several weeks are required for M. tuberculosis.
The biomass increase in an exponential manner until one of two happens:-
1) Nutrients in the medium become exhausted.2) Toxic metabolic products accumulate and inhibit growth.
3- Stationary phase:Exponential growth cannot be sustained in a close system with limited nutrients. Eventually growth slows down and the total bacterial cell number reaches a maximum and stabilizes, this known as stationary phase in which there is a slow loss of cells through death, balanced the formation of new cells through growth and division, the count stays constant.
4- Decline phase:
After a period of time in the stationary phase, the death rate increases until it reaches a steady level. After the majority of cells have died, the death rate decreases, so that a small number of survivors may persist for months as a few cells growing at the expense of nutrients released from cells that die & lyse.
Growth on agar plate
Unlike growth in broth, less is known about growth on solid media, which results macroscopic colonies. Each colony represents a wide range of environments, from an abundance of O2 and nutrients at the edge, to almost no O2 or nutrients available to cells in the center. It is likely that all phases of growth are represented in the colonies, depending on the location of the cell and the age of the culture; thus cells at different locations can show different phenotypes; still, in practice, colonies can be used reliably to inoculate routine tests of antimicrobial susceptibility in clinical labs.Measurement of Cell Mass:
It involved both direct and indirect methods:
1- Direct physical measurement:Measurement of dry weight, wet weight and volume of cells after centrifugation, used with very dense cultures for research and industrial purposes.
2- Direct chemical measurement:
It measures some chemical components of the cell, such as total nitrogen, total protein and total DNA.3- Indirect measurement of chemical activity:
Such as rate of O2 production or consumption, CO2 production and consumption.4- Turbidity measurement
Determines the amount of light scattered by a suspension of cells using spectrophotometer with calibration of a standard curve.
Bacteria scatter light in proportion to their numbers. Turbidity or Optical density of the cell suspension is directly related to cell mass or number. This method is sensitive to about 107 cell/ml
Media for Bacterial Growth:
In order to study the properties of a given organism, it is necessary to cultivate it in pure culture on suitable growth media contain all the nutrients required by the organism, and these are:
1- A source of protein (Nitrogen source) derived from casein or infusion of brain, heart or liver.
2- Carbon source.
3- Minerals (Sulfur and phosphorus).4- Growth factors e.g.: amino acids, vitamins.
5- Control of PH in the final product (after sterilization). There are two main types of media Liquid & Solid.Liquid media are of limited use in identification of bacterial species because:-
1- Growth usually does not exhibit characteristic appearance.
2-Organism cannot be separated from mixed growth in liquid media. Solid media are useful in identification and isolation of pure culture for different bacteria.
Gelatin was used by the early bacteriologists to make the first solid media, now agar is used for gelling media, It is an acidic polysaccharide extracted from certain red algae. Agar is uniquely suitable for microbial cultivation because it is resistant to microbial action.
Culture media are of many kinds according to their ingredients such as:-
1- Basal media: (Simple media) as Nutrient broth, peptone water, it is the basis of most media.
2- Enriched media: (Blood agar) with nutritional requirements.
3- Selective media: (Gentamicin blood agar) contain substances that inhibit all but a few types of bacteria.4- Indicator media: (MacConkey agar) incorporate substance that is changing visibly as a result of the metabolic activity of organisms.
5- Transport media: Maintain the viability of a pathogen and avoid over growth of other contaminations during transit from the patient to the lab
4rd stage Lec.3
Staining:
Bacteria in nature are colorless, and are difficult to be recognized and studied by the light microscope, unless they are stained.Stains react chemically with cellular material, and enhance the contrast between the cell and the background.
A stain is a dye consists of:-
1- A colored ion (chromophore), either (+ve) or (-ve) charged.
2- A counter ion to balance the final charge. Bacteria carry a net (-ve) charge at PH: 7, therefore:
a) Positive dye (cation) such as: Methylene blue, crystal violet & basic
fuchsine, are useful for direct staining of cells.
b) Negative dye (anion) such as: Eosin & nigrosin will not directly stain bacterial cells, but they stain the background leaving the cells clear and bright.
There are two main types of staining:
I) Simple staining:It means that one dye and a one step procedure are used to stain microbial cells, to reveal a microbial morphology feature like: size, shape and arrangements of cells.
The most common dyes used in simple staining are cationic (or basic)
dyes, such as: Crystal violet, Methylene blue and basic fuchsine.
Staining of microbes requires a suitable smear spread in a thin film over a small area of a microscopic slide, then fixed by heating to make the cells adhere to the slide.
A good smear preparation should:
1- Be of an appropriate thickness to view individual cells.
2- Withstand repeated washing during staining.
3- The cell will retain the original morphology after fixation and staining.
II) Differential Staining:-Using stains that react differently with different cell types, thus these stains are important in identification of bacteria; this staining ,mostly requires more than one dye and more than one step.
1- Gram stain:
It is the most commonly used stain; it divides bacteria into two large groups:a) Gram- positive bacteria (blue-purple in color)
b) Gram- negative bacteria (pink in color)The different responses and coloring of bacteria is based on
fundamental differences in cell structure and composition of cell wall. Staining with Gram stain is of four steps:-1- Application of a primary stain (crystal violet).
2- Adding of mordent (Gram iodine) for better complex formation between a dye and its target compound.
3- Decolorization by an organic solvent (acetone- alcohol) to remove the primary stain from the cell.
4- Adding a counter stain (safranin) to recolor cells that have lost primary stain after Decolorization; it should contrast in color with the primary stain.
The cell wall of a Gram +ve bacterium is composed of a heteropolymer of protein and sugar (peptidoglycan) called murein
(25nm thickness). This murein provides a barrier through which the crystal violet- iodine complex cannot pass during Decolorization, and the cell appears purple in color after the staining procedure.
A Gram -ve bacterium contains less murein and more lipid than a Gram
+ve one; this allows a rapid and effective removal of the dye- complex during Decolorization. The Gram –ve cells appear pink after staining with counter stain safranin.
2- Acid- Fast Stain:
In a manner quite similar to the Gram- stain, the acid- fast stain differentiates an important group of bacteria, the Mycobacteria, on the basis of lipid content (mycolic acid) at the surface of the cell, giving it waxy properties. Once these cells are stained by using heat to allow the stain to penetrate, they resist Decolorization with acid- alcohol, hence the name acid- fast.3- Bacterial Endo spore stain:
Bacterial Endospores present special problems for food industry, because of their resistance to high temperatures used to sterilize products.Endospores form inside vegetative cells in genera like Bacillus and Clostridium; they do not stain readily and require a heating step to drive the dye (e.g. Methylene blue or crystal violet) into the spore body. Once stained. Spores retain the dye. Whereas washing with water removes
the stain from vegetative cells.
4-Negative staining- Capsule stain:
It is the staining of everything in the back ground but not the cells .a themselves. It is useful to demonstrate the mucoid capsule that surrounds the cells of many bacterial spp. The presence of a
capsule is a major factor in determining the Pathogenicity of a
bacterium.
A suspension of cells is mixed with a drop of India ink on a glass .b
slide and spread thinly for viewing with phase contrast optics. The unstained capsule is visible against a grey background with the cell appears as a darker area in the center of the capsule.
5- Flagella stain:
Many bacterial spp. Are motile, most by means of flagella. Their positions are of taxonomic significance. It is critical to use young actively culture (exponential phase). Staining flagella usually requires several attempts before success.4rd stage Lec.4
Normal Flora in Human
Normal flora means: - The population of microbes that inhibit regularly the skin and mucous membranes of healthy normal person and do not interfere with normal body functions (commensals).
The majority of N.F. is bacteria. Viruses, fungi and protozoa are also found in healthy person, but form only minority of the total population of N.F. Most investigators do not consider viruses and
parasites members of N.F., because they are not commensals and do not aid the host.
Why must we know N.F.?
Knowledge of N.F. of the human body is important in diagnostic Microbiology, especially for determining the clinical importance of microorganisms that are isolated from patient specimens.
Normal flora frequently are found in clinical specimens as a result of contamination during collection or because the colonizing organism is involved in the infection.
The normal flora is acquired rapidly during and shortly after birth. The new born human is exposed to microbes from the mother and the environment, skin is colonized first, followed by the oropharynx, gastrointestinal tract and other mucosal surfaces.
Factors influence normal flora:
The normal flora in and on the human body is determined by many factors such as: Age, diet, environment (PH, temperature, O2, moisture..), hormonal state, health, personal hygiene.Normal flora can be arranged into two groups:
1- The resident: relatively fixed types of microbes regularly found in a given area at a given age.2- The transient: Non- pathogenic or potentially pathogenic microbes from the environment that inhibit the skin or mucous membrane for hours, days or weeks.
If the resident flora is disturbed, transient microbes may colonize, proliferate and produce disease.
Significance of the Normal flora to the host:
Normal flora influences the well- being of the host and plays a critical role in his health as it:1- Provides essential growth factors and vitamins e.g. vit. K.
2- Aids absorption of nutrients in gastrointestinal tract.3- Prevents colonization of pathogens and protects against infections with highly virulent microbes.
4- Stimulate the immune responses of the host.
Infection of the host by normal flora:
-Normal flora may act as opportunistic pathogens, especially in host with impaired immunity and may produce disease under certain circumstances. For example:- Flora of gingival crevice causes dental caries in 80% of the population.
- Bacteria Streptococcus viridans (N.F of the upper respiratory tract), if they are introduced into blood stream in large numbers (after tooth extraction or tonsillectomy), they may produce infective endocarditis.- Bacteria Escherichia coli are part of normal flora of the large intestine and are harmless in that location, if introduced into urinary tract, they cause painful urinary tract infection (UTI).
Normal flora of different parts of the human body:
Skin:Acinetobacter, Bacillus, Staphylococcus, Streptococcus, Corynebacterium, Candida.
Upper Respiratory Tract:Acinetobacter, Actinomyces, Corynebacterium, Haemophilus, Moraxella, Neisseria, Staphylococcus, Streptococcus, Candida, Entamoeba.
Gastrointestinal tract:
Bacteroides, Campylobacter, Clostridium, Enterobacteriaceae, Helicobacter, Staphylococcus, Streptococcus, Lactobacillus, Pseudomonas, Propionibacterium, Candida, Entamoeba, Trichomonas.
Genitourinary System:
Bacteroides, Clostridium, Corynebacterium, Enterobacteriaceae, Gardnerella, Haemophilus, Lactobacillus, Mycoplasma, Staphylococcus,Streptococcus, Treponema.
Bacterial Pathogenicity
Pathogenicity: Ability to cause disease.Virulence: Degree of Pathogenicity.
Many properties that determine a virulence are unclear or unknown, but when a microbe overpowers the host defenses, disease results.Types of bacterial pathogen:
Bacterial pathogens can be classified into two broad groups:
1- Opportunistic pathogens:These cause disease only when the host defenses are impaired or compromised (e.g.: acquired disease, immunosuppressive therapy,
These pathogens are part of the normal flora, and when they
introduced into anatomic sites, where they are not normally found, they may develop disease.
2- Primary pathogens:-
These pathogens are capable of causing disease in individuals with intact immunological defenses, as they cause disease in individuals with impaired defenses.Virulence Factors:
The possession of virulence factors differentiates pathogens from non- pathogens, and their number and potency separate opportunist from primary pathogens.ID50:- Infectious dose required to cause disease in 50% of inoculated test animals.
LD50:- Lethal dose of microbial toxin that will kill 50% of experimentally inoculated test animals.e.g.:- ID50 for Vibrio cholera is 108cells.
ID50 for Bacillus anthracis is 5000-10000 spores. Virulence factors help bacteria to:
1) Invade the host2) Cause disease
3) Evade host defenses
Some of the virulence factors in bacteria:Bacteria have many types of virulence factors that provide microbes with the capacity to avoid host defenses and damage host cells, tissues and organs, such as:-
1) Adherence factors:-
Many pathogens colonize mucosal sites by using Pili (fimbriae) to adhere to cells. Fimbriae are numerous thin, rigid and rod- likestructures present on the surface of G –ve and some G+ve bacteria, they are much thinner than flagella and involved in attachment of some bacteria to the host cell surfaces. Their antigenic composition is complex. They consist of aggregates of a structural protein subunit called Fimbrillin (Pilin). Fimbriae are found in many bacteria like: E. coli, Pseudomonas, Neisseria, and Vibrio.
2) Invasive Factors: Surface components that allow the bacteria to invade host cells, these factors can be encoded to plasmid, but often are on chromosome.
3) Capsule:
Many bacteria are surrounded by capsules that protect them from opsonization and phagocytosis.Most capsules are polysaccharides composed of Sugar monomers that vary among different bacteria. Capsule reduces the efficiency of phagocytosis and prevents efficient opsonization of bacterium by complement or specific antibody. All pathogens associated with Meningitis & Pneumonia have capsules, such as: H influenzae, N. meningitidis and Strep. pneumoniae.
4- Enzymes:-
Many pathogens secrete enzymes that contribute to their Pathogenicity:A) Leukocidins: Prevent phagocytosis by killing WBC
B) Hemolysins: Cause the lysis of RBCs (Streptococci).C) Coagulase: Cause blood to coagulate to protect bacteria from phagocytosis and other host defenses.
D) Kinase:
Enzymes that dissolve blood clots which the host form to isolate the pathogen and helps them escape from host defenses.
E)Collagenase: Break down collagen found in many connective tissues e.g.: Clostridium perfringens causes Gas- gangrene, uses this enzyme to spread through muscle tissues.
F) Hyluronidase:
Enzymes that hydrolyze hyluronic acid which is a constituent of the ground substance of connective tissue, and aid bacterial spread through tissue e.g.: Staphylococci, Streptococci.G) Streptokinase: (Fibrinolysin)
An enzyme produced by hemolytic Strep. It activates a proteolytic enzyme of plasma and aid the spread of Strep. Through tissues.Streptokinase is used in treatment of acute myocardial infarction to dissolve fibrin clots.
H) Proteases:
Enzyme hydrolyze immunoglobulin and allow pathogens (e.g.: N. meningitidis, Strep. pneumoniae) to inactivate the primary antibodies found on mucosal surfaces and eliminate protection of the host by antibodies.4rd stage Lec.5
Bacterial Toxins:
Toxins are biochemically active substances that are released by
microorganisms and have a particular effect on host cells. Microorganisms use toxins to help them establish infections and multiply within the host. 40% of the toxins cause disease by damaging the cell wall.
Toxins also can cause human disease in the absence of the pathogens that produce them, and this is the common mechanism of Food poisoning that involve the ingestion of pre- formed bacterial toxins, it is referred to as Intoxication, e.g.: Botulism.
Bacterial toxins are generally classified into two groups:
1- Exotoxins2- Endotoxins
Exotoxins:-Exotoxins produced mostly inside some G+ve bacteria and less
G-ve bacteria, as part of their growth and metabolism, and released into the surrounding media.They are proteins in nature and many are enzymes.
They are soluble in body fluids, so can easily diffuse into the blood and are rapidly transport throughout the body.Exotoxins cause damage to the host cell by:-
1- Destroying particular parts of the host cells.
2- Inhibiting certain metabolism functions.
They cause Extreme pyrogenic response (fever). Exotoxins are of 3 major categories:-1- Cytotoxins:-
Kill host cells by affect their function e.g.: Corynebacterium diphtheriae
2- Neurotoxins:-Target the nervous system and can interfere with normal nerve impulse transmission. e.g.: Clostridium tetani, Clost. botulinum.
3- Enterotoxins:-
Affect cells lining the gastrointestinal tract e.g.: Vibrio choleraeExotoxins are among the most lethal substances known; only 1mg of the botulinum exotoxin is enough to kill 1 million guinea pigs.
Exotoxin is inactivated by heat and no longer cause disease, but stimulates the body to produce antitoxin (antibodies), that provide immunity to exotoxins.
Toxoid:-
Is altered exotoxin injected to stimulate the production of antitoxins and provide immunity (by formaldehyde). Inactivation of toxins without altering antigenicity results in successful vaccine, e.g.: diphtheria and tetanus toxoids.
Some medically Important Exotoxins:-
Bacteria Exotoxin Tissue damage Action Disease
Clost. tetani Tetanospasmin Neurons Spastic paralysis TetanusClost. perfringens α- toxin RBCs, WBCs Cell lysis Gas gangrene
Endothelium
Clost. botulinum Neurotoxin nerve muscle Flaccid paralysis BotulismJunction
Coryn. Diphtheriae Diphtheria throat, heart, Inhibition protein DiphtheriaToxin peripheral nerve synthesis
Vibrio cholerae Enterotoxin Intestinal epi- fluid loss from Cholera
Thelium intestinal cells
Staph. aureus α- toxin RBCs & WBCs Hemolysis Abscesses Hemolysin RBCs & WBCs Hemolysis Abscesses Enterotoxin intestinal cells induce vomiting food- poisoning& diarrhea
TSST-1
Release cytotoxin Toxic Shock S.Strep. pyogenes Streptolysin RBCs &WBCs Hemolysis Hemolysis, py- O & S ogenic lesions
Bacillus anthracis Cytotoxin lung Pulmonary Anthrax
Edema
Aspergillus fumigus Afla toxin Liver carcinogenic liver damage, cancerEndotoxins:-
They are complex lipopolysacchrides in the outer envelope of the cell wall of G-ve bacteria. The outer envelope of these bacteria consists of lipoprotein, phospholipids and lipopolysacchrides (LPs).
Lipoprotein of (LPs) called (Lipid A) is the endotoxin.
The endotoxin liberates when G-ve bacteria die and the cell wall lysed. The substance is heat stable. Administration of endotoxin to animal or human results in a series of events:
Fever, leucopenia, hypoglycemia, hypotension, shock, impaired perfusion of essential organs ( brain, heart, Kidney), intravascular coagulation and death.
e.g.:- Salmonella typhi, Proteus spp. Neisseria meningitidis.
Characteristics of exotoxins & endotoxins:Exotoxin Endotoxin
1- Excreted by living cell Released on bacterial death2- Produced by both G+ve & Found only in G-ve bacteria
G-ve bacteria3- Unstable, toxicity often destr- Stable, withstand heating at oyed by heating at above 60oc above 60oc for hours.
4- Highly antigenic, stimulate weakly immunogenic formation of antitoxin.
5- Converted to antigenic, non- not converted to toxoids
Toxic toxoids by formalin, heat
6- Highly toxic, fatal to animals in moderately toxic, fatal in tens
µg or less. Or hundreds of micrograms
7- Usually bind to specific receptors Specific receptors not found on cells. on cells.
8- Usually do not produce fever in usually produce fever in host
Host. By release of interleukin-19- Frequently controlled by extra- Synthesis directed by chrom- Chromosomal genes (plasmid) osomal genes.
"The infection process"
I) Entry into the Human Body:
Bacteria must first gain entry into the body to establish an infection. The mouth, nose, respiratory tract, ears, eyes, urogenital tract and anus, are sites through which bacteria can enter the body. Natural defense mechanisms and barriers, such as: skin,mucus, ciliated epithelium and antibacterial secretions (e.g. lysozyme), make it difficult for bacteria to gain entry into the body.
These barriers are sometimes broken ( e.g.: a tear in the skin, a tumor or ulcer) providing a portal of entry for the bacteria, or the bacteria may compromise the barriers and invade the body.
Sites of Entry:
A . Skin: Skin has a thick, horny layer of dead cells that protects the body from infection by many means such as:
1- Inactivate microorganisms by fatty acids (skin PH is about 5.5).
2- Substances secreted by sebaceous and other glands.3- Certain peptides formed locally by keratinocytes.
4- Materials produced by the Normal flora of the skin.Cuts in the skin provide a means for bacteria to gain access to the tissue underneath, or may enter hair follicles or sebaceous glands to cause styes & boils.
Fungi (the dermatophytes) infect the non-living keratinous structures (hair, nails) and if the parasites rate of growth into keratin exceeds the rate of shedding of keratinous product, the infection may become chronic.
B. The conjunctiva:
It’s a specialized area of skin, kept clean by tears aided every few seconds by the wiper action of the eyelids contaminated fingers, flies or towel carry infection to the eye. Antimicrobial substances in tears (Lysozyme) and certain peptides have a defensive role.C. Respiratory tract:
In the upper & lower R-T, inhaled micro org., like other particles (dust, smoke) will be entrapped in mucus, carried to the back of throat by ciliary action, and swallowed; some micro org. have developed specific mechanisms to avoid this fate. e-g: inhibiting ciliary activity or avoiding destruction by alveolar macrophages (Tubercle bacilli).D. Gastrointestinal tract:
The acid, bile & the general flow of intestinal contents, are the natural defenses in gastrointestinal tract, however, many bacteria are unaffected or have means to evade these defenses e-g: the outer membrane of G-ve bacteria makes them more resistant to acid and bile.
E- Urinogenital tract:
Urinogenital tract is a continuum, so micro organisms can spread easily from one part to another. It has natural defenses, e-g:1) Certain lactobacilli colonize vagina & produce lactic acid (vaginal PH=5) which inhibit other micro org.
2) The protective layer of mucus in bladder & the production of antibodies & immune cells.
II) Attachment and Colonization:
Bacteria use specific mechanism to adhere to and colonize different body surfaces. If the bacteria can adhere to epithelial or endothelial cell linings of bladder, intestine and blood vessels, they cannot be washed away, and this adherence allows them to colonize the tissue.
Escherichia coli and other bacteria have adhesins that bind to specific receptors on the tissue surface and keep the organisms from being washed away. Many of these adhesion proteins are present at the tips of fimbriae (pili) and bind tightly to specific sugars on the target tissue.
A special bacterial adaptation that facilitates colonization is a biofilm produce by bacteria; Bacteria in biofilm are bound within a sticky web of polysaccharide that binds the cells together and to the surface (e.g.: Dental plaque). The biofilm matrix can also protect bacteria from host defenses and antibiotics.
III) Invasion:
Once surface attachment has been secured, microbial invasion into subsurface tissues and organs (infection) is accomplished by the direct action of an organism's virulence factors. Some microorganisms produce factors that force mucosal surface phagocytes (M cells) to ingest them and then release them unharmed into the tissue below the mucosal surface.
Other organisms such as Staphylococci an t proteins and nucleic acids that destroy host cells and tissues, (e.g. d Streptococci, produce an array of enzymes that hydrolyzed hosHyluronidase, nuclease, Collagenase.).
Some pathogens cause disease from their site of attachment without further penetration, e.g.: Diphtheria and whooping cough, the bacteria produce toxic substances that destroy surrounding tissues but the organisms themselves do not penetrate the mucosal surface they inhabit.
Microbial Strategies for Surviving the Immune System:
Pathogen multiplies and invades quickly that damage to host is complete before immune response can fully activated, or organism's virulence is so great that the immune response is insufficient. Pathogen invades and destroys cells involved in immune response.
Pathogen survives unrecognized in host cells and avoids detection by immune system.
Pathogen produces enzymes (proteases) that directly destroy or inactivate antibodies.
4rd stage Lec.6
Some Medically Important Bacteria
Staphylococcus: Cluster- Forming Gram +ve cocci:
Staphyle: Greek word means a bunch of grapes.Staphylococci belong to family: Micrococcaceae which also includes:
Micrococcus and Stomatococcus.Staphylococci are non- motile, non-spore forming, occasionally capsulated; catalase +ve, oxidase –ve whereas Micrococci are usually oxidase +ve.
All Staphylococci produce catalase whereas Streptococci don't.
Staphylococci ferment glucose, facultatively anaerobic, Micrococci are obligate aerobes.The most important human pathogen, Staph. aureus contains protein A
an antiphagocytic virulence factor in its cell wall.Most strains also contain clumping factor (bound Coagulase) on their outer surface, which binds to fibrinogen, thus causing the organisms to aggregate in plasma. Another (free) Coagulase causes clotting of plasma in a tube test, and distinguishes this species
Staph. aureus is Coagulase +ve.
There are nearly 30 defined spp. and sub spp. of Staphylococci. Staphylococci are wide spread in nature, their habitats are skin andmucous membranes of mammals and birds, most important is Staph. aureus which can cause both superficial and deep pyogenic infections as well as toxin-mediated illnesses.
Coagulase –ve Staph. saprophyticus is an important urinary tract infectious agent in women.
Species of Staphylococci found on human skin include:-
Staph. epidermidis (albus), Staph. haemolyticus, Staph hominis, Staph. capitis, Staph xylosus and others.All of these are opportunistic pathogens especially in patients with intravascular catheters or implanted prosthetic devices.
Stomatococcus mucilaginosus is associated with an aggressive endocarditis and bacteriaemias in immunosuppressed patients.
Staphylococcus aureus:
Morphology and culture characters:Staph. aureus is about 1µm in diameter, arranged in clusters. On blood agar and nutrient agar (o/n at 37Oc), it forms colonies 1-3 mm, they are smooth, low convex, opaque, sometimes surrounded by a narrow zone of haemolysis on blood agar,
Older colonies become translucent and sticky, some strains are capsulated, and their colonies are large and slimy.
Pigmentation:-
Ranges from cream to gold. Pigmentation enhanced on fatty media, prolonged incubation and by leaving plates at room temp.Non- pigmented strains are not uncommon; grown anaerobically;
colonies are often smaller and grayish in color.S. aureus tolerate conc. Of NaCl that inhibit most other bacteria.
Enzymes & toxins:S. aureus produces many enzymes & toxins, some of which are virulence factors such as Protein A, Capsule (some strains) & Peptidoglycan.
Enzymes include bound & free Coagulase, Nucleases, Proteinase, Phosphatase & Fibrinolysin.
Toxins include Enterotoxins A-E, toxic shock syndrome toxin (TSST-1), epidermolytic toxins A&B, Hemolysin α, β, Y and Leukocidins.
Coagulase test Catalase test
S. aureus infections:* Folliculitis: result from infection of the hair follicles by S.aureus.
* Furuncles: infection leads to the formation of a collection of pus caused by Coagulase: It is an enzyme that clots plasma and serves to wall off the infected site and impedes ingestion by phagocytic cells*Carbuncles: infection may spread from a furuncle to the subcutaneous tissues. They are serious lesions that may result in blood stream invasion (Bacteremia).
* Impetigo: A highly communicable superficial skin infection characterized by large blisters, containing many staphylococci in the superficial layers of the skin.
* Cellulitis (skin & soft tissues):A diffused inflammation or submucosal tissue .
* Osteomyelitis: The bacteria reach the bone via hematogenous dissemination from a distant infection site.* Broncho pneumonia (especially post-influenza): a complication of viral influenza associated with the formation of lung abscess.
* Toxic shock syndrome (TSS): In human it is associated with a sudden onset of high fever, vomiting, diarrhea, muscles pain and rush. It may progress to sever shock with evidence of renal failure.
* Staphylococcal scalded skin syndrome: It usually occurs in young children due to exfoliatin toxin production at a local site of infection (usually the nose) which causes epithelial desquamation at remote sites of the body.
* Staphylococcal food-poisoning: S.aureus produces soluble Enterotoxins when grows in carbohydrate and protein foods. The toxin acts on neural receptors in the upper GIT leading to stimulation of the vomiting center in the brain. Within 4-6 hrs following ingestion of these preformed toxins, the patient exhibit symptoms of: Diarrhea, abdominal cramps, acute vomiting, no fever and the recovery is rapid.
Biochemical characters:
S. aureus ferments a range of sugars, including Mannitol. Coagulase + ve, Voges-Proskauer (acetion production) + ve Gelatinase + ve, alkaline phosphatase + ve. Indole – veUrease±�
Resistance to physical & chemical agents:
S. aureus is among the hardiest of the non-sporing bact.
To antibiotics:It withstands moist & heat at 60oc for 30 min.
It is readily killed by phenolic & hypochlorite disinfectants.
Sensitivity
Most clinical isolates of S. aureus are resistant to benzyl-penicillin, due to the production of a beta-lactamase that binds to the antibiotic and destroys it activity by opening it at the beta-lactam ring.Some S. aureus strains are resistant to the beta-lactamase resistant
penicillins (Methicillin, cloxacillin, flucloxacillin….)These strains are called Methicillin-resistant S. aureus (MRSA) they spread world-wide and caused major therapeutic problems.
The Methicillin resistance implies resistance to all beta-lactam antibiotics, including the cephalosporins.
S. aureus strain are sensitive to the glycopeptides Vancomycin which used in treatment of serious MRSA infections.
Diagnosis:
S. aureus is hardy and easy to recover from swabs, pus, tissues and blood cultures.
It grows readily on blood, chocolate and nutrient agar at 37oc for 18-
24hr. Gram stain slid & catalase test (+ve) must be done, also Coagulase test (slide or tube method) and finally antibiotic tests appropriate to the clinical situation.
Isolates or food samples examined by latex agglutination test for
Enterotoxins.Coagulase-Negative Staphylococci:-
They all from clusters and colonies smaller but similar to those of S. aureus and are grey or white in color.These staphylococci are potential pathogens and some of them possess virulence factors similar to those S. aureus.
S. saprophyticus is an important cause of urinary-tract infection; other species cause opportunistic infections such as endocarditis of prosthetic heart valves.
Hospital-acquired infections are due mostly to S. epidermidis carried by staff and patients in cardiac, orthopedic or neonatal intensive care units and present problems both of diagnosis and management.
4rd stage Lec.7
Streptococcus and Enterococcus:
- G+ve spherical bacteria form pairs or chain.- Old cultures lose their Gram positivity and appear to be G-ve.
- Facultative anaerobes, non spore forming bacteria.
- Form small colonies on agar media mostly with hemolytic effect on blood agar.- Catalase –ve (this helps to distinguish them from Staphylococci).
- Need enriched media to grow (e.g.: blood agar).- Growth and hemolysis are aided by incubation in 10% CO2.
- They are mostly commensal in mouth and throat.- Strep. pyogenes and Strep. agalactiae are primary pathogens.
- Strep. faecalis (Enterococcus) is commensal in the intestine.- Peptostreptococcus is an obligate anaerobe.
Classification of Streptococci:
Streptococci are a heterogeneous group of bacteria and no one system suffices to classify them.
Initial classification depends on the type of haemolysis produced on blood agar media:-
1) β- haemolytic Streptococci:-Strains produce soluble Hemolysin (Streptolysin O & S) that
Form a clear zone of hemolysis around their colonies on blood agar. Strep. pyogenes (group A) is a main human pathogen.2) α- Haemolytic Streptococci:-
Strains that do not produce soluble haemolysin and cause partial clearing, often a green coloration (α- hemolysis) e.g.: Strep. Pneumonia.3- Non- haemolytic Streptococci:-
Strains that have no change around colonies on blood agar. e.g.: Strep. mutans (dental caries).A practical classification of Streptococci is based on:-
1- Colony morphology and haemolysis on blood agar.
2- Biochemical reactions.
3- Serological groups of cell- wall and capsule antigens
Classification by serology:-
Rebecca Lancefield (1933) classified different groups of β- haemolytic Streptococci into 20 serological subdivisions, depending on differences of polysaccharide antigens in the cell wall using the letters A---- H and K-, -- V.
e.g.: Strep. pyogenes (group A) Strep. agalactiae (group B)
Streptococcus Pyogenes:- (Lancefield group A)* G+ve cocci, occurring in chains, capsulated in very young cultures, non-motile and non-spore forming.
* Facultative anaerobe grows best on blood agar.
* Colonies are small, low convex, with matt (contain M protein) or glossy & mucoid surfaces (heavily capsulate).* Colonies on blood agar surrounded with clear, wide zone of hemolysis.
* Killed by 54oc in 30min. cultures should be stored at 35oc in blood broth or cooked-meat media or else freeze-dried.* Sensitive to most antiseptics, benzyl penicillin and a wide range of antimicrobial drugs.
* Catalase – ve, insoluble in bile, PYRase + ve (which distinguishes it from non-group A hemolytic streptococci).
Enzymes & toxins:
S. Pyogenes produces exoproteins that play a part in pathogenesis such as:-
1- Erythrogenic (Dick) toxin: causes the rash in scarlet fever the presence of antibodies to this toxin is detected by Dick test in which a test dose of the toxin is injected intradermally.2- Haemolysin: It is of two kinds:
a) Streptolysin O: oxygen- labile and antigenic.b) Streptolysin S: oxygen- Stable causes hemolysis around colonies on aerobic blood agar, it is not antigenic.
3- DNase: (A, B, C, &D):- DNase B is the commonest form in S. pyogenes.
4- Other enzymes: Streptokinase (Fibrinolysin), Hyluronidase, PYRase which formed only by group A strep. and enterococci.Cellular antigens:-
β- Streptococci are divided into 20 Lancefield groups by their cell wall antigen.The group A antigen is characteristic of S. pyogenes.
M-protein: group (A) streptococci is subdivided into over 60 Griffith's serotypes by differences in M protein antigen on their cell wall.
M protein impedes phagocytosis, attachment to epithelial cells.
T protein: It is a surface antigen in group (A) strains and is used as a typing marker in epidemiological studies.R protein: Different forms of this antigen present in group A serotypes but their role is unknown.
Pathogenicity:
S. pyogenes. Is the most frequent bacterial cause of Pharyngitis and Cellulitis. It adhere to pharyngeal epithelium via pili covered by M- protein , it induce two important immunologic diseases :1- Rheumatic fever
2-Acute GlomerulonephritisLab Diagnosis:
Swabs are taken from throat, nose, vagina or purulent lesion and cultured on blood agar plates, incubated: Aerobically in 5-10% CO2 (Candle Jar)
Anaerobically to improve haemolysis and group A strains that form only O- lysine fail to cause lysis on aerobic plates.
Microscopic examination of smear of pus to detect short chain of G+ve cocci.
Examine of patient's serum for Streptococcal antigens.
Haemophilus haemolyticus may be mistaken for β-haemolytic Streptococci, but their haemolysis is stronger on aerobic than anaerobic plates and it is resistant to penicillin.
Strep. pyogenes does not grow on MacConkey agar but
Strep. agalactiae does. Strep. pyogenes is more sensitive to Bacitracin than most other Streptococci, so this is used to detect Strep. pyogenes in the absence of Lancefield grouping. A disc of 0.04 units of Bacitracin is plated on a cultured plate, Strep. pyogenes should show a large inhibition zone.
For Lancefield grouping a commercial kits for Streptococcal grouping are widely used because they are convenient and liable.
Serological test (e.g.: Antistreptolysin O titer (ASOT)) are used to confirm primary infections and for diagnosis of non- suppurative sequelae of Strep. pyogenes infection, such as Rheumatic fever or Glomerulonephritis.
Streptococcus agalactiae (Lancefield group B):
It is a major Streptococcal pathogen in sites other than the upper respiratory tract. They are associated with:Septicemia & meningitis in neonates, pneumonia, endocarditis, meningitis, Cellulitis and arthritis in adults.
It is β, α or non haemolytic on blood agar.
Colonies are grey, mucoid and larger than those of other
Streptococci.
Specimens of patient should be plated on MacConkey agar. (On which most stains grow) as well as on blood agar.
Penicillin and Gentamicin disks should be placed on the Blood agar so that α and non- haemolytic strains can be Suspected from their penicillin sensitive and Gentamicin resistant reactions.
Tests for identification of group B particularly for α and non-
Haemolytic strains include:-
1- The CAMP* reaction
2- Gram stain
3- Lancefield grouping
CAMP reaction:- Detects the production of CAMP factor by group B Streptococci which enhances the action of Staph β- lysine.
4rd stage Lec.8
Non- beta haemolytic Streptococci:
They usually show α or non haemolysis on blood agar. The principle members are:-
Streptococcus pneumoniae
Viridans Streptococci: - Strep. mutans- Strep. salivarius
- Strep. milleri
Streptococcus pneumoniae:-
Pneumococci are part of the normal naso & oropharyngeal flora ofmany healthy persons (carriers), though they are involved in infection of the upper and lower respiratory tract such as:-
Bronchopneumonia, acute and chronic bronchitis, sinusitis, otitis media, meningitis, conjunctivitis, peritonitis and arthritis.
They are G+ve cocci in pairs (diplococcic) Lancet- shape or short chains, non-motile, non- sporing and all freshly isolated strains are capsulated.
Aerobic and facultatively anaerobic, grow best in 5-10% CO2 (Candle jar) on blood or chocolate agar (heated blood) which supplies nutrients bacteria need.
Colonies are small and flattened or depressed centrally (draught- sman form) with α-haemolysis zone around the colonies and that helps to identify the Pneumococci on blood agar.
The organisms tend to die in cultures in 1-2 days and undergo autolysis.
Pneumococci are Catalase –ve, Oxidase +ve, soluble in bile salt which is a valuable identifying property, produce acid but not gas from glucose, lactose, sucrose and inulin.
Killed by moist heat at 55oc in 10 minutes and readily by most
disinfectants. It should be freeze- dried for maintenance.
Highly sensitive to Optochin (ethyl hydro cuprein hydrochloride) the Optochin sensitivity test provides the simplest means of identifying Pneumococci and distinguishing them from viridans Streptococci. Most strains are highly sensitive to benzyl penicillin, amoxicillin, cephalosporin, erythromycin and cotrimoxazole.Differentiate characters of Pneumococci & Viridans Streptococci
CharacterPneumococci
Viridans Streptococci
Morphology
Ovoid or lancet shape diplococci, or short
Chains
Short or long chains or rounded cocci
Capsule
Present
Usually absent
Colonies
Flattened or draughts
-man shape
Convex
Effect on blood
agar
Narrow zone of α-
Haemolysis
Wider or narrow
Zone of α hemolysis
Optochin
Sensitive
Resistant
Bile solubility
+
-
Inulin fermentation
+
-
Virulence in mice
+
-
50
- There are 83 serotypes of Pneumococci according to the nature of their polysaccharide antigen of the capsule, which is partly secreted into the culture media in the form of specific soluble substance (SSS). The type of Pneumococci is determined by its reaction with type- specific antisera.
Quelling test:-
This test is useful for rapid identification and typing of Pneumococci. When Pneumococci (in sputum or culture) are mixed on a slide with specific antipolysacchride serum of the same type (or polyvalent antiserum which contains antibodies to more than 80 types), thecapsule swells and makes the cocci appear enlarged.
Pathogenicity:-
(fig)Pneumococci produce disease through their ability to multiply in the tissues. They produce no toxins; their virulence is a function of their capsule, which prevents phagocytosis.
The most important disease caused by Pneumococci is Pneumonia. Pneumococcal pneumonia is usually sudden, with fever, chills and sharp pleural pain, the sputum is bloody or rusty, recovery began between the fifth and tenth days of disease.
The mortality rate is as high as 30%.
Empyema:- (Pus in the pleural space)Is a significant complication and requires aspiration and drainage.
Pneumococci may reach other sites from the respiration tract such as:
- Sinuses (Sinusitis)
- Middle ear (Otitis media)
Meninges (meningitis)
Treatment:-Antimicrobial Therapy must be given early to terminate the illness and to avoid severe complications (e.g.: meningitis, endocarditis, septic arthritis).
The penicillins are the drugs of choice. Penicillin- resistant strains have appeared, they present little difficulty in pneumonia, but in meningitis, where limited amount of the drug reaches the central nervous system, they are a very serious problem.
Genus: Enterococcus (Fecal Streptococcus):-
- Formerly classified is Genus: Streptococcus (Lancefield group D).- Enterococcus faecalis and Enterococcus faecuim are the most
important clinically.- They are G+ve cocci cells often in pairs or short chains.
- Non- fastidious, non capsulated, α or non haemolytic on blood agar.- Resistant to 40% bile salts (grow on MacConkey agar).
- Resistant to Optochin, grow at 45oc, vogues- proskauer +ve.
- Some strains liquefy gelatin and produce H2S.- Normal habitat is the intestine of human & animals.
- Most infections are endogenous.- They may cause urinary tract infection (UTI), endocarditis, and septicemia after surgery.
- Drug of choice, Penicillin in combination with amino glycosides.
4rd stage Lec.9Neisseria:-
Neisseria, Moraxella: (Gram –ve cocci)The meningococci, N. meningitidis and gonococci, N. gonorrhea, are the important pathogens in genus: Neisseria.
Other Neisseria species are commonly found as commensals in the upper respiratory tract.
Neisseria meningitidis:-
- Oval G-ve diplococci with the long axes parallel.
- Seen in large numbers inside polymorph nuclear leucocytes.- Capsules are not evident, non spore forming, non motile and palliated.
- Aerobe, grow on enriched media (e.g.: blood agar, chocolate agar)under 5- 10% CO2.
- Colonies on blood agar are 1-2mm, convex, grey & translucent, after
48hs, colonies are larger with an opaque raised centre and thin transparent margins which may crenated.- Non-hemolytic, oxidase + ve utilize glucose & maltose, but not lactose or sucrose.
- Die within few days at room temp., but culture may be maintained on chocolate agar slants in screw-capped bijou bottles for several weeks, freeze-drying for long term storage.
- Killed at 55oc in 5min., readily killed by disinfectants.
Pathogenicity:-- The nasopharynx is the portal of entry of meningococci, there the organisms attach to epithelial cells with the aid of pili.
- From the nasopharynx, organisms may reach the blood stream
(meningococcemia).Meningitis:-
Is the most common complication of meningococcemia, it usually begins suddenly, with intense headache, vomiting, and stiff neck, progresses to coma within few hours.
The Meninges are acutely inflamed, with thrombosis of blood vessels and exudation of polymorph nuclear leukocytes, so that the surface of the brain is covered with thick purulent exudates.
Lab diagnosis:
Specimens may include: 1) Cerebrospinal fluid (CSF)2) Blood for culture.
3) Aspirate from skin lesions.4) Pus from an infected joint.
5) Nasopharyngeal swab from suspected carriers.- Swabs are plunged into transport media (e.g.: Stuart's media) for forwarding to the lab and all specimens must be submitted to the lab immediately.
- Plate out specimens (The centrifuged deposit in case of CSF) on both blood and chocolate agar and incubate at 37oc in 5- 10% CO2 for 24 hr.
- Examine Gram- stained smear, stain a second film with Methylene blue (in case of CSF, blood pus & aspirate) to detect the cell types.
- G –ve diplococci may be seen inside pus cells, and many are extracellular.
- Colonies of Neisseria on solid media can be identified by the oxidase test (+ve) and can be further identified by carbohydrate fermentation reactions.- Antibiotic sensitivity test must be done (Penicillin G is the drug of choice or Cefotaxime and Chloramphenicol).
- Latex agglutination test for measuring Antibiotic to meningococcal polysaccharides and agglutination with type- specific or polyvalent serum.
- If there is any doubt about the identity of the Neisseria, it should be forwarded to a reference lab for further examination.
Neisseria gonorrhea:-
Morphology and staining of N. gonorrhea are identical to these of N. meningitidis, they are G-ve, non motile diplococci, individual cocci are kidney- shape, occur in pairs, the flat sides are adjacent, palliated.– Aerobe grows on enriched media 5-10 % CO2.
– Colonies are convex glistering, elevated and mucoid, non pigmented and non hemolytic oxidase +ve.
– The main character that distinguishes the gonococcus from meningococcus is the ability to produce acid from glucose but not maltose.
Pathogenesis:-
Gonococci attack mucous membranes of the genitourinary tract, eye, rectum and throat, producing acute suppuration followed by chronic inflammation and fibrosis.In males it causes urethritis with yellow creamy pus and painful urination; in female it causes vaginitis with mucopurulent discharge.
– Gonococcal bacterium leads to skin lesions on the hands, forearms,
feet and legs and to suppurative arthritis.
– Gonococcal Opthalmia neonatorum, an infection of the eye of the newborn, is acquired during passage through an infected birth canal.
Lab. Diagnosis:-
The routine lab. Diagnosis of gonorrhoeae is as follows:-* Gram-stained smears of urethral discharge from men and urethral & cervical secretion from women are examined for Kidney- shaped G- ve intracellular diplococci with a few extracellular organisms (smear in this case reported + ve).
Approx. 95% of infected men & 60% of infected women will yield a + ve smear.
* Specimens are plated out on blood & chocolate agar and incubated under 5-10% CO2 at 37oc. To avoid overgrowth by contaminants, the culture medium should contain antimicrobial drugs (e-g: - Vancomycin, colistin, trimethoprim).* Gram-stained slide and oxidase test should be done for suspected colonies (It should be G – ve diplococci, oxidase + ve).
* Set up a rapid carbohydrate utilization test (RCUT).
* Plates are kept for 48 hr and cultures are re-examined before reported negative (- ve).* Serological test (e-g: ELISA) are not very useful because of Gonococcal heterogeneity.
Antibiotic Sensitivity:The gonococcus is usually sensitive to many antibiotics e-g: - Penicillin, Cefotaxime, Ciprofloxacin, Cotrimoxazole, Tetracycline, Erythromycin and Streptomycin.
Moraxella:
Moraxella catarrhalis (Branhamella catarrhalis) is the only important member of subgenus: Branhamella. They are G – ve diplococci kidney shaped, oxidase +ve, grow on simple media. It is N.F in R.T but has been isolated as causative agent of diseases e-g: Septic meningitis, endocarditis, otitis media and bronchitis.* Any G – ve diplococcus recovered in large numbers from the lower R.T of patient with pneumonia should be considered.
Branhamella is resistant to penicillin; it does not ferment glucose, maltose, sucrose or lactose.
* Drug of choice is Erythromycin.
4rd stage Lec.10
Gram-NegativeRods (Enterobacteriaceae)
The Enterobacteriaceae are a large, heterogeneous group of G-ve rods whose natural habitat is the intestinal tract of humans and animals.
The family includes many genera:-
Escherichia. Klebsiella. Shigella. Salmonella. Enterobacter. Serratia and Proteus.Some enteric organisms (e.g.: E.coli) are part of normal flora and incidentally cause disease, while others, the salmonellae and shigellae, are pathogenic to humans.
Escherichia coli
Classification:Family: Enterobacteriaceae
Genus: EscherichiaSpecies: Escherichia coli (E. coli)
Escherichia coli is a common inhabitant of the intestinal tract of man and warm- blooded animals. Most strains of E. coli are harmless and are a part of the normal intestinal microflora. These strains serve a useful function in the body by suppressing the growth of harmful bacteria and by synthesizing amounts of vitamins(vitK2).
Escherichia coli is G-ve, non-spore forming rod. 80% of strains are motile. Facultative anaerobe. Grows between 37-44oC, ferment lactose and grow as smooth pink colonies on MacConkey agar.
All strains of Escherichia are Indole +ve, methyl-red +ve, Voges- Proskauer –ve, Citrate –ve, Urease-ve, oxidase -ve; they do not produce H2S in Triple sugar- iron. Most strains produce gas from glucose.
Many strains are harmless. Found in raw milk, raw meat, non- chlorinated water, contaminated fruits and vegetables.
E.coli in human infections:
It is predominant in the healthy human intestine and is thus an indicator of faecal pollution in water supplies. It is able to cause frequent opportunistic infections:Peritonitis, appendix abscesses, septic wounds, Bacteraemia and occasionally meningitis in neonates.
E.coli stains are the commonest cause of infections of the lower urinary tract (UTI) and pylonephritis. An increasing number of strains are recognized as primary gastrointestinal pathogens causing diarrheal diseases.
Types of Pathogenic E.coli:-
there are 4 strains or categories that cause diarrheal illnesses or disease1) EHEC (enterohemorrhagic E. coli): Shiga toxins; bloody diarrhea, One serotype, E. coli 0157:H7 is responsible for the majority of the bloody diarrhea that occurs due to the production of Shiga toxins.
2) ETEC (enterotoxigenic E. coli): Secretory toxins; watery diarrhea with nausea, abdominal cramping, and fever.
3) EPEC (enteropathogenic E. coli): toxin similar to Shigella toxin; watery or bloody diarrhea .childhood diarrhea.
4) EIEC (enteroinvasive E. coli): invade epithelial cells; mucoid, bloody diarrhea and fever .Shigella-like dysentery with blood and mucus.
Treatment:
Gentamicin and sulpha drugs.Klebsiella:
Klebsiellae are everywhere in nature, in humans they can inhabit:-
The skin, pharynx and gastrointestinal tract as part of the normal flora. The respiratory tract, urogenital tract and sterile wounds
It is an opportunistic human pathogen. Klebsiella is responsible for a large number of nosocomial infections in hospitalized patients
. These infections include:
Respiratory infections, such as bronchitis. Urinary tract infections.
Surgical wound infections.
Bacteremia.
Biliary tract infection.
Characteristics:
Gram-negative rod-shaped bacteria with a polysaccharide capsule.
Non-spore forming. Non-motile.
Aerobic and facultatively anaerobic.
Lactose fermentors (pink colonies on MacConkey agar)
Moist and mucoid colonies texture.
Oxidase negative.
Voges-Proskauer positive
Indole negative Simmons's citrate positive
The virulence factors of Klebsiella are:
Capsular antigens (K antigens)
Pili (Fimbriae): (adherence). Siderophores
Siderophores are high-affinity, low -molecular-weight iron chelators secreted by bacteria and are capable of competitively taking up iron bound to host proteins.
Toxins:
Some strains of K. pneumoniae produce a heat-stable Enterotoxin gives rise to diarrhea. Endotoxins of Klebsiella are the lipopolysacchrides (LPS) in the outer membrane. Biofilm formation:
Klebsiella is one of the pathogens that are able to form biofilm, which is one of its virulence factors.The most important member of this genus is:
Klebsiella Pneumoniae (K. aerogenes)Epidemiology:
The most common infection caused by Klebsiella bacteria is pneumonia. Clinical symptoms are: severe, rapid onset of high fever, cough with blood jelly sputum, the infection may lead to destroying of lung tissue and causes pleural abscesses. Mortality in Klebsiella pneumonia is around 50%.
LABORATORY DIAGNOSIS:
1- Specimens: Urine, sputum, pus, infected tissue, a swab of a surgical wound.
2- Microscopy: in a Gram stained slide, Klebsiella appears as short, plump, gram- negative bacilli and has a big capsule.
3- Culture: Media are MacConkey, blood agar. Klebsiella produces mucoid colonies, and lactose fermentors.
4- Serology: Using pooled antisera to detect monovalent, specific O and K- antigens
.4rd stage Lec.11
Salmonella
Family:EnterobacteriaceaeGenus:Salmonella
Species: Salmonella typhi
Salmonella paratyphi
Salmonella typhimurium
Salmonella enteritidis
Salmonella enterica & others….
.
Morphology:-
-Salmonella are gram-negative, non spore forming bacilli.- Most species motile, with peritrichous flagella.
-They form acid and usually gas from glucose, maltose, mannitol, but do not ferment lactose, sucrose.-Salmonellae are resistant to freezing in water and to certain chemicals, e.g.: brilliant green, sodium tetrathionate and sodium deoxycholate; such compounds inhibit coliform bacilli and are; therefore, useful for isolation of Salmonellae.
-Salmonella species can be identified by biochemical tests and antigenic analysis.
Classification:-
The genus Salmonella is classified into serotypes, according to the surface antigens. There are 3 main antigens:-1- "H" or flagellar antigen
It is inactivated by heating over 60o c and also by alcohol and acids. With sera containing anti-H antibodies, such antigens agglutinate rapidly in large fluffy clumps.2."O" or somatic antigens
It is part of the bacterial cell wall and is resistant to prolonged heating at 100 c, to alcohol, and to dilute acids.
3. The"Vi" antigens
Capsular antigens that are present at the periphery of the bacteria.Vi antigens are destroyed by heating for 1 hour at 60 c and by acids and phenol. Cultures possessing Vi antigens tend to be more virulent than those lacking them.Toxins:-
As in all gram-negative bacteria, the cell walls of salmonellae contain lipopolysacchrides (LPS). These are liberated upon lysis of the cell and act as endotoxins. Salmonella also produces another toxin called enterotoxin. The Salmonella enterotoxin is readily degraded by heat, so proper cooking of food will destroy the activity of the toxin. The enterotoxin remains inside the bacteria, so the toxin concentration increases with the increase in bacterial numbers.Pathogenesis:-
Salmonella may cause several diseases including gastroenteritis, enteric(typhoid) fever or septicemia. Disease is initiated by oral ingestion of the bacteria followed by colonization of the lower intestine. The bacteria are capable of mucosal invasion, which results in an acute inflammation of the mucosal cells. This increases fluid production and release of fluid into the intestinal lumen, resulting in diarrhea.
Salmonella gastroenteritis (food poisoning) is the most common form of salmonellosis and generally requires an 8-48 hour incubation period and may last from 2-5 days. Symptoms include nausea, vomiting and diarrhea. Salmonella enteritidis is the most common isolate.
Enteric or typhoid fever occurs when the bacteria leave the intestine and multiply within cells of the reticuloendothelial system. The bacteria then re- enter the intestine, causing gastrointestinal symptoms. Typhoid fever has a10-14 day incubation period and may last for several weeks. Salmonella typhi is the most common species isolated.
Bacteremia does occur in 5 percent of adults with Salmonella gastroenteritis and can result in hematogenous spread to the heart (endocarditis), spleen, bone (Osteomyelitis), and joints (reactive arthritis), although blood cultures are rarely positive.
Diagnosis:
Salmonella bacteria can be detected in stool or blood cultures. Specimens are blood or feces. In the stool, the laboratory is challenged to pick out Salmonella from
many other similar bacteria that are normally present.
The main steps for isolation are:
1- Enrichment culture: The specimen (usually stool) is put into Tetrathionate broth1-2 days to inhibit normal flora and permit replication of salmonellae.
2- Inoculation on:
MacConkey agar: (Non-lactose fermentor colonies). Salmonella-Shigella agar (S.S agar): permit good growth of salmonellae over other Enterobacteriaceae.
Bismuth sulfite agar permits rapid detection of S.typhi which forms black colonies because of H2S production.
3- Final identification:
Biochemical reactions: Indole –ve, Motility +ve, Urease –ve, TSI –alkaline/acid/gas/hydrogen sulphide.
Transmission and epidemiology:-
Source of infection: the sources of infection are food and drink that have been contaminated with Salmonella.
Enteric fever is generally transmitted from person to person or
contaminated food or water with human feces and an asymptomatic human carrier.Treatment:
Treatment with antibiotics is not usually necessary; however, if the infection spreads from the intestines, the infection can be treated with Ampicillin, Gentamicin, trimethoprim/sulfamethoxazole, ceftriaxone, amoxicillin, or ciprofloxacin.Rapid tests:-
The length of time required to isolate, serogroup and serotype Salmonella has led to several alternative techniques to develop for speeding up the procedure. Some of these are: Immunoassay
PCR Gene sequencing- DNA hybridization
ELISA rapid test
Shigella
Family: Enterobacteriaceae
Genus: Shigella
Species:
Sh.dysenteriae Sh.flexneri
Sh.boydii
Sh.sonnei
Morphology& Characteristics:
G-ve rods, non motile and usually do not ferment lactose, but do ferment other carbohydrates, producing acid but not gas, they do not produce H2S. Colonies are about 2mm convex, circular, and transparent on MacConkey agar (lactose non-fermentor).Pathogenicity:
- Shigella infections are limited to gastrointestinal tract.- Highly communicable.
- The infective dose is less than 103organisms.- After (1-2 days) incubation period, there is a sudden onset of abdominal pain, fever, and watery diarrhea due to exotoxin acting in the small intestine, stool often contains mucus and blood.- Shigella invade the mucosal epithelium of the intestine causing abscesses in the wall of the large intestine which leads to necrosis of the mucous membrane, superficial ulceration, bleeding and formation of a "pseudomembrane" on the ulcerated area.
- Symptoms subside spontaneously in 2- 5 days. However in children and elderly disease may lead to dehydration and even death.
-Epidemiologically, shigellae are transmitted by "food, fingers, feces and flies" from person to person.
Toxins:
1- Endotoxin: (lipopolysaccharide) upon lysis, causes irritation of the bowel wall.
2- Shigella dysenteriae Exotoxin: A heat- labile exotoxin that affects both the gut and the central nervous system, and may contribute to the severity and fatal nature of Sh. dysenteriae infections.
Diagnosis:
1- Specimens: stool or rectal swabs for culture. Serum specimens must be taken 10 days apart to demonstrate a rise in antibodies titer.2- Culture: a) Specimens are cultured on differential selective media e.g.: MacConkey or EMB agar, and on thiosulfate-citrate- bile agar, which suppress other Enterobacteriaceae and G+ve bacteria.
b) Colorless (non-lactose- fermentors) colonies are inoculated into TSI:
Alkaline/acid/no gas/no hydrogen sulphide and non motile are suspected to be Shigella spp. and should be subjected to slide agglutination by specific Shigella antisera .Treatment:
Chloramphenicol, Ampicillin, tetracycline, and trimethoprim are most Commonly inhibitory for Shigella isolates and can suppress acute clinical attacks of dysentery.4rd stage Lec.12
Genus: Proteus
Proteus is Gram-negative Proteobacteria. Proteus bacilli are widely distributed in nature as saprophytes. They are opportunistic pathogens, commonly responsible for urinary and septic infections, often nosocomial.
The most important species are:-
1) P. vulgaris,
2) P. mirabilis,Identification
Proteus species do not usually ferment lactose. It is oxidase-negative but catalase- and nitrate-positive. Specific tests include positive Urease (which is the fundamental test to differentiate Proteus from Salmonella). Proteus mirabilis and Proteus vulgaris can be differentiated by an Indole test for which only Proteus vulgaris tests positive.75
Swarming:
Proteus is unique, however, because it is highly motile and does not form regular colonies. Instead, Proteus forms what are known as "swarming colonies" when plated on non- inhibitory media. Swarming is inhibited on MacConkey agar by bile salt. Swarming give rise to a very thin film of bacteria on the agar surface, but swarming periods are interspersed with periods when cells stop and undergo a cycle of growth and division so that the colony has a distinct zonation.
Pathogenicity:
Proteus can cause:1- Urinary tract infections2- Hospital-acquired infections
More than 40% of nosocomial infections are those of the urinary tract, most of these occurring in catheterized patients. Bacterial colonization (including Proteus mirabilis) of the urinary tract and catheters results not only in infection, but also various complications, such as blockage of catheters with crystalline deposits of bacterial origin, generation of gravels and pylonephritis.
About 10-15% of kidney stones are, caused by alkalinization of the urine by the action of the Urease enzyme (which splits urea into ammonia and carbon dioxide) of Proteus (and other) bacterial spp.
Proteus species have also been recovered from infected wounds and abscesses and from cases of otitis media, meningitis, septicaemia and Osteomyelitis.
P. mirabilis:
Proteus mirabilis is the commonest species of Proteus in human infections. It can be found as part of the micro flora in the human intestine. This organism is not usually a pathogen, but does become a problem when it comes into contact with urea in the urinary tract. From there, infection can spread to other parts of the body. P. mirabilis for most of the urinary tract infections that occur in hospital settings and for 90% of Proteus infections It has at least 10 adhesion factors making this organism extremely sticky and motile. It can be easily identifiable in a blood agar plate by the formation of concentric rings of its swarming movementaccounts. . It is motile; The endotoxins of its LPS membrane elicit an inflammatory response from the host.Pathogenicity:
P. mirabilis produces Urease, an enzyme that converts urea into ammonia by the following process:(NH2)2CO→ 2NH3 + CO2.
Infection by P. mirabilis can therefore be detected by an alkaline urine sample (pH 8 and up) with large amounts of ammonia.P. mirabilis can be found as a free-living microbe in soil and water. The organism is also normally found in the gastrointestinal tract of humans.
Urinary tract infections (UTI) are very painful and can become lethal if the infection spreads to other systems in the body.
P. mirabilis causes urinary tract infections primarily through indwelling catheters. P. mirabilis can then adhere to the insides and outsides of the catheter, forming biofilm communities. Once established, these microbes pass through the urethra via swarming motility to the bladder. P. mirabilis binds to bladder epithelial cells where it eventually colonizes. P. mirabilis infection can also lead to the production of kidney and bladder stones. The bacteria colonize the stones as they form, making them less accessible to antibiotic attack.
Most strains of Proteus mirabilis are sensitive to Ampicillin and cephalosporins. Unlike Proteus vulgaris which is not sensitive to these antibiotics. However, this organism is isolated less often in the laboratory and usually targets immunosuppressed individuals.
Pseudomonas :
Pseudomonas is a genus of the family Pseudomonadaceae.This genus is widespread in nature, inhabiting soil, water, plants, animals, and present in small numbers in the intestinal flora and the skin of humans.
Characteristics:-
Gram –ve, rod shaped and polar-flagella bacteria. One or more polar flagella, providing motility
Strictly Aerobic,
Non–spore forming
Lactose non- fermenting
pos HYPERLINK "http://en.wikipedia.org/wiki/Catalase" \h itive catalase test
*Positive oxidase test.
More than half of all clinical isolates produce the blue-green pigment pyocyanin. Pseudomonas often has a characteristic sweet odor.
Biofilm formation:-
A significant number of cells can produce exopolysaccharides known as biofilm, which makes it difficult for pseudomonads to be phagocytosed by white blood cells, and difficult to remove from food preparation surfaces. Growth of pseudomonas on spoiling foods can generate a "fruity" odor.
Pseudomonas has the ability to metabolize a variety of diverse nutrients.
Combined with the ability to form biofilms, they are thus able to survive in a variety of unexpected places. For example, they have been found in areas where pharmaceuticals are prepared, a simple carbon source, such as HYPERLINK "http://en.wikipedia.org/wiki/Soap" \h soap residue. Other unlikely places where they have been found include HYPERLINK "http://en.wikipedia.org/wiki/Antiseptic" \h antiseptics, and bottled mineral water.
A biofilm microcolony formed by P.aerugenosa
Pigment production:-The Pseudomonas group produces water- soluble pigments. Strains of P.aerugenosa producedifferent pigments:
- The nonfluorescent bluish pigment pyocyanin, which diffuses into the agar.
-The fluorescent pigment pyoverdin which gives a greenish color to the agar.-Some strains produce the dark red pigment pyorubin or the black pigment pyomelanin.
Other Pseudomonas species are nonpigmented (e.g. P.mallei)
Pathogenicity:-The members of this genus HYPERLINK "http://en.wikipedia.org/wiki/Opportunistic_pathogen" \h are opportunistic pathogens and demonstrate a great deal of metabolic diversity, some (e.g.: P.alcaligenes) are capable of growth at 4oc which may result in fatal infection if contaminated products are refrigerated and later used for intravenous therapy. Two species, P. pseudomallei and P. mallei, cause severe and often fatal infections and must be processed with extreme caution in the laboratory.
Pseudomonas aeruginosa can transmit through contaminated water, Inhalation of aerosols, Medical devices rinsed with the contaminated water or indirect contact from contaminated surfaces via health worker’s hands.
Pseudomonas aeruginosa is invasive and toxigenic and has become an important cause of infection, especially in patients with compromised host defense mechanisms. It is the most common pathogen isolated from patients who have been hospitalized longer than 1 week. It is a frequent cause of nosocomial infections such as
pneumonia, urinary tract infections (UTIs), and Bacteremia.
Pseudomonal infections are complicated and can be life threatening. Adding to its Pathogenicity; this bacterium has minimal nutritional requirements and can tolerate a wide variety of physical conditions.
Skin: Pseudomonas does not grow on dry skin, but it flourishes on moist skin. Green nail syndrome is an infection that can develop in individuals whose hands are frequently submerged in water; it also causes secondary wound infections that have characteristic blue-green pus with a fruity odor.
Burns infections: Pseudomonas also has emerged as an important source of burn wound sepsis. Invasive burn wound sepsis is defined as the bacterial proliferation of100,000 organisms per gram of tissue, with subjacent involvement of subjacent unburned tissue.
Eye:-P aeruginosa is a common cause of HYPERLINK "http://emedicine.medscape.com/article/1194028-overview" \h bacterial keratitis, scleral abscess, and endophthalmitis in adults and ophthalmia neonatorum in children.
Symptoms are pain, redness, swelling, and impaired vision and may lead to rapid destruction of the eye.
The bacterium is often found in mild otitis externa in swimmers. P aeruginosa may invade the bloodstream and result in fatal sepsis or meningitis.
Diagnosis:-
1- Pseudomonas will grow well on blood agar, sometimes with hemolysis; appear on culture in green color after few days. Lactose non- fermentor on MacConkey agar.2- Sometimes produce a sweet or grapelike odor.
3- gram stain(gram negative )4- oxidase +ve, catalase +ve
5- grow in 42C*
6- floursent under UV.
Treatment:-
Pseudomonas aeruginosa is frequently resistant to many commonly used antibiotics and should not be treated with single- drug therapy. The combination of gentamicin and carbenicillin is frequently used to treat severe Pseudomonas infections.Use as bioremediation agents
Some members of the genus Pseudomonas are able to metabolize chemical pollutants in the environment, and as a result can be used for bioremediation (e.g. P. pseudoalcaligenes is able to use cyanide as a nitrogen source).4rd stage Lec.13
Genus: Vibrio
Family: VibrionaceaeThe important genera belonged to this family are:
1- Genus: Vibrio2- Genus: Aeromonas
3- Genus: PlesiomonasAbout 12 of the 35 Vibrio species have been implicated in gastrointestinal and extra intestinal infections in man. The most important of these is V.cholerae. Other species of Vibrio are: V. parahaemolyticus, V. vulnificus, V.mimicus, and V. alginolyticus.
Vibrio cholerae:
- V. cholerae is short, often curved, gram –ve rods, motile by a single polar flagellum, facultatively anaerobes, oxidase +ve and reduce nitrate to nitrite.- Whereas most Vibrio species are halophilic grow optimally with 3% NaCl, V. cholerae is non- halophilic and grow well in ordinary media.
- It forms a fine surface pellicle in liquid media e.g. peptone water.
- Most strains grow well on MacConkey agar giving pale colonies (lactose non- fermenting).
- The optimal pH for V. cholerae is 8.2. Alkaline peptone water (pH: 8.6) is useful for enrichment of vibrios from feces or other contaminated materials.- Their growth is inhibited in acidic condition (pH< 6.8) and they are rapidly killed at pH<5.0.
- survive up to a few days on moist fruits, vegetables, and cooked foods.
- Easily killed by disinfectants and moist heat (56oc in 30 min.).- Selective media for isolation of V. cholerae is TCBS agar (thiosuphate citrate bile- salts sucrose), on this media V. cholerae colonies are yellow (sucrose- fermentor) and other sucrose non- fermentor vibrios (e.g.: V. parahaemolyticus) are green.
Differential tests:
String test is used to separate Vibrio spp. from Aeromonas andPlesiomonas. In this test, organisms are emulsified in 0.5% Sodium deoxycholate, which lysed the vibrio cells, but not those of Aeromonas spp.and Plesiomonas spp. with cell lysis there is release of DNA,which can then be pulled up into a string using a inoculating loop.
V.cholerae cell growth on TCBS String test
V.cholerae and V. mimicus are the only Vibrio spp. that do not require salt for growth. A key test in separating other vibrios which are halophilic is growth in nutrient broth with 6% NaCl.
The colonies of vibrios resemble those of the family Enterobacteriaceae, but differ by their positive oxidase test. The oxidase test must be performed from medium with fermentable sugar (e.g.: lactose in MacConkey agar or sucrose in TCBS) to avoid a false – ve test if pH is below 5.1.
Antigenic structure:
All strains of V.cholerae share a common, heat- labile H flagellar antigen that is of no value in epidemiological studies.V.cholerae serotypes are based on somatic (O) antigens. Serotype O1 is the most important because almost all strains isolated from epidemic cholera have belonged to serogroup O1. Serotype O1 is further divided into two biotypes: Classical and El Tor.
The El Tor biotype named after the quarantine camp where it was first isolated from pilgrims returning from Mecca, differs from classical type, and has now spread and largely displaced the classical biotype.
In 1992 a new non- O1 strain (O139) arose in south India.
The name "Non-Cholera Vibrio"(NCV) is used for strains of V.cholerae of serotypes O2 to O138 to distinguish them from the strains of serogroup O1 and O139 which are associated with epidemic cholera.Other species of Vibrio cause a variety of infections in humans.
Biotypes
El Torclassical
Ogawa
V.choleraeSerotype O1 serosubgroups Inaba
Hikojima
phage types
genus Vibrio non-O1 – other serotypes
non-agglutinating vibrios non-cholera vibrios
other species
V. parahaemolyticus—food-associated diarrheal disease
V. vulnificus—wound infection; septicemia
V. alginolyticus—otitis externa; wound infection
Pathogenesis:
Cholera is an acute, non-invasive infection of gastrointestinal tract.Incubation period is1-4 days. There is a sudden onset of nausea and vomiting and profuse diarrhea with abdominal cramps. The mortality rate without treatment is 25%- 50%.
The organisms do not reach the blood stream, but remain with the intestinal tract, where they multiply and liberate enterotoxin [(Cholera toxin (CT)], which causes mucosal cells to hyper secret water and electrolytes and results in profuse watery diarrhea (resembles rice water) leading to fluid loss, then severe dehydration and hypotension, if untreated lead to death
Lab Diagnosis:
Specimen should be processed without delay, or should be placed in a liquid alkaline transport medium to prevent the overgrowth of other organisms.1) Inoculation in Alkaline peptone water and incubation for 6-8 hr.
2) Then inoculation on TCBS for 24hr at 37oC→ large, yellow. Translucent colonies(suspected colonies).
3) For final diagnosis colonies should be transferred onto:
a) Kligler: (double sugar fermentation, gas +ve, H2S +ve)
b) Semi solid Mannitol: (motile, Mannitol fermentation +ve). c) Alkaline peptone water (Indole +ve, V.P. +ve).
4) Oxidase test +ve (done with wooden stick to avoid false +ve result).
5) The API 20E system gave accurate identification of vibrios.
6) Agglutination tests using anti- O1 antiserum.
Kligler test Oxidase test
API 20E system
Treatment:The most important part of therapy is water and electrolyte replacement to correct severe dehydration and salt depletion.
Most strains are sensitive to Tetracycline, Chloramphenicol, Ampicillin and Trimethoprim.
4rd stage Lec.13
The Gram positive spore- forming rod
These rods are divided into:
1) Aerobic (Bacillus)2) Anaerobic (Clostridium)
Genus: BacillusThe most important pathogenic member belonged to this genus is:
Bacillus anthracis
General characters:
It is one of the largest bacteria (4- 10µm) in length. The end of the bacillus is concave and swollen (bamboo stick). They occur in chains, long chains are formed in culture but short chains formed in the host body. Capsules are found in smears from infected animals, but not in culture except in enriched media. Spores are formed in soil only; they are seen either free or in the center of the cell.They are aerobic, colonies are irregular, raised, grayish white, non-haemolytic, ferment many sugars; Catalase +ve
Antigens:
It has three main antigens:1) Capsular antigen: (virulence antigen)
2) Somatic polysaccharide in cell wall.
3) Somatic protein: Stimulate antibody production.
Toxins:
The virulence of B. anthracis is due to at least 2 factors:1) Extracellular toxin: (fractions I, II, III).
2) Capsular polysaccharide: antigenic factor.
Anthrax toxin is lethal and its main effect is increasing vascular permeability.
Pathogenicity:Anthrax is a septicaemic disease of sheep and cattle. Infection may take place by:
1- Skin: (results malignant pustule).2- Inhalation: (haemorrhagic meningitis).
3- Ingestion: violent enteritis with blood diarrhea.The spores germinate and the vegetative cells produce toxin leading to the formation of oedema and hemorrhage. The bacilli may reach the In man, the infection is acquired from animals and infections occur mostly through farmers, butchers, veterinary surgeons, through skin (cuts, hair follicle), lesions of all sizes may be produced, they start as a papule then become a pustule within 12- 48 hrs with an oedemateous area around a black central necrotic area.
Lab diagnosis:
Handling of B. anthracis should be carried out with the greatest care, specimens is taken from lesions, exudates, sputum, etc:1) Microscopic exam: Films are made from exudates, sputum…. And stained by Gram's
method to detect the presence of Gram +ve chains of non- sporing bacilli.2) Cultures are made on blood and Nutrient agar, smears from cultures show G +ve chains of bacilli several showing central spores.
3) Animal inoculation (guinea pigs).
4) Serological tests:Infected tissue extract + anthrax antiserum = precipitation (means test is positive).
Treatment:Anthrax bacillus is sensitive to Penicillin, Streptomycin, Tetracycline and Chloramphenicol.
Bacillus subtilis:
Gram +ve rods occur in chains or singly, motile and non capsulated. Produce β- haemolytic zone on blood agar, they don't produce any toxin, they are opportunistic.
Bacillus cereus:
B.cereus produces several enterotoxins, which cause disease is more an intoxication than a food- borne infection. This disease is of two forms: the emetic type and the diarrheal type.B.cereus has also been associated with various opportunistic infections.
92