To describe he knee joint, ligaments, structure &
neurovascular supply
To demonstrate the ankle joint anatomy
To list the main features of other lower limb joints
To list main groups of lymph nodes in the LL

The knee joint:
This is the largest synovial joint in the
body.
It consists of:
1- The weight bearing tibio-femoral
articulation.
2- The patello-femoral articulation
which directs the pull of quadriceps
tendon anteiorly on the tibia without
tendon wear.

General characteristics:
Basically the joint is a hinge joint that allows mainly flexion - extension
movement, though the actual movements are more complex.
Like all hinge joints, the knee joint is reinforced by two collateral ligaments.
In addition, two very strong ligaments (the cruciate ligaments) interconnect
the adjacent ends of the femur and tibia and maintain their opposition during
movement
Two fibrocartilaginous menisci, between the femoral condyles and tibia
accommodate changes in the shape of the articular surfaces during
movements.
Because the knee joint is involved in weight bearing, it has an efficient
'locking' mechanism to reduce the amount of muscle energy required to keep
the joint extended when standing.
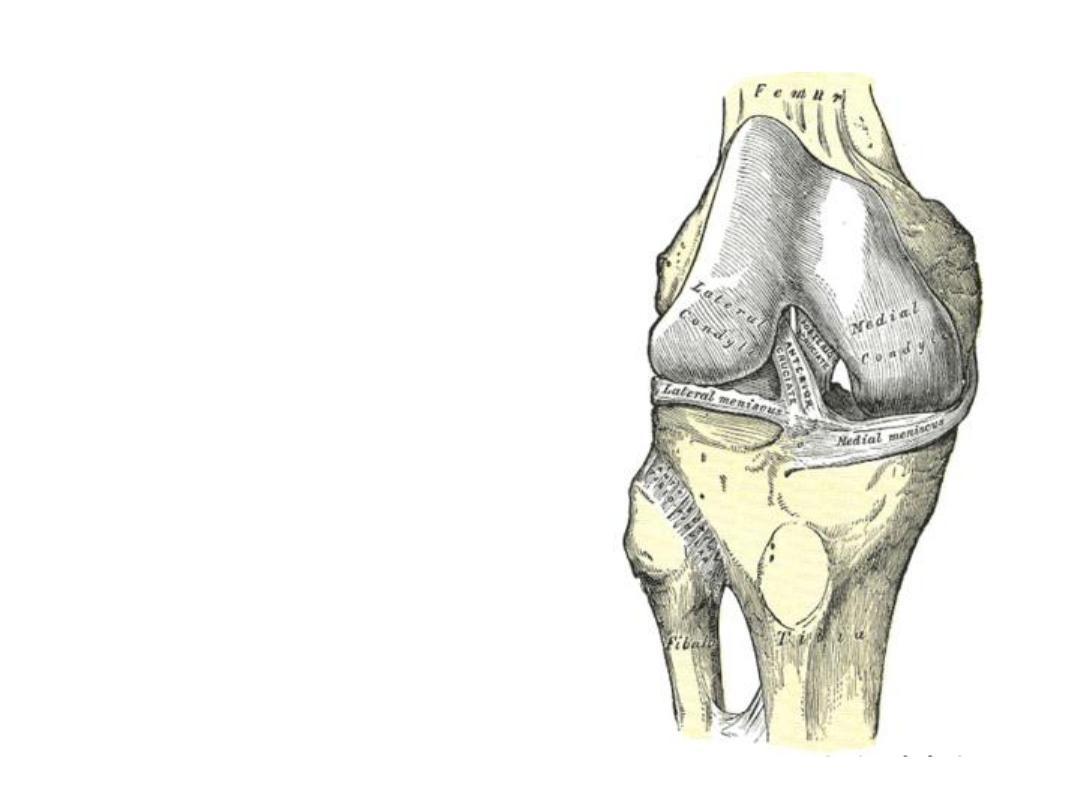
Articular surfaces:
-Like all synovial joints, articular surfaces are covered by hyaline cartilage.
-The major surfaces involved include:
1- Tibio-femoral articulation:
A-The two femoral condyles;
- The medial is longer, narrower & more concave
- The lateral is more anteriorly projecting.
B-The superior aspect of the tibial condyles.
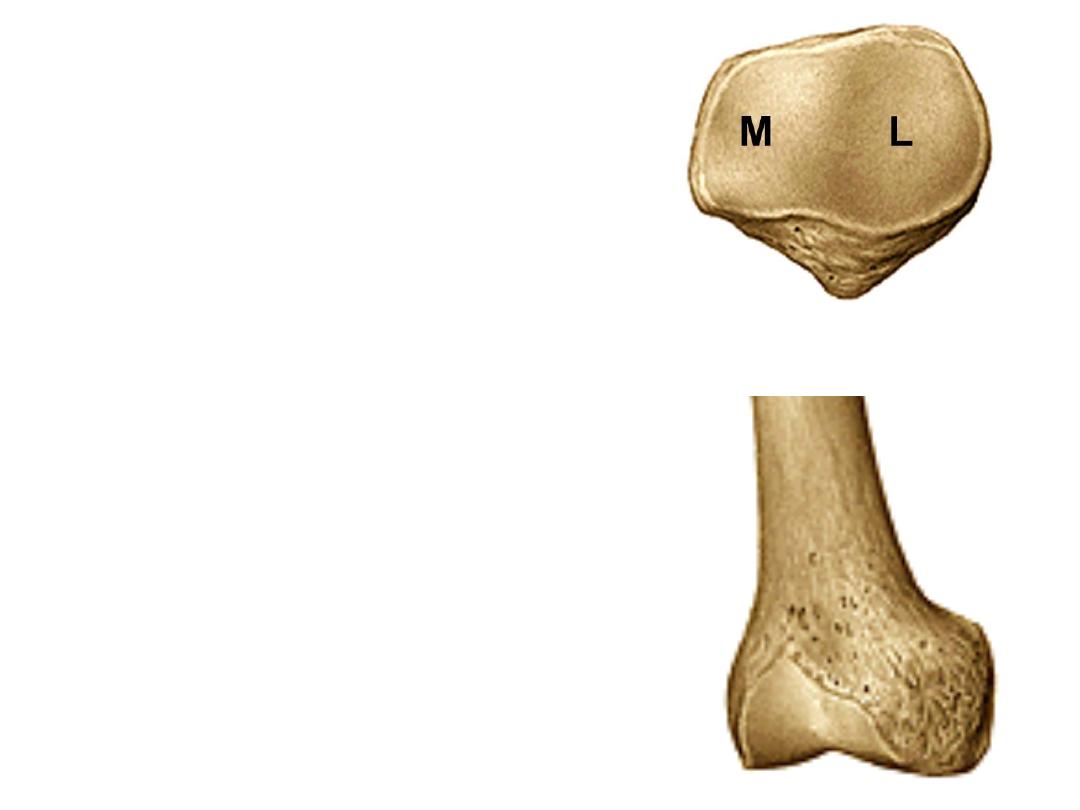
2- Patello-femoral articulation:
A-The patellar surface of the femur.
B- Posterior surface of the patella, the
lateral aspect is wider than the medial
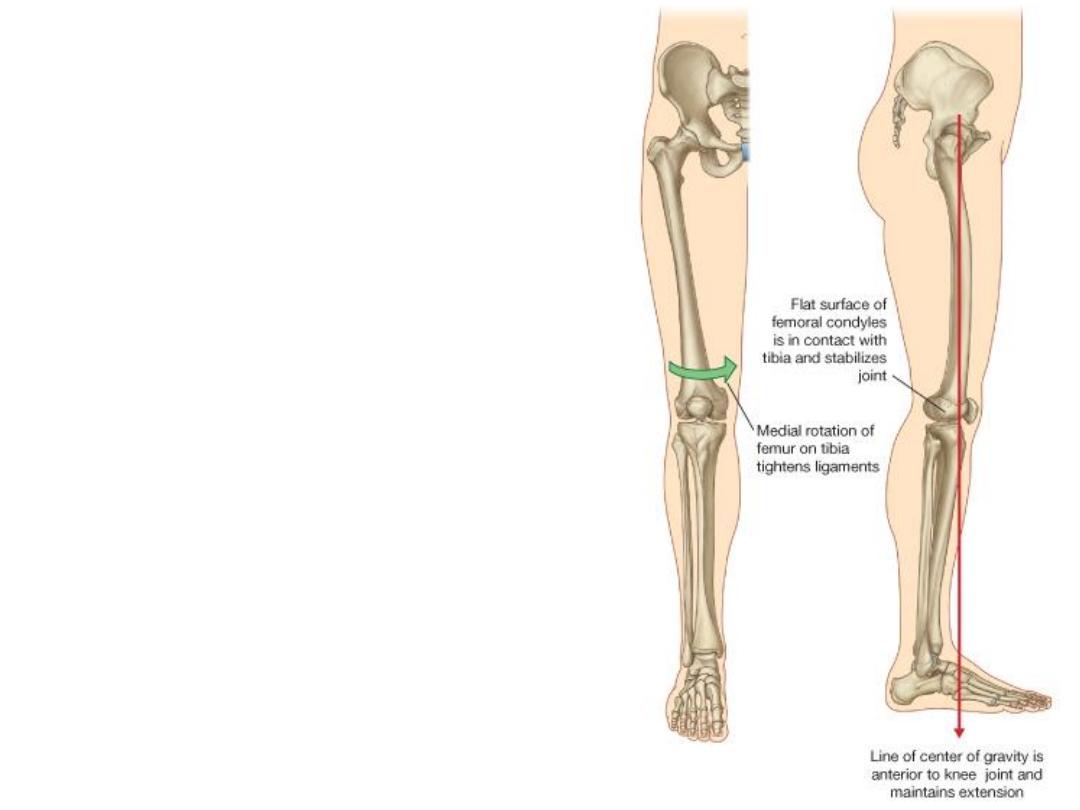
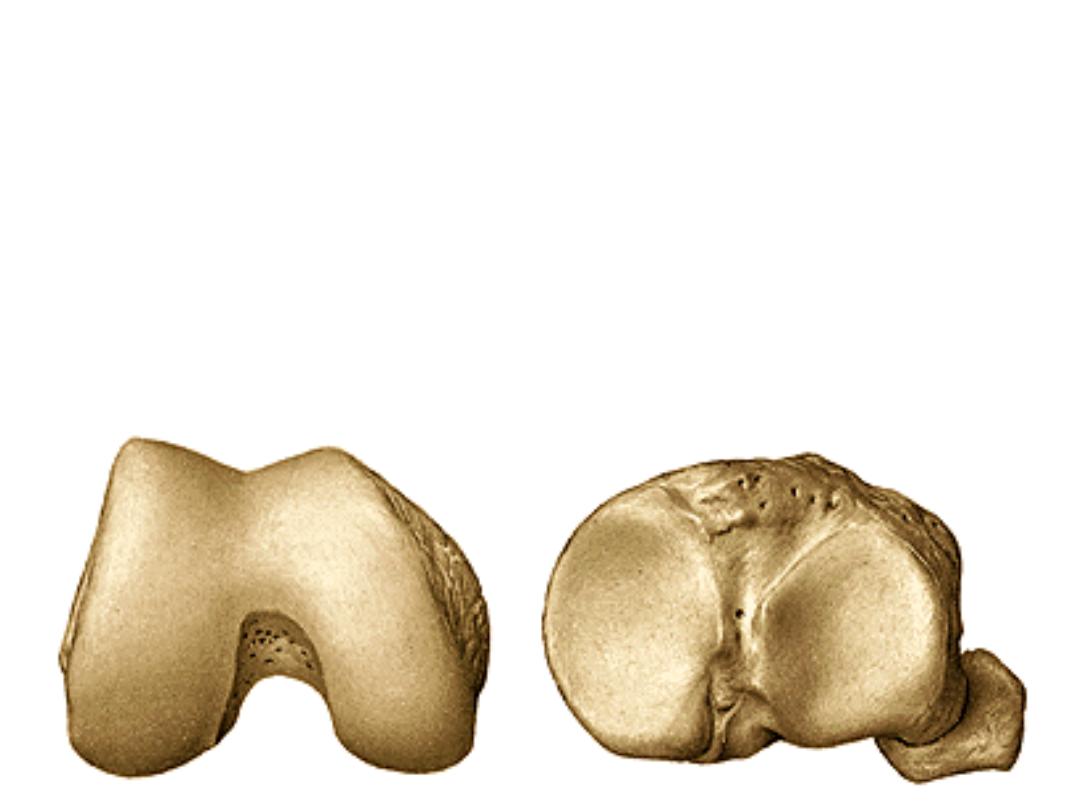
Locking mechanism (screw-home
movement):
-When standing, the knee joint is
'locked' into position to reduce the
amount of muscle work needed to
maintain the standing position
Iliotibial tract keeps this etended
position
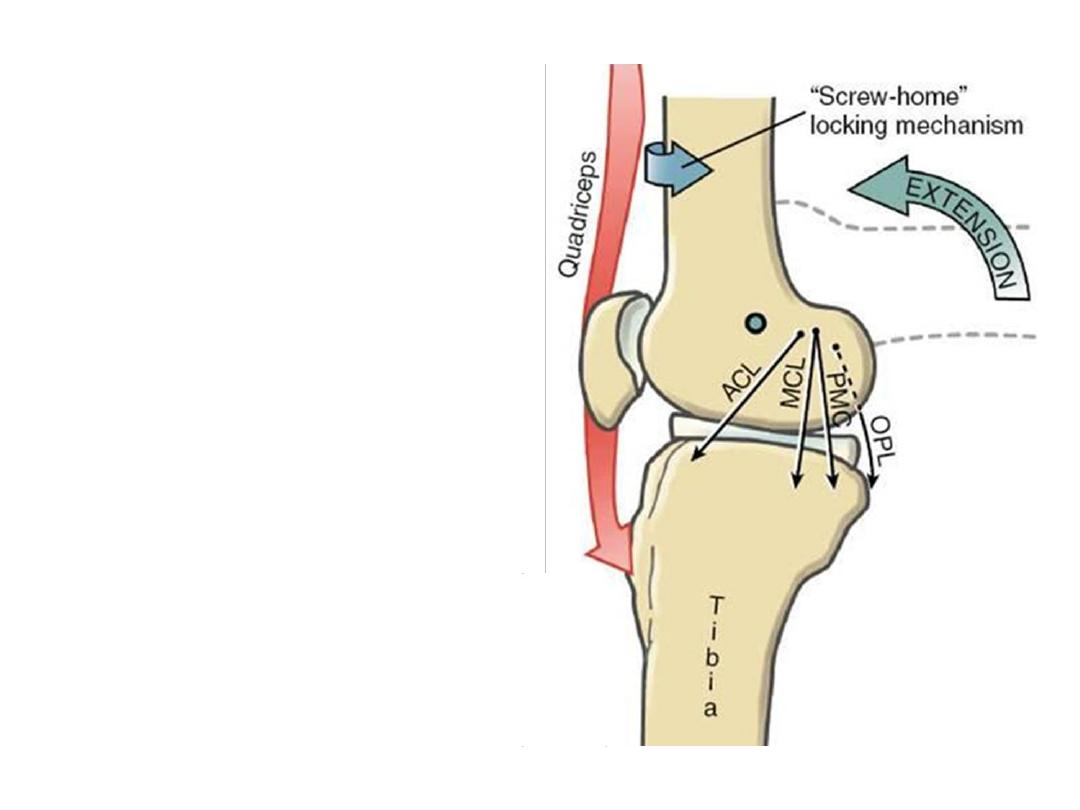
-This locking is provided by the
element of medial rotation that
accompanies extension during
standing
i.e; because of the shorter LFC it
will stop moving before the MFC
which will still rotating on the
tibia till full locking of the joint
occurs.
Popliteus muscle unlocks the
knee by initiating lateral rotation
of the femur on the tibia
Don’t be confused!
The LFC in this view looks longer than the medial but this
is because this is the full length of the articular surface of the LFC while there
is more posterior articular surface is remaining for MFC for the locking
mechanism
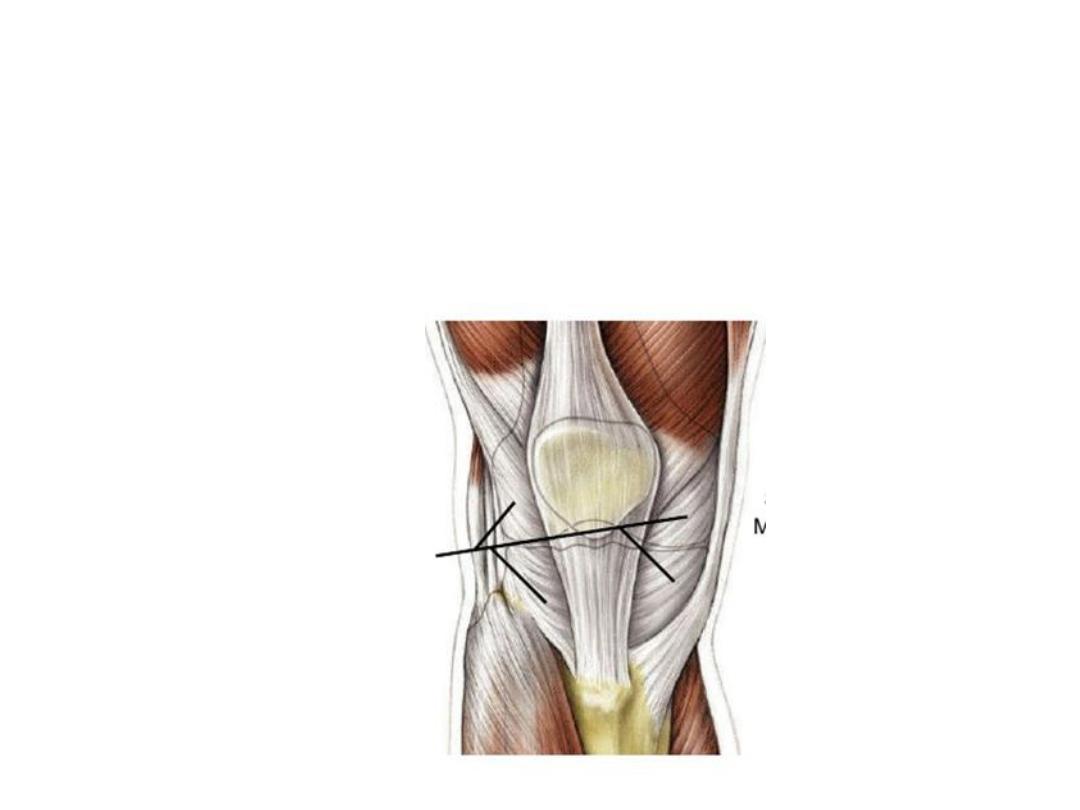
Fibrous membrane:
-The fibrous capsule encloses the articular cavity and the intercondylar region.
-Medially blends with the tibial collateral ligament and is attached to the medial
meniscus.
-Laterally it neither blends with fibular collateral ligament nor attached to the
lateral meniscus
-Anteriorly, the capsule is attached to the margins of the patella
-Popliteus tendon pierces the capsule to insert on the lateral femoral condyle.
-Muscles contributing to the capsule are:
1- Vasti medialis & lateralis (patellar retinacula)
2- Semimembranosus (oblique popliteal ligament)
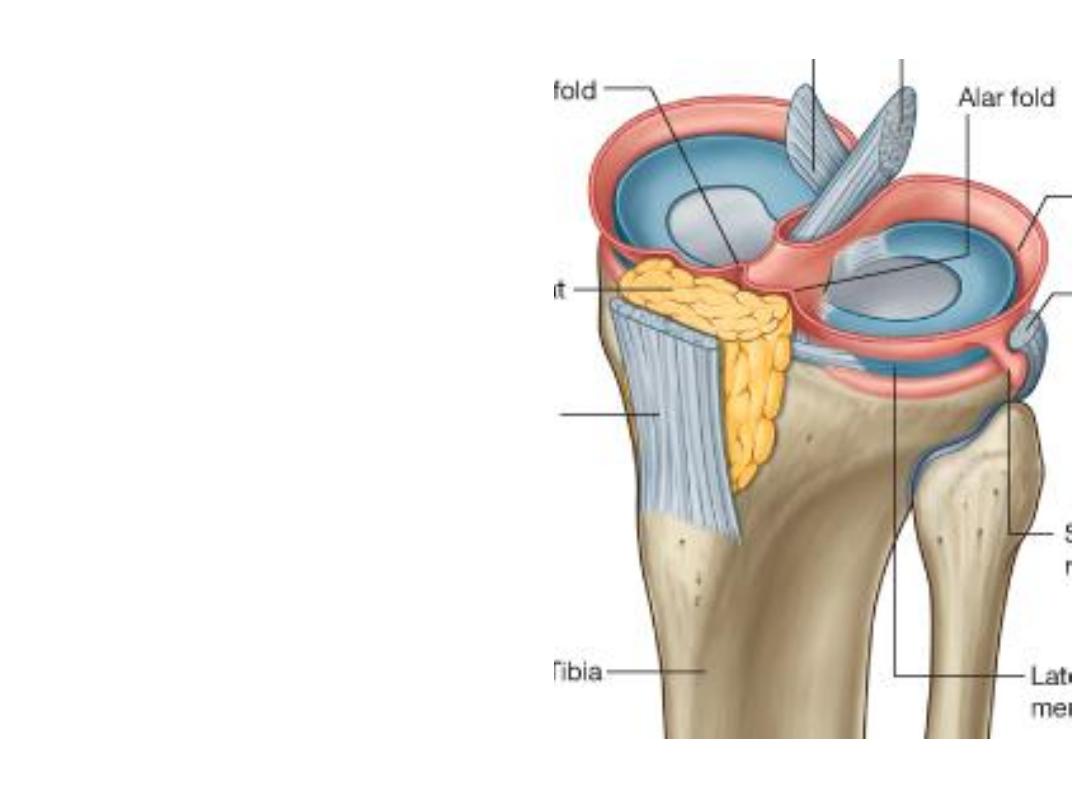
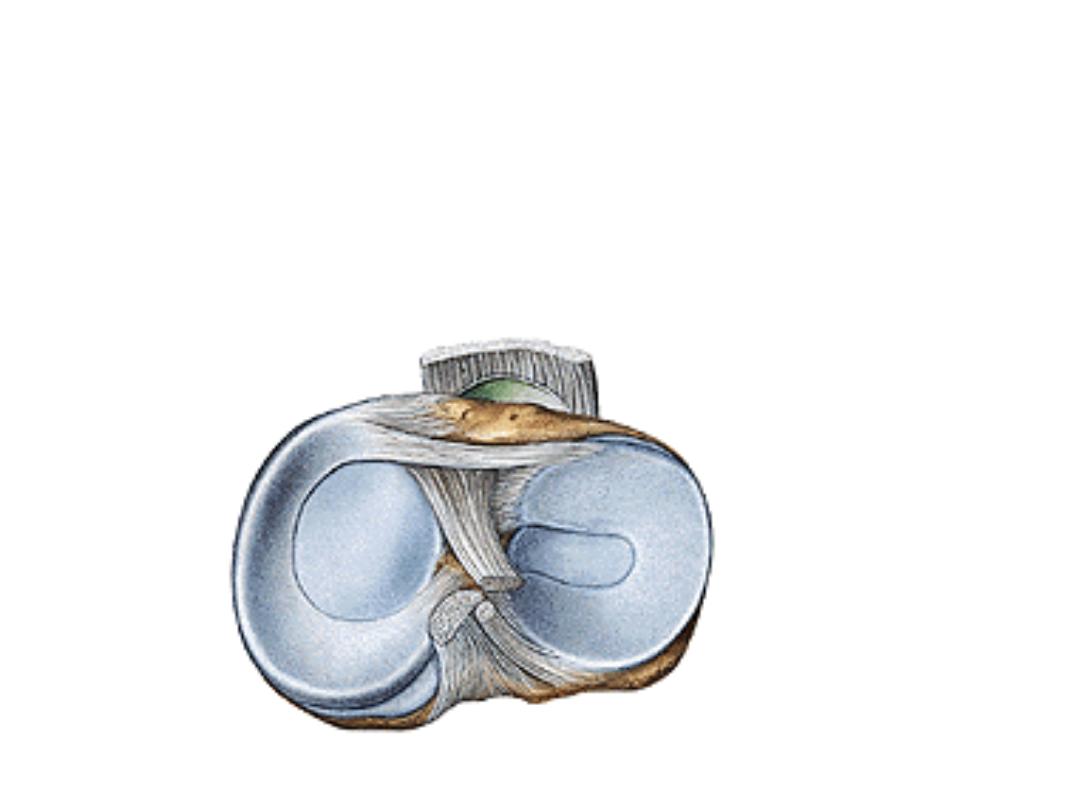
Synovial membrane:
-This membrane attaches to the
margins of the articular surfaces
& to the outer margins of the
menisci
- The two cruciate ligaments,
though within the capsule, they
lie outside the articular cavity.
-Anteriorly,
the
synovial
membrane is separated from the
patellar
ligament
by
an
infrapatellar fat pad.
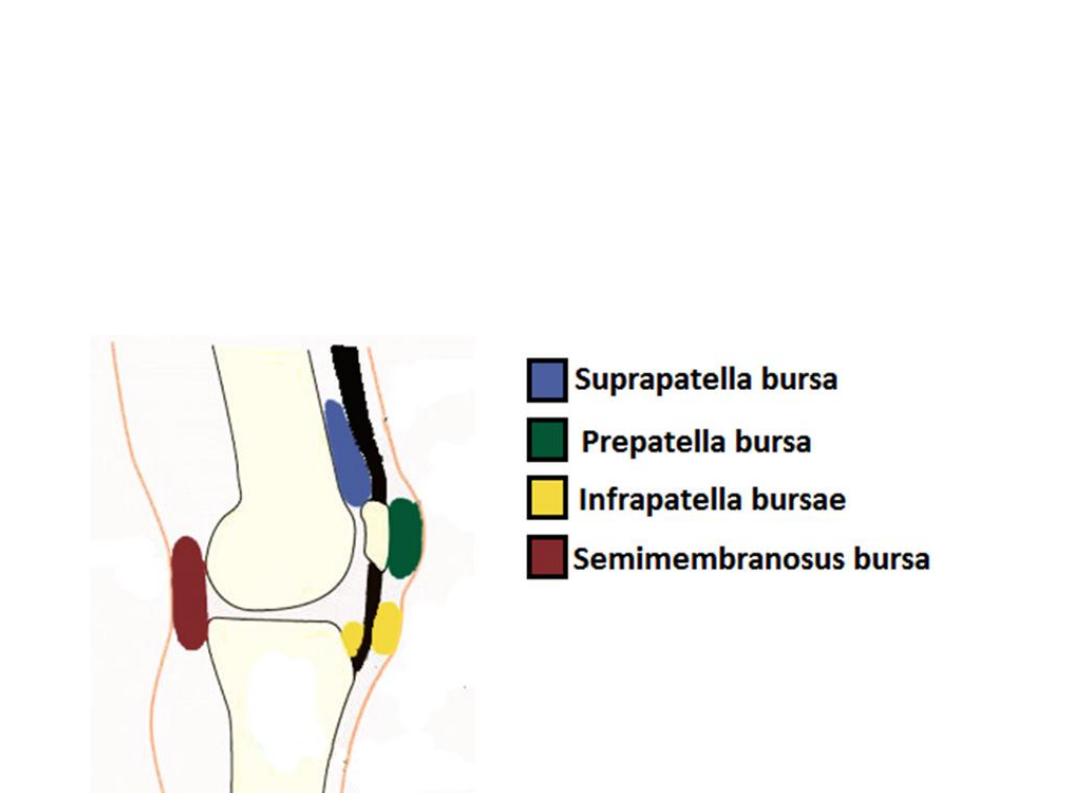
Knee joint bursae:
1- Subpopliteus bursa;
between popliteus tendon & lateral femoral condyle.
2- Suprapatellar bursa:
between quadriceps tendon & the front of femoral haft.
3- Subcutaneous prepatellar bursa.
4- Deep and subcutaneous infra-patellar bursae
5- Semimembranosus bursa
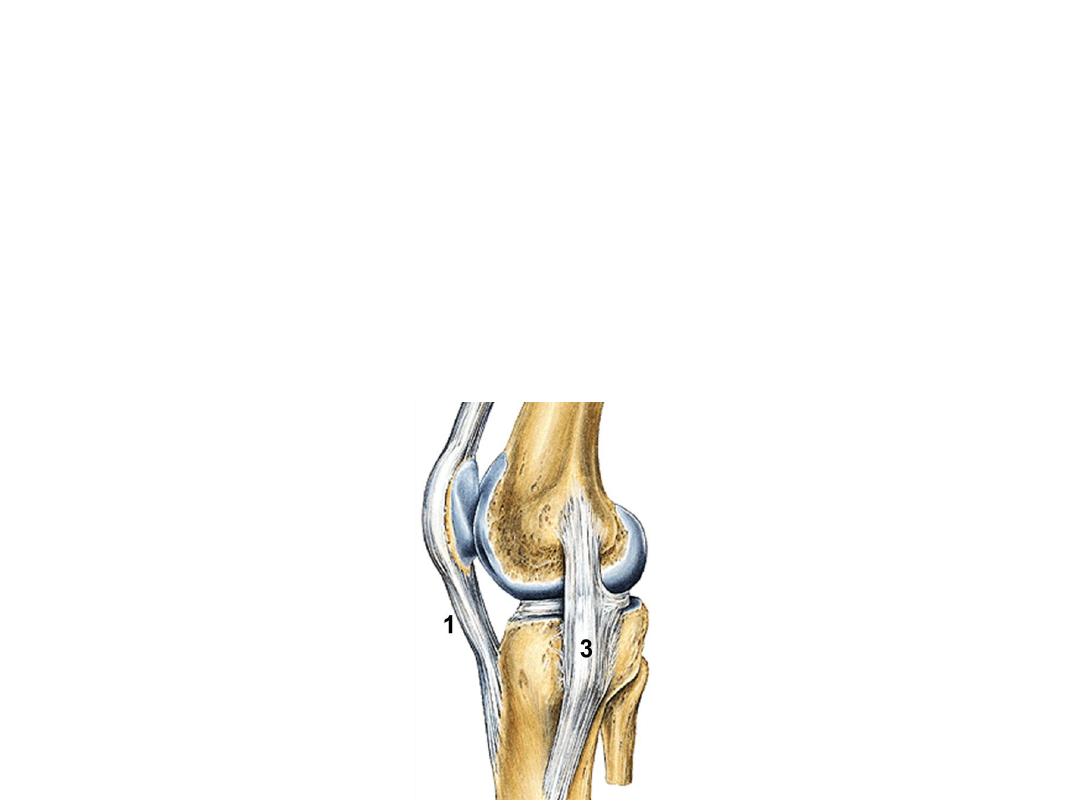
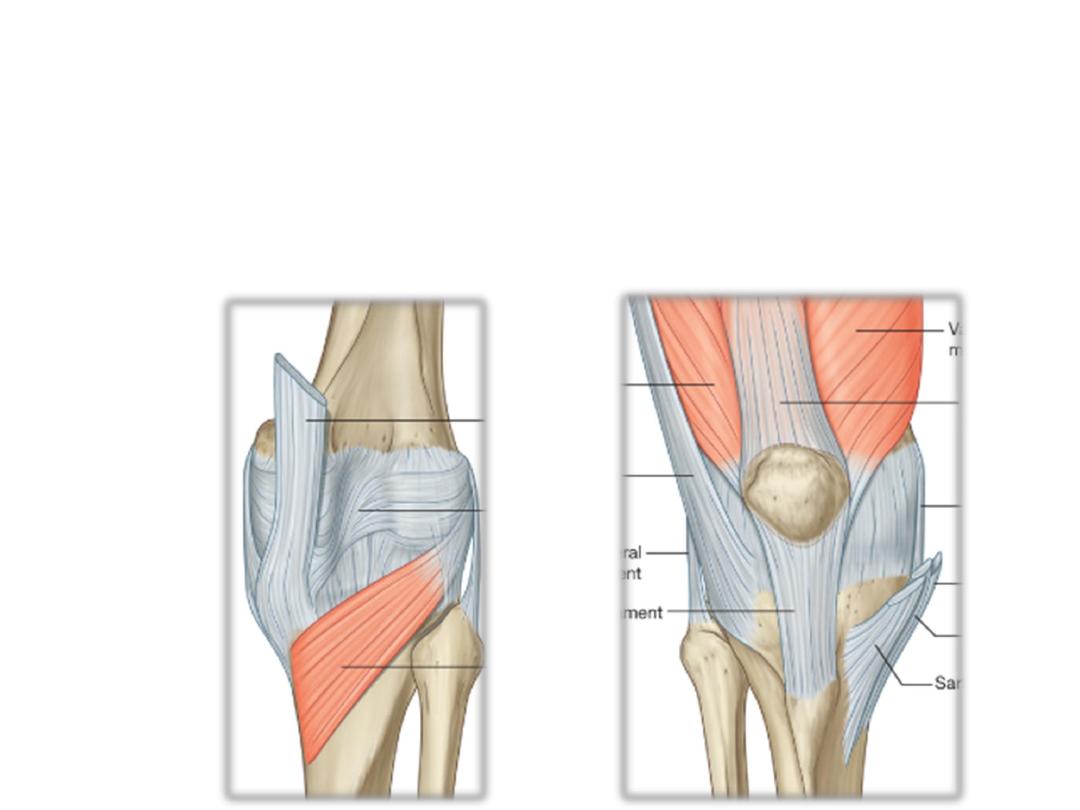
Ligaments:
1- The patellar ligament:
Is basically the continuation of the quadriceps femoris
tendon inferior to the patella.
2- Fibular collateral L:
a cord-like L attached superiorly to the lateral femoral
epicondyle & Inferiorly to the lateral surface of the fibular head, it is NOT
attached to the capsule
3-The tibial collateral L:
a broad L extends between the medial femoral
epicondyle & medial surface of the tibia, it is ATTACHED to the capsule
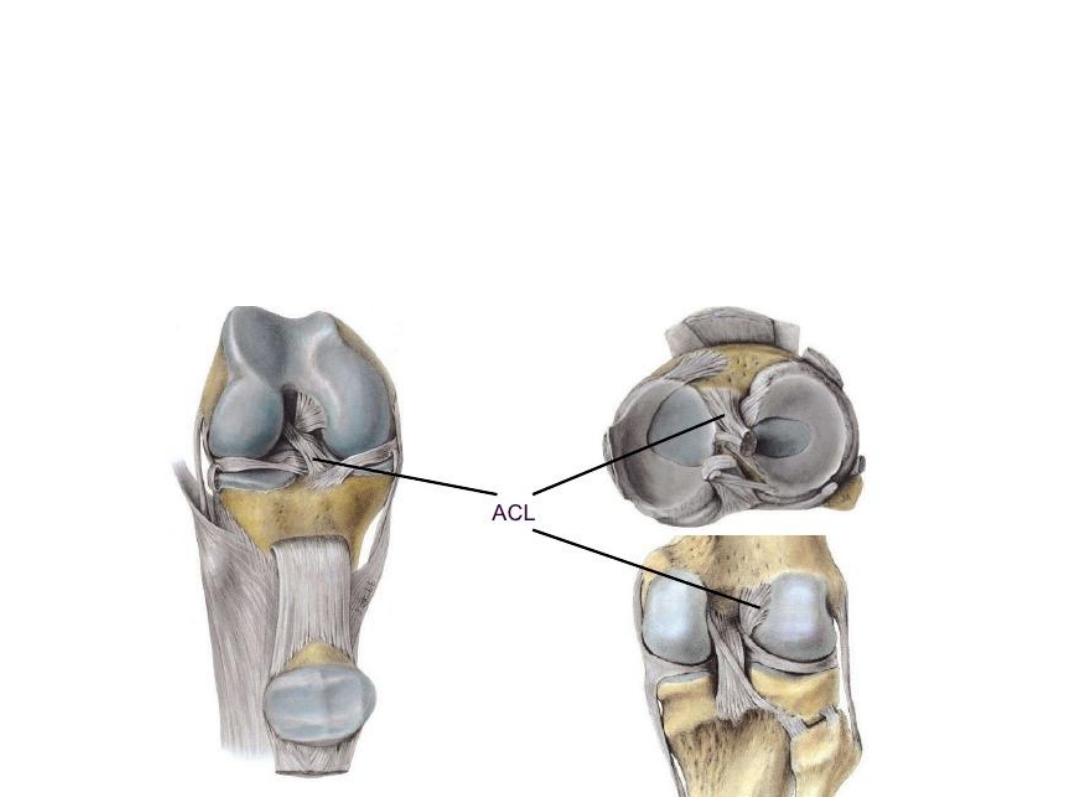
4- The cruciate ligaments:
-The Anterior CL
extends between the anterior part of the intercondylar area of
the tibia & the lateral wall of the intercondylar fossa of the femur
-The anterior cruciate ligament prevents anterior displacement of the tibia
relative to the femur
-Supplied by the middle genicular artery
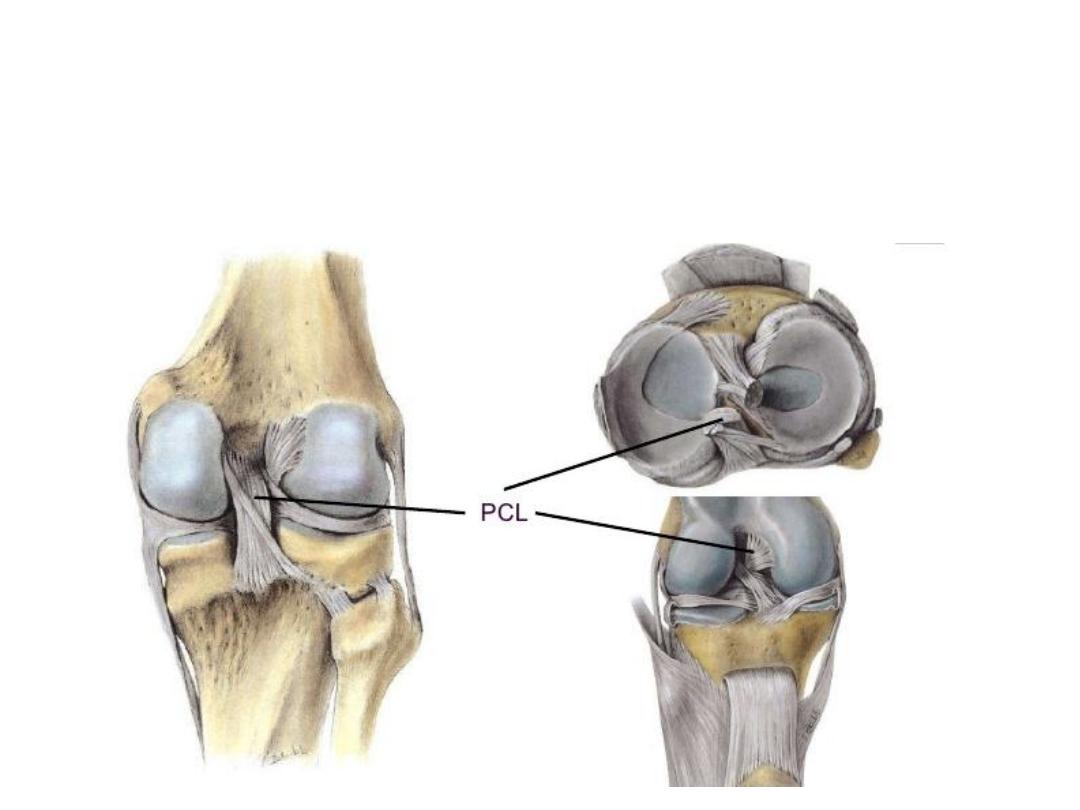
-The Posterior CL
extends between the posterior aspect of the intercondylar
area of the tibia & the medial wall of the intercondylar fossa of the femur.
-It restricts posterior displacement of tibia relative to femur
-Supplied by the middle genicular artery
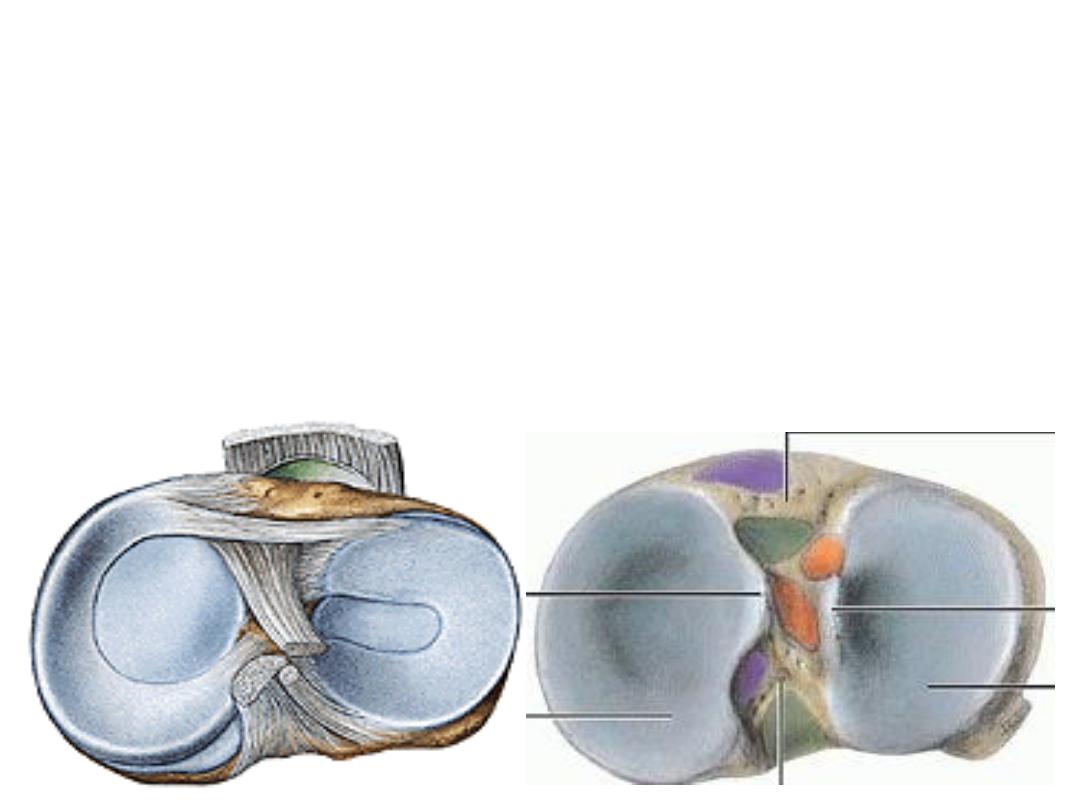
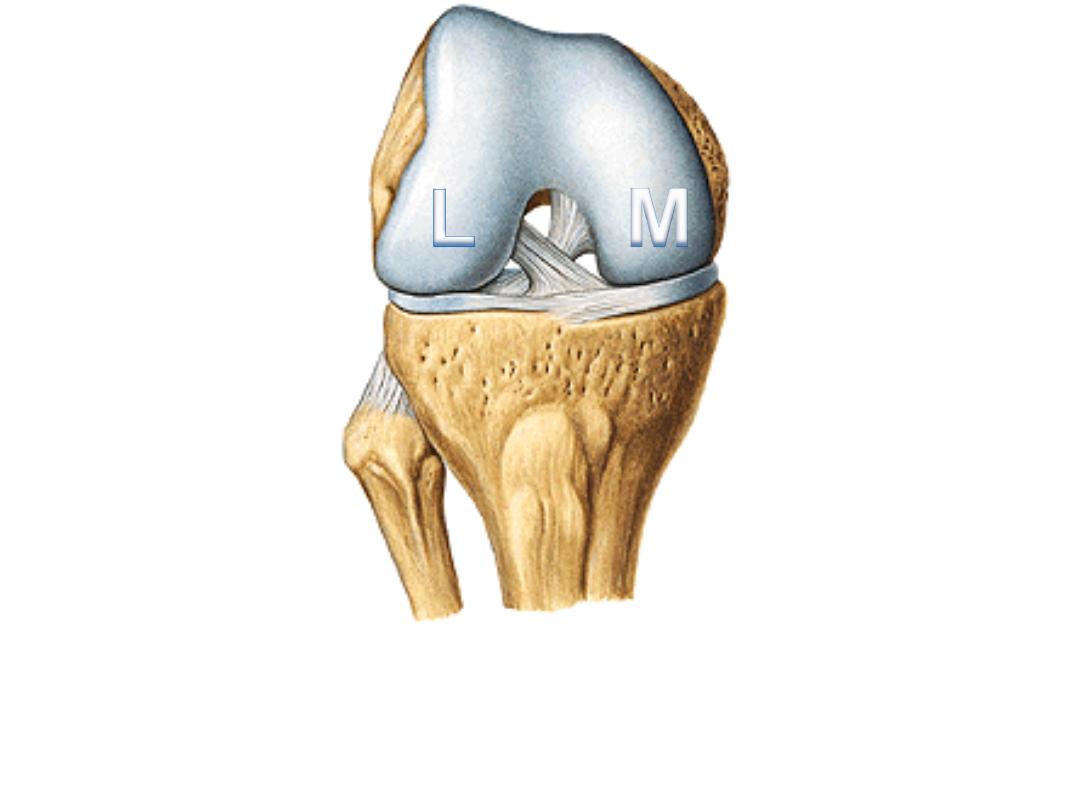
The menisci:
-These are C-shaped, medial & lateral fibrocartilaginous structures
-MM is semilunar while LL is almost circular
- Both are attached at each end to the intercondylar region of the tibial plateau
-Both are connected to each other anteriorly by the transverse ligament of the
knee
-Their function is to improve congruency between articular surfaces during
movements
MM
LM
ACL
PCL
MM
MM
LM
LM
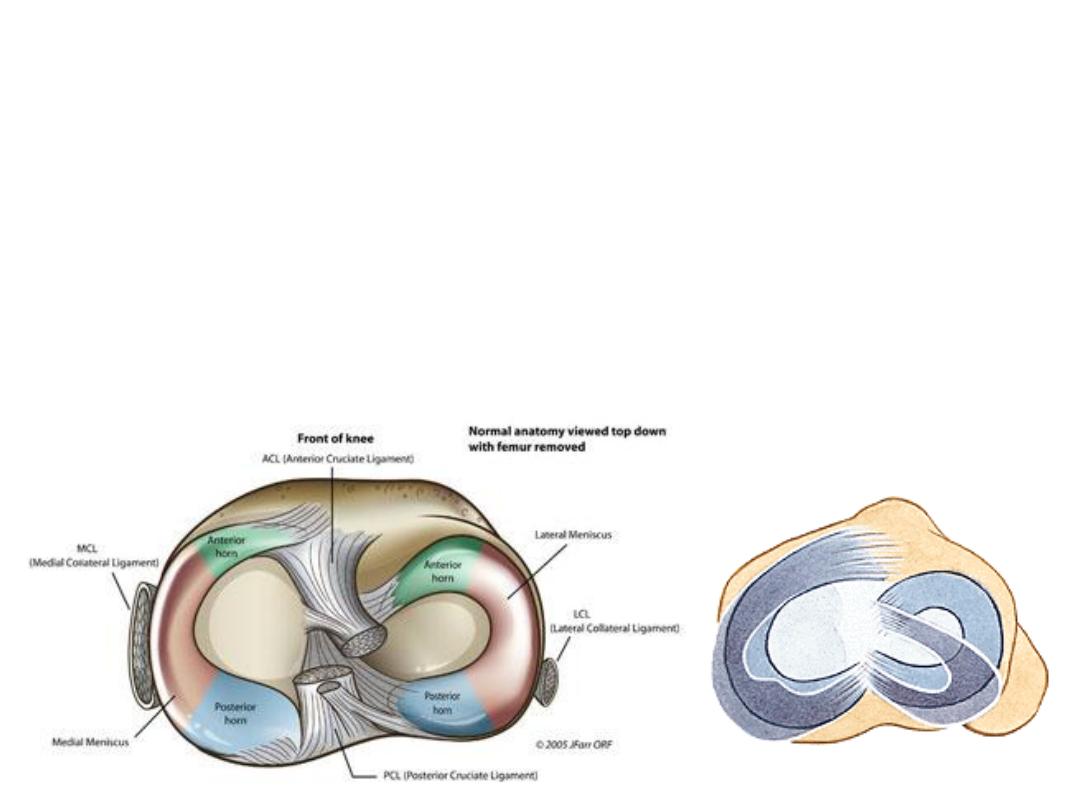
-MM is more liable to injury because it is fixed &
can’t be taken away
from the moving femoral condyles
-LM is less liable to injury because it is more mobile
-Factors which predispose to mobility of the LM are:
1- No attachment to knee capsule
2- Attachment to popliteus which draws it back.
3- The posteriorly sloping lateral tibial condyle.
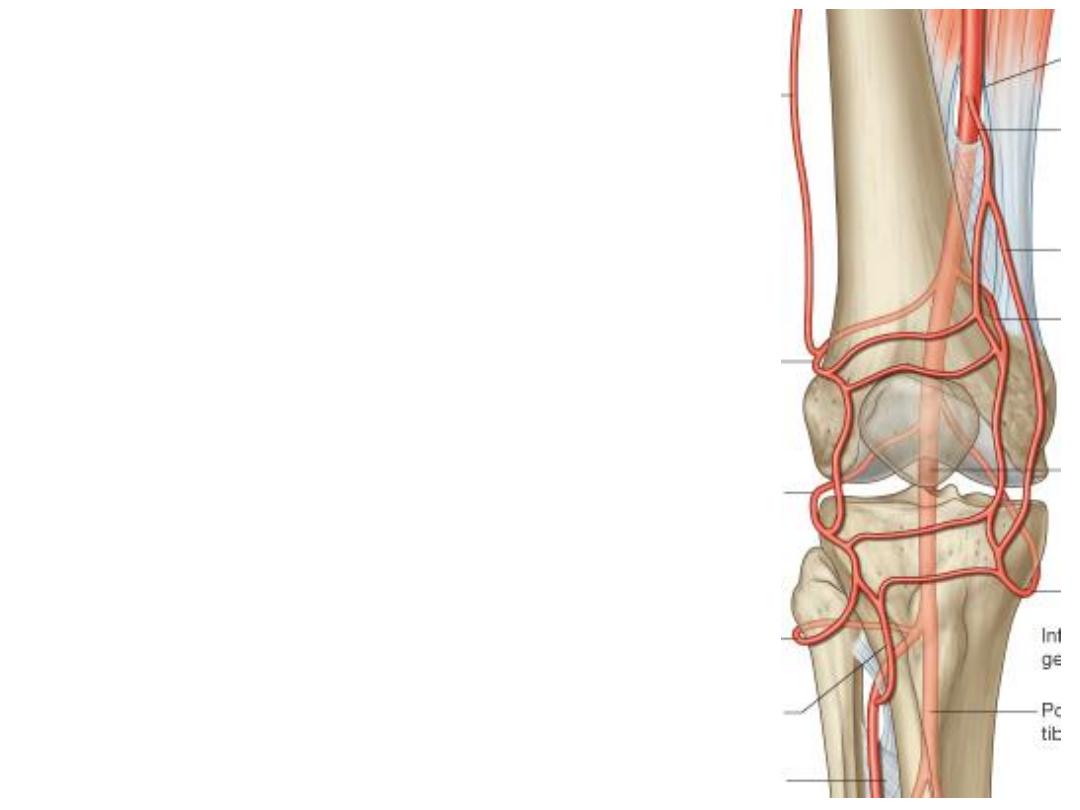
Vascular supply (anastomosis around the knee):
Ten arteries share in the formation of this anastomosis
which supplies the knee joint & surrounding
structures:
1) The genicular arteries
2) Descending branch of LFCA
3) Descending genicular artery
4) Fourth perforator artery
5) Anterior & posterior tibial recurrents
6) Circumflex fibular artery
-The knee joint is innervated by branches from the
obturator, femoral, tibial, and common fibular nerves.

Movements:
- Extension: Quadriceps femoris
- Flexion: Hamstrings, gracilis, sartorius and popliteus.
- Lateral rotation: Biceps femoris.
- Medial rotation: semimembranosus, semitendinosus, gracilis, sartorius
and popliteus.
Lateral and medial rotation can only occur when the knee is flexed (if the
knee is not flexed, the medial/lateral rotation occurs at the hip joint).
Proximal TF joint:
- An arthrodial (synovial) plane
joint between the lateral condyle
of the tibia and the head of the
fibula.
- The contiguous surfaces of the
bones present flat, oval facets
covered
with
cartilage
and
connected
together
by
an
articular capsule and by anterior
and posterior ligaments.
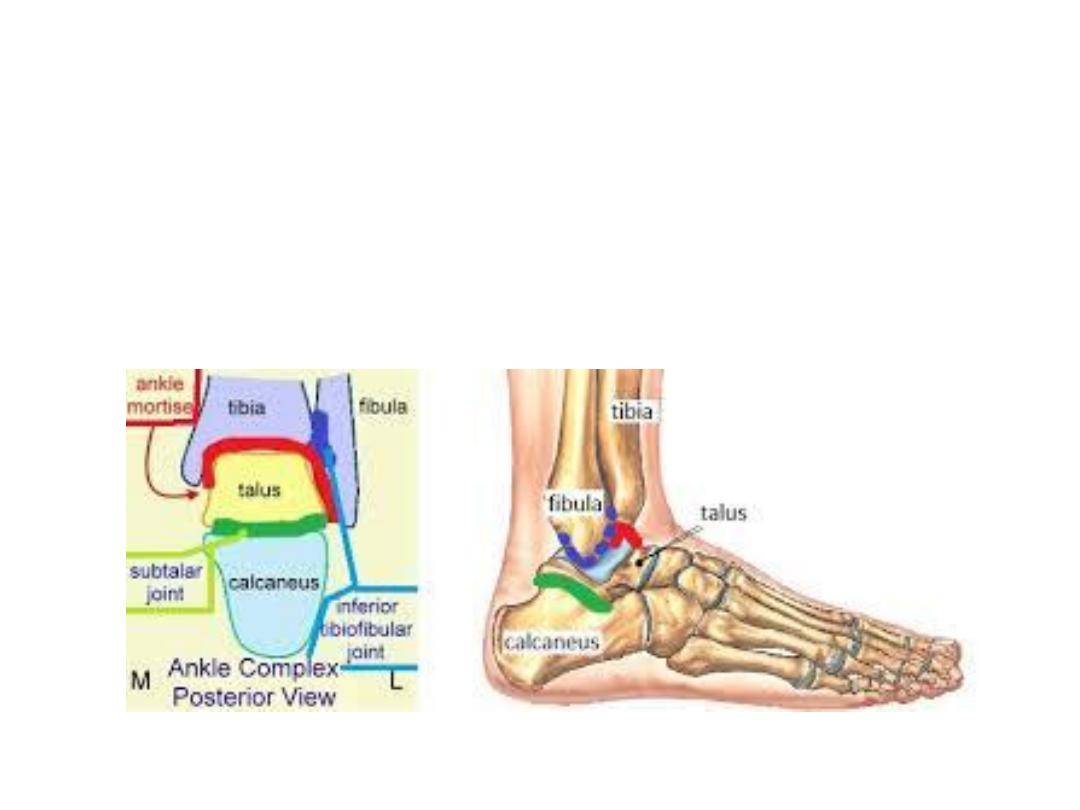
Ankle joint:
1- Ankle proper (Mortise joint, Talocrural joint)
2- Inferior tibiofibular
3- Subtalar
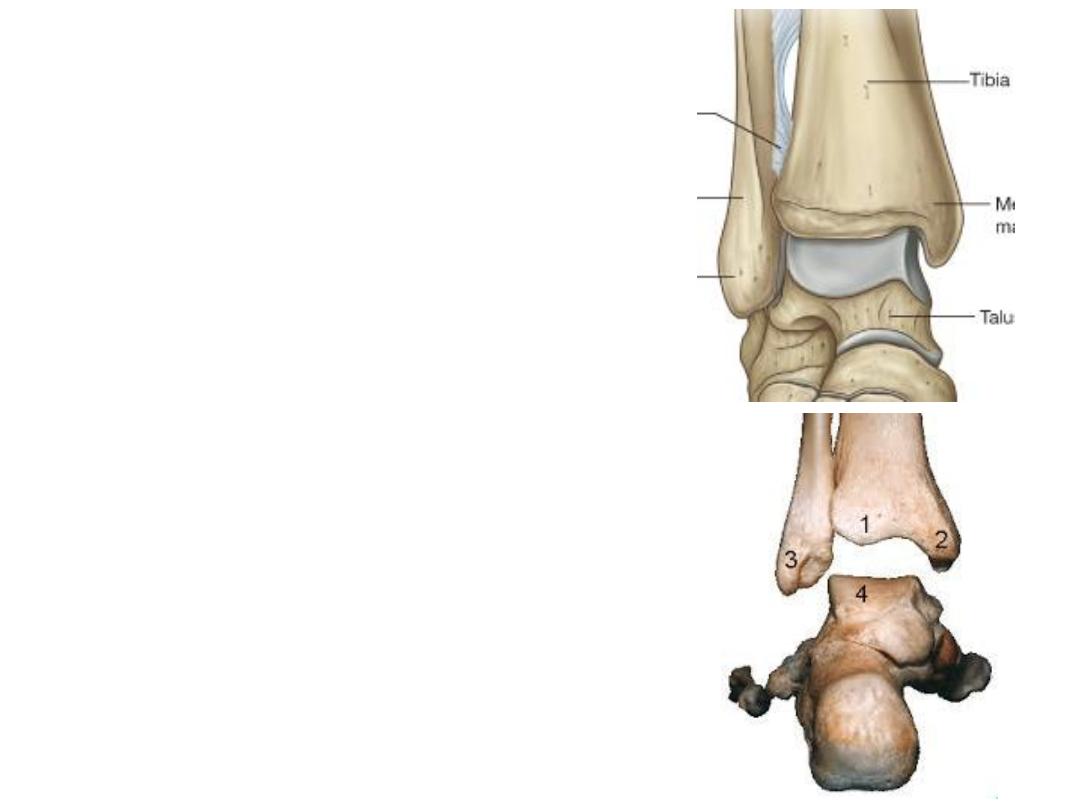
The ankle joint proper:
-The anchored distal ends of the fibula & tibia
create a deep bracket-shaped socket for the
upper expanded part of the body of the talus
-The roof of the socket is formed by the
inferior surface of the distal end of the tibia
-Medial & lateral sides are formed by the
corresponding malleoli
-The ankle joint is a hinge-like synovial joint
which involves the talus of the foot and the
tibia and fibula of the leg
-It mainly allows dorsiflexion & plantarflexion
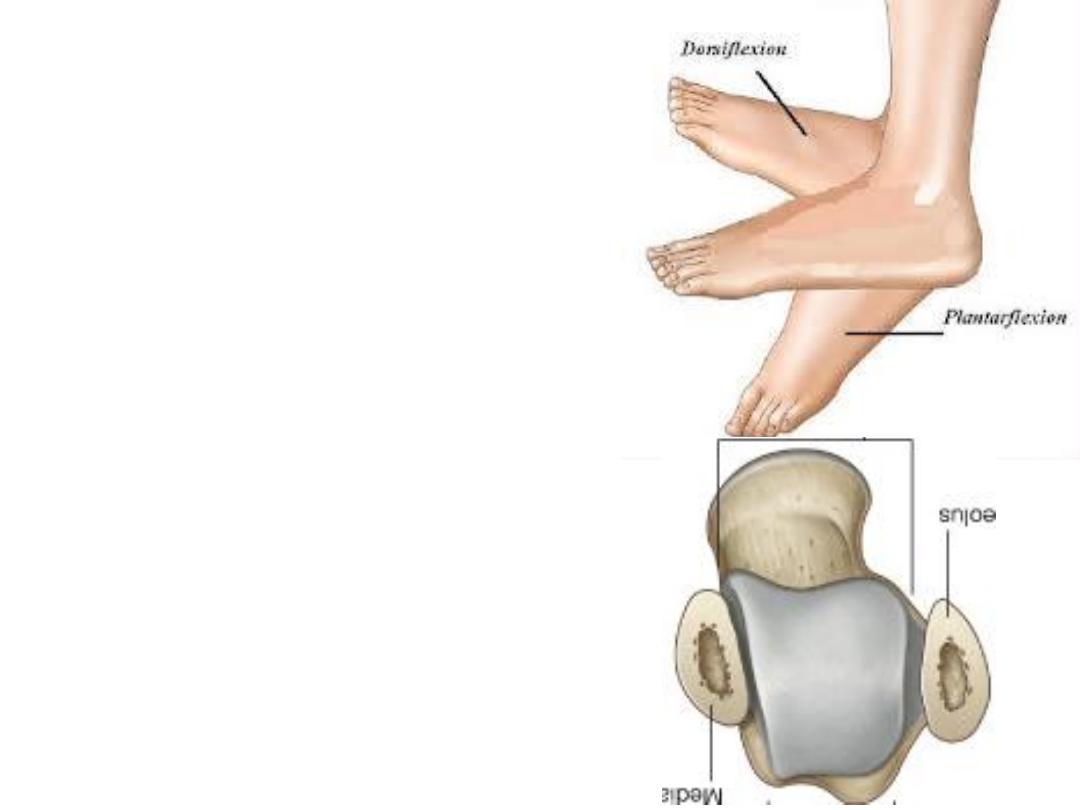
-When viewed from above, the articular
surface of the talus is much wider
anteriorly than it is posteriorly.
-As a result, the bone fits tighter into its
socket when the foot is dorsiflexed &
therefore most stable in this position.
-The articular cavity is enclosed by a
synovial membrane, which attaches
around the margins of the articular
surfaces & reflects on the inside of the
capsule.
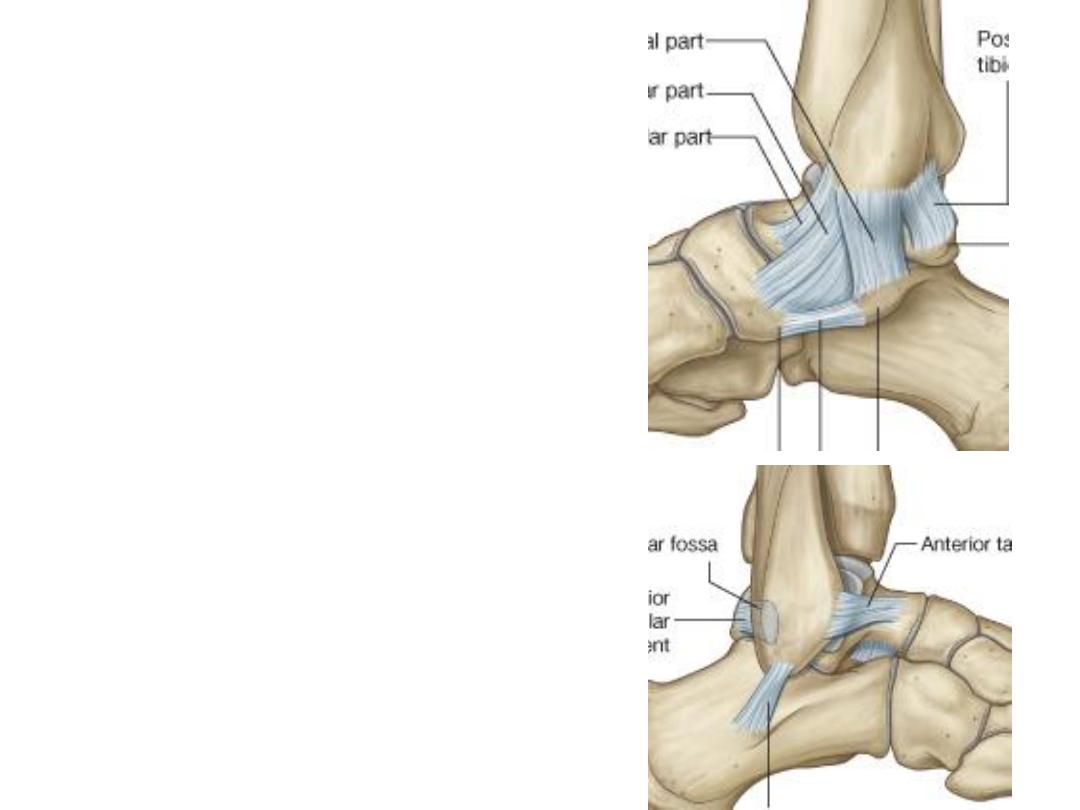
Medial (deltoid) ligament:
-A large, strong & triangular in shape.
Its apex is attached to the medial
malleolus and its broad base is
attached below.
Lateral ligament:
- The lateral ligament of the ankle is
composed of three separate ligaments,
anterior talofibular, posterior talofibular
& calcaneofibular ligaments.
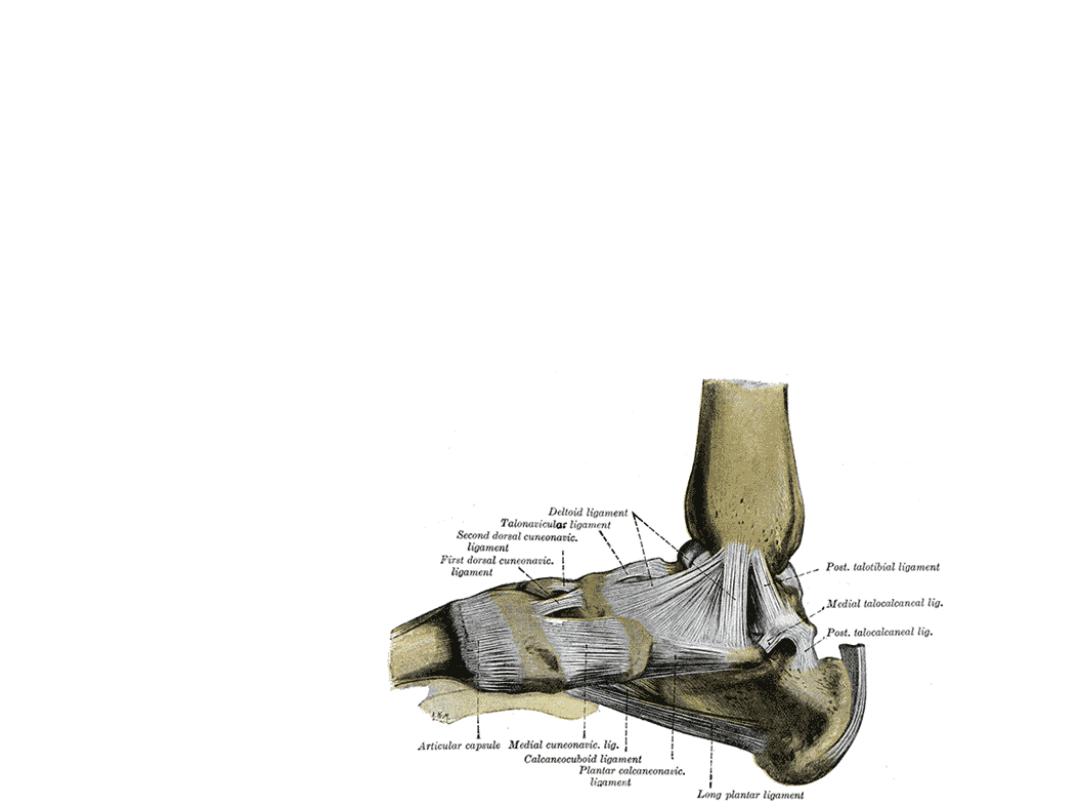
Subtalar joint:
• The talus is oriented slightly obliquely on the anterior surface of the
calcaneus.
• There are two points of articulation between the two bones, anterior &
posterior
• In both, the concavity on talus receives a convexity of calcaneus
• 4 talocalcaneal ligaments support the joint
• It is involved in inversion-eversion movement
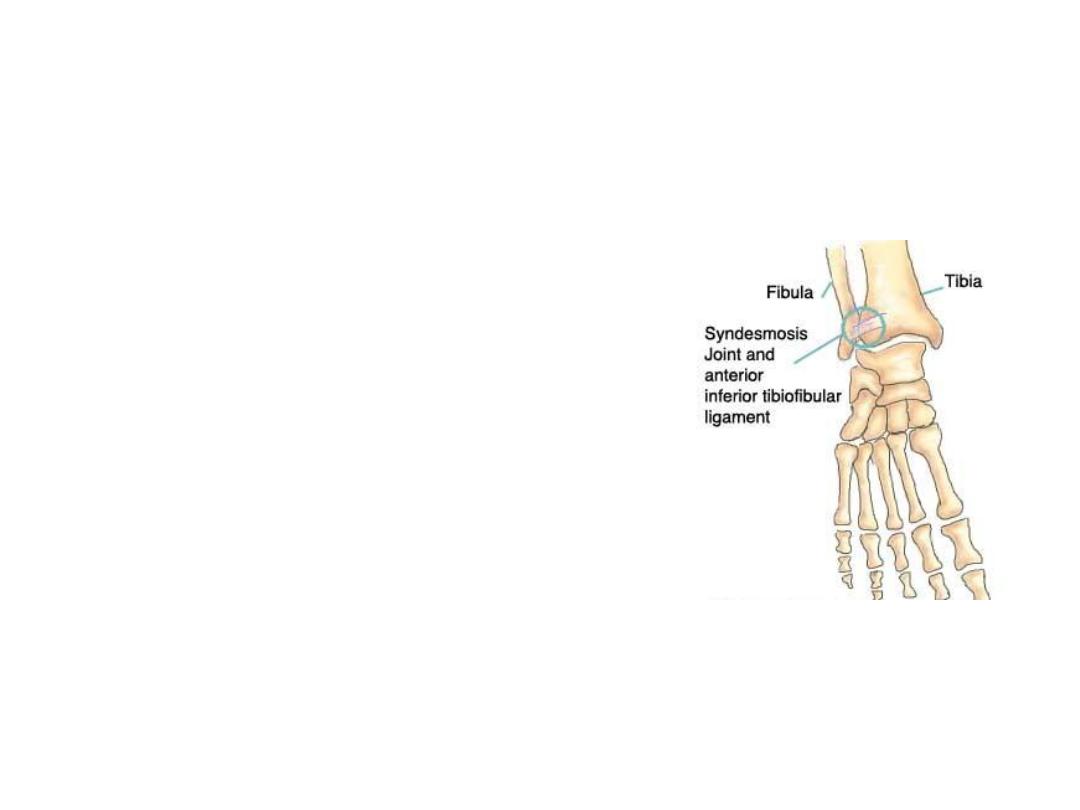
Tibiofibular joints:
Distal TF joint:
- Syndesmotic (fibrous) plane joint
- Formed by the rough, convex surface
of the medial side of the distal fibula
with the rough concave surface on the
lateral side of the tibia.
- These surfaces are smooth, and
covered with cartilage continuous with
that of the ankle-joint.
- The ligaments are:
Anterior ligament of the lateral malleolus
Posterior ligament of the lateral malleolus
Interosseous membrane of leg
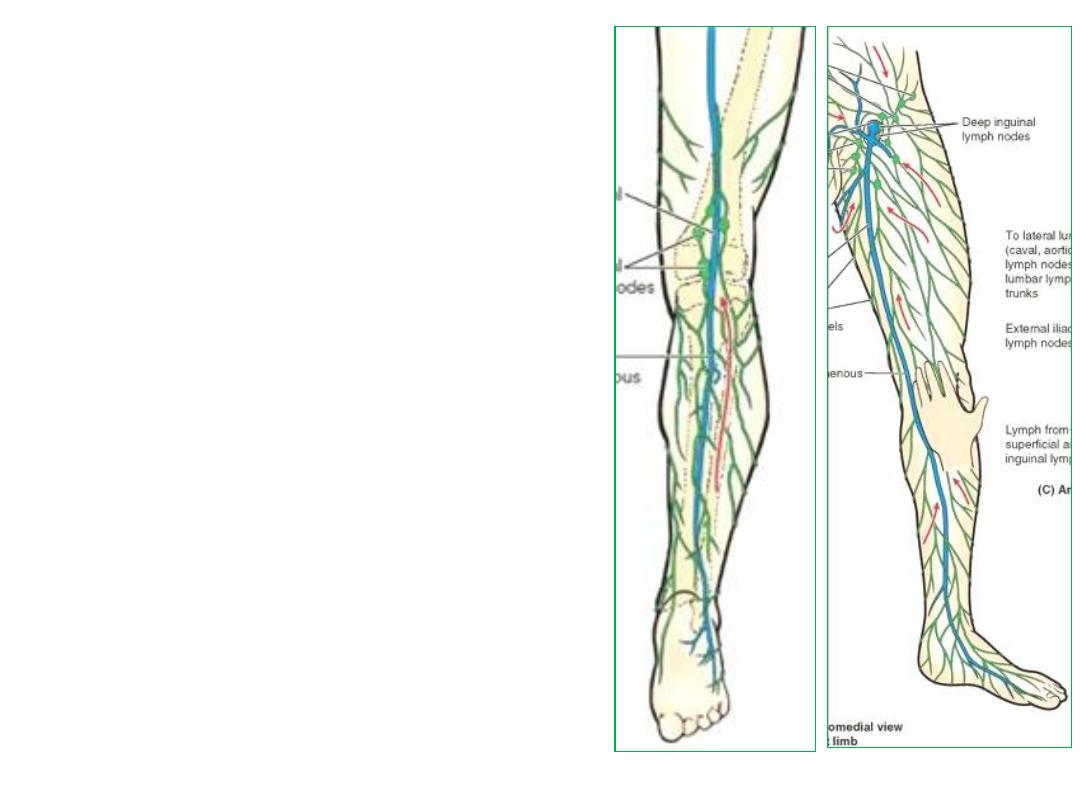
Lymphatic drainage of the lower limb:
-Superficial lymphatics drain everything
superficial to deep fascia & accompany
veins
-Deep
lymphatics
drain
deeper
structures & accompany arteries
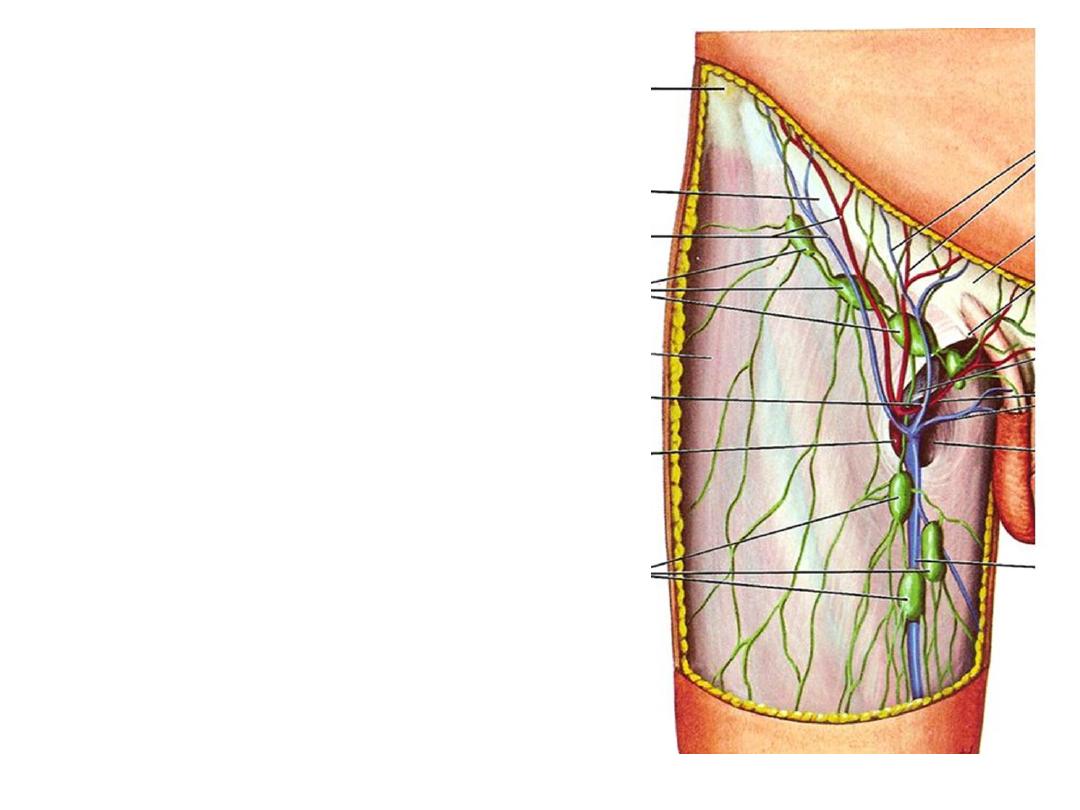
Superficial LN:
-The vertical group of superficial inguinal
LN
drains the lower limb & are arranged
around the termination of great saphenous
vein
(vs deltopectoral)
-Popliteal LN
drain the heel, lateral leg &
foor & arranged around the termination of
small saphenous vein
(vs supratrochlear)
Deep LN:
Deep inguinal node lies in the femoral canal
(vs axillary)
Superficial lymphatics
Accompany veins
Deep lymphatics
Accompany arteries
SILN
Vertical group
DILN
Superficial
Pop. LN
Structures
superficial to fascia
lata except lateral
foot, heel & back of
leg
From lateral foot,
heel & back of leg
Deep
Pop. LN
Along G saphenous v.
Along S saphenous v.
From deep
structures of the
lower limb
External iliac LN
Internal iliac LN
From gluteal
region
Along gluteal arteries
