13
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
Medical and dental emergencies and complications in
dental practice and its management
Access this article online
Quick Response Code:
Website:
www.jeed.in
DOI:
10.4103/0974-7761.115144
Introduction
An emergency is a medical condition that demands
immediate attention and successful management. These are
the life‑threatening situations of which every practitioner
must be aware of so that needless morbidity can be avoided.
A survey of 4000 dental surgeons conducted by Fast and
others revealed an incidence of 7.5% emergencies per dental
surgeon over a 10‑year period.
[1]
Emergencies can be prevented to a certain extent by a detailed
medical history, physical examination, and patient monitoring.
Preparation for an emergency and sound knowledge about the
management of all emergencies in general is of prime concern
to dental specialists.
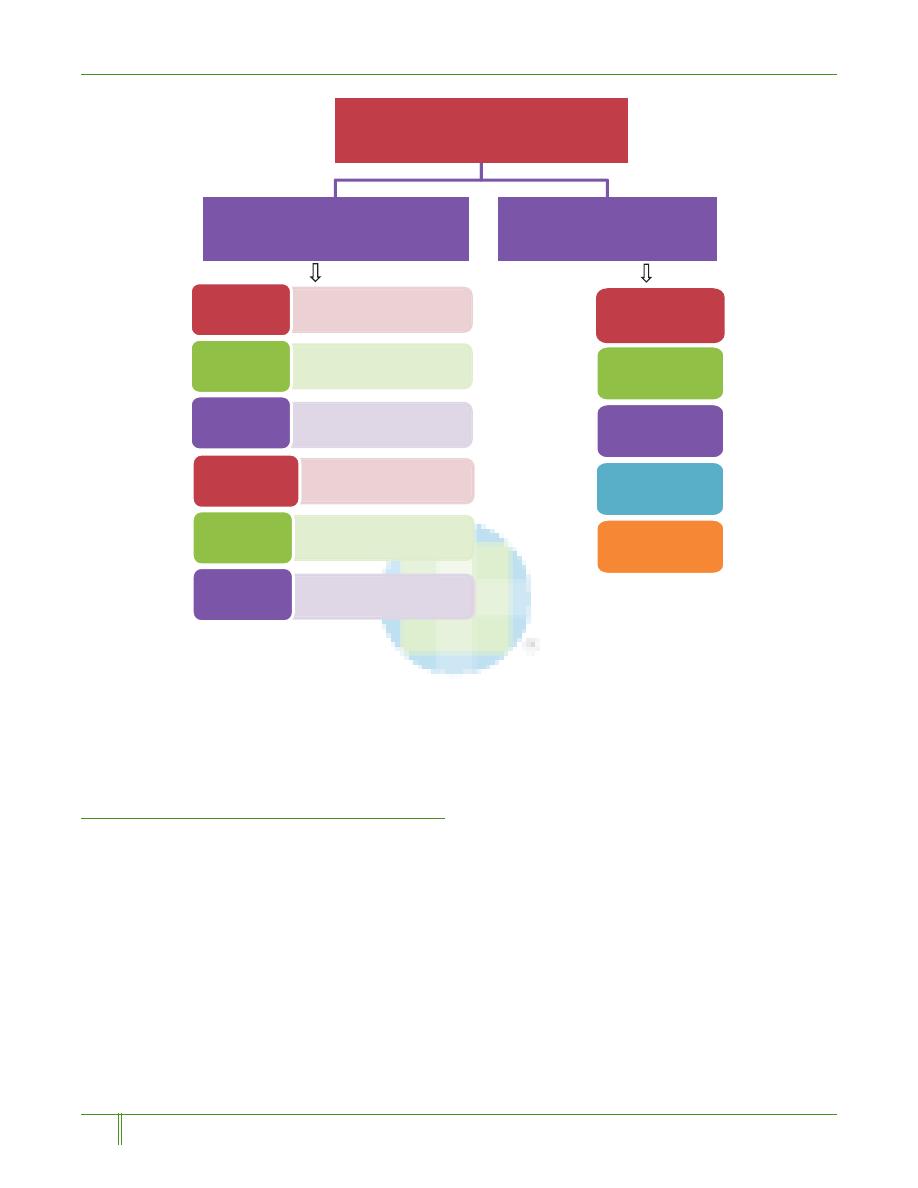
Basic principles of management of medical
emergencies
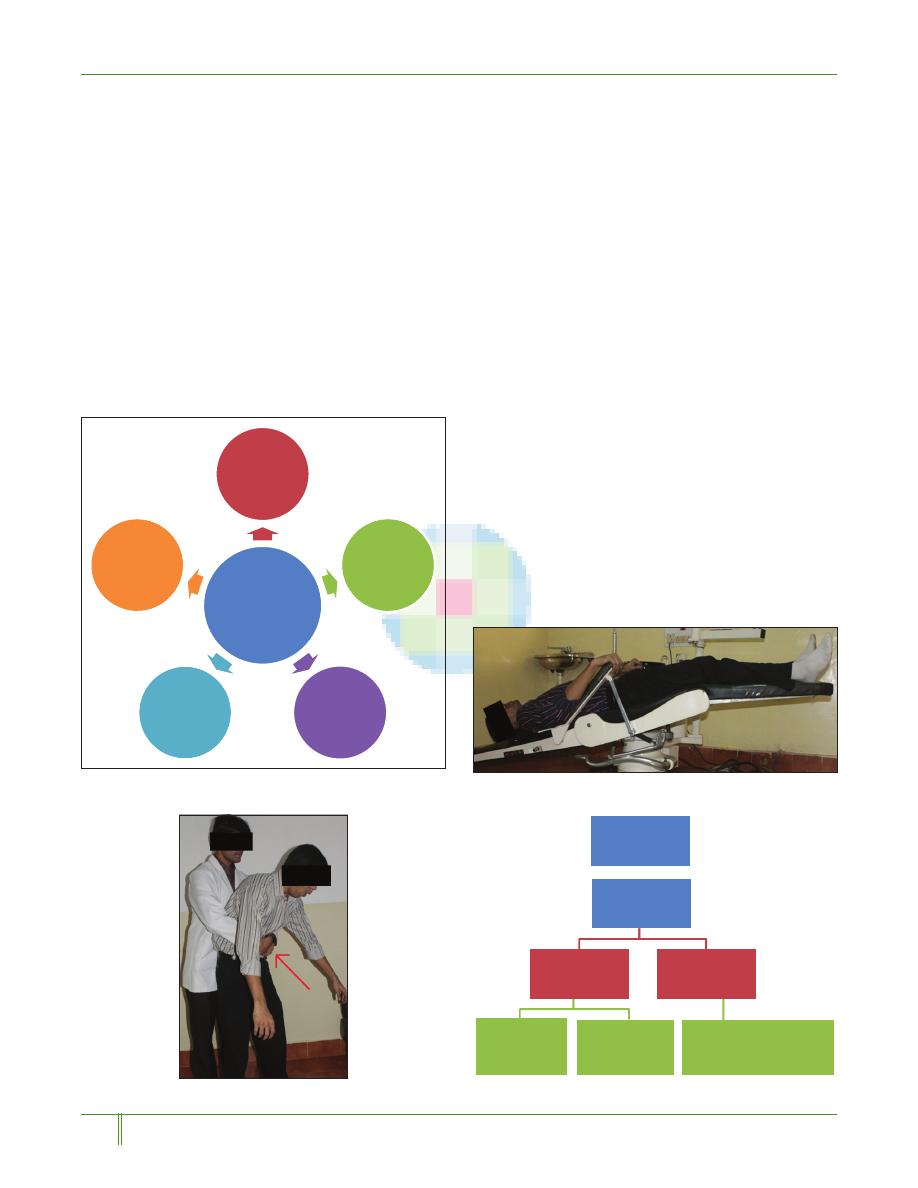
The golden rule in managing any emergency is rendering
basic life support (BLS) measures and cardiopulmonary
resuscitation (CPR). This is done by following the basic
principles: Position (P), Airway (A), Breathing (B),
Circulation (C), and Definitive therapy (D)
[2]
[Figure 1].
The primary positions to manage an emergency are
supine position, Trendelenburg position, and semi‑erect
position.
[3]
Maintaining a patent and functioning airway
is the first priority in managing an emergency. This is
achieved usually by the head tilt‑chin lift manoeuvre.
[4]
If
clear airway is still not achieved, then invasive procedures
like direct laryngoscopy and cricothyrotomy can be
followed. The next priority is to check for the presence
of adequate breathing which is assessed by the look‑feel
and listen technique.
[4]
If spontaneous breathing is not
evident then rescue breathing should be accomplished
immediately either by the mouth‑to‑mouth technique or
the bag‑valve‑mask technique. After establishing a patent
airway and breathing, circulation is assessed. The most rapid
and reliable method is by palpating the carotid pulse at the
region of the sternocleidomastoid muscle. If pulse is absent,
then CPR is initiated immediately. Once airway, breathing,
and circulation is maintained, definitive treatment is begun
if the emergency is acute and cause is clear to the dental
specialist. Definitive therapy involves administration of
drug when indicated and contacting for emergency care.
The medical and dental emergencies that are commonly
encountered in dental practice involve syncope, airway
obstruction, anaphylaxis, local anesthetic toxicity, asthmatic
attack, chest pain, hemorrhage, and seizure. Myocardial
infarction and cardiac arrest are extremely rare. Analysis of
history and patient counseling and motivation also play a role
in minimizing the emergencies.
Department of Prosthodontics and Crown and Bridge, A.B. Shetty Memorial Institute of Dental
Sciences (A constituent College of Nitte University), Deralakatte, Mangalore, Karnataka, India
ABSTRACT
Any dental professional can encounter an emergency during the course of their treatment.
Every Dental specialist should have the knowledge to identify and manage a potentially
life‑threatening situation. Prompt recognition and efficient management of an emergency
by the specialist results in a satisfactory outcome. Though rare, emergencies do occur in a
dental clinic. The ultimate goal in the management of all emergencies is the preservation of
life. The prime requisite in managing an emergency is maintenance of proper Position (P),
Airway (A), Breathing (B), Circulation (C), and Definitive treatment (D). The purpose of this
article is to provide a vision to the commonly occurring medical and dental emergencies and
complications in dental practice and their management. Data for the study was collected from
PubMed data base search.
Key words:
Anaphylaxis, asthmatic attack, complications, local anesthetic toxicity,
medical emergencies, syncope
Krishna D Prasad,
Chethan Hegde,
Harshitha Alva, Manoj Shetty
Address for correspondence:
Dr. Harshitha Alva,
Department of Prosthodontics
and Crown and Bridge,
A.B Shetty Memorial Institute
of Dental Sciences, Mangalore,
Karnataka - 575 018, India.
E-mail: drharshitha@gmail.com
Review
Article
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
14
Prasad, et al.: Emergencies, complications and their management
Syncope
Syncope is caused due to inadequate cerebral perfusion.
Causes of sudden loss of consciousness and collapse include
hypotension, adrenal crisis, anaphylaxis, cardiac arrest,
diabetic collapse, hypoglycemia, epileptic seizure, fainting,
or stroke.
[5]
The early manifestations include nausea, warmth,
perspiration, baseline blood pressure, and tachycardia. Late
manifestations include hypotension, bradycardia, pupillary
dilation, peripheral coldness, and visual disturbance. Most
of the syncopal attacks can be prevented by ensuring that
the patient has had their meal before treatment in case of
systemic diseases like diabetes and also making the patient lie
in the supine position before administering local anesthetics.
[5]
Management: The patient should be in the supine position
[Figure 2]. Recovery is almost instantaneous if the patient has
simply fainted. Then maintain airway, check pulse (if absent,
indicates cardiac arrest), and start CPR immediately. If pulse is
palpable and the patient has not completely lost consciousness,
four sugar lumps may be given orally or intravenous 20 ml of
20‑50% sterile glucose. A hypoglycemic patient will improve
with this regimen. But if there is still no improvement medical
assistance should be summoned. Meantime, hydrocortisone
sodium succinate 200 mg IV should be given.
[5]
Airway obstruction
Airway obstruction is usually caused due to accidental slippage,
aspiration of foreign objects, or laryngeal spasm. Patient
manifests with inability to speak, grasps the throat (universal
sign), coughs, inability to exchange air (in spite of respiratory
movements), cyanosis, and loss of consciousness. These might
eventually lead to cardiac arrest finally.
Management: Main priority is to clear the airway, but the
method differs depending upon whether the patient is
conscious or unconscious. If the patient is conscious, then
he/she must be made to sit straight, support chest with one
hand, and deliver five sharp back blows between the shoulder
blades with the heel of the other hand. But if the patient is
choking, an attempt is made to expel the object with upward
thrusts using Heimlich thrust [Figure 3]. It acts as artificial
cough that produces a rapid increase in intra‑thoracic pressure
thus helping to expel the foreign body [Figure 4].
In an unconscious patient: The patient is got to a supine
position and deliver inward and upward thrust five times.
&LU
'HILQLWLYH
7KHUDS\
3
P
FXODWLRQ
3ULQFLSOHVRI
HPHUJHQF\
PDQDJHPHQW
3RVLWLRQ
%UHDWKLQJ
$LUZD\
Figure 1: Principles of emergency management
Figure 2: Syncope management : Trendelenburg Position
Figure 3: Heimlich Thrust
$VVHVVVHYHULW\
6HYHUHDLUZD\
REVWUXFWLRQ
,QHIIHFWLYHFRXJK
8QFRQVFLRXV
6WDUW&35
&RQVFLRXV
EDFNEORZV
DEGRPLQDOWKUXVWV
0LOGDLUZD\
2EVWUXFWLRQ
(IIHFWLYHFRXJK
(QFRXUDJH&RXJK
&RQWLQXHWRFKHFNIRU
GHWHULRUDWLRQWRLQHIIHFWLYH
FRXJKRUUHOLHIIURPREVWUXFWLRQ
$LUZD\REVWUXFWLRQ
Figure 4: Airway obstruction management
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
15
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
Prasad, et al.: Emergencies, complications and their management
This thrust is followed by turning patient to one side to clear
oral cavity. Attempt to re‑ventilate, commence CPR and
administer oxygen
.
If the foreign object is still not dislodged
and patient’s condition deteriorates, then a surgical airway is
created by Laryngoscopy or cricothyrotomy.
[5]
A 10‑year institutional review on aspiration and ingestion in
dental practice concluded that dental procedures involving
single‑tooth cast or prefabricated restorations involving
cementation have a higher likelihood of aspiration. This can
be prevented by measures such as use of rubber dams or
gauze, throat screens, or floss ligatures.
[6]
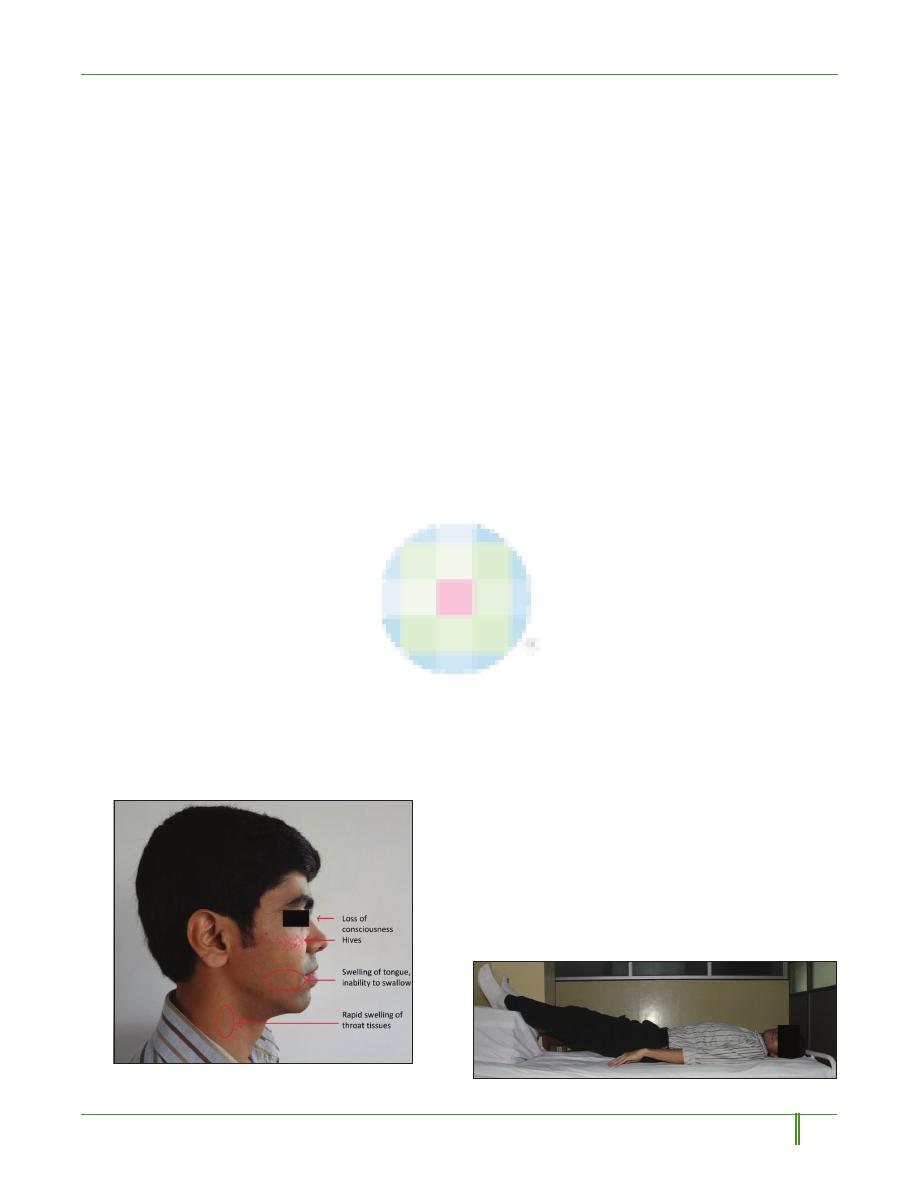
Anaphylaxis
It is a hypersensitive state that results from exposure to
an allergen. The most common allergen in a dental setup
is latex.
[2]
Manifestations vary from a mild form where the
patient presents with erythematous rash, cyanosis, nausea,
vomiting, tachycardia, utricaria, or angiodema to a severe
form which leads to airway obstruction or inadequate blood
pressure and blood flow to the brain which is a life‑threatening
situation [Figure 5]. Management involves lying the patient
in the supine position with legs raised [Figure 6], administer
oxygen, and the drug of choice being 0.5 ml of 1:1000
adrenaline IM or SC.
[5]
Local anesthetic toxicity
Local anesthetics are the most commonly used drugs in
dentistry. Toxicity is usually either due to the local anesthetic
itself or the vasoconstrictor which can be due to rapid infusion
or failure to aspirate before injection. Generally, the reactions
are self limiting. Toxicity presents with talkativeness, slurred
speech, anxiety, confusion, drowsiness, or even seizure and
cardiac arrhythmias in extreme cases.
Management: Sessate the administration of injection and
monitor vital signs. Administer oxygen and in adverse cases
administration of diazepam 5 mg slowly is advised.
[5]
Asthmatic attack
Anxiety, infection, exposure to an allergen or drugs can
precipitate an asthmic attack. The goal of management during
an acute asthmatic episode on a dental chair should be to
relieve the bronchospasm associated with the attack. Patient
presents with thickness or heaviness in the chest, difficulty
in breathing, spasmodic and unproductive cough, expiratory
wheeze, and anxious behavior. Hence, the patient should
primarily be relieved of irritants and all articles should be
removed from oral cavity.
[5]
Drug of choice is 2 puffs of albuterol. If no improvement is
seen in 15 seconds then administer 1:1000 adrenaline 0.5 ml
SC/IM and if still no response is observed in 2‑3 min then
salbutamol slow IV injection is advised.
[5]
Chest pain
Factors that precipitate chest pain include angina, acute
myocardial infarction, gastrointestinal reflux disease, anxiety,
costochondritis and paroxysmal supraventricular tachycardia.
[2]
Patients generally present with tightness, fullness, constriction,
or heavy weight on the chest. Angina pectoris and acute
myocardial infarction (AMI) are the two commonly occurring
cardiac problems in a conscious patient. Patient’s history is of
prime concern here. If this is the first time patient has ever
experienced a chest pain, then dental specialist should treat
him or her as if it were an acute myocardial infarction and
have emergency medical service transfer immediately. If not
then it is an angina pectoris situation.
Quality of pain can also indicate whether the patient is having
an angina or acute myocardial infarction. In angina pectoris
pain is significant but not severe whereas an acute myocardial
infarction pain generally radiates to left side of the body‑left
shoulder, left mandible, left arm.
[2]
Management: For angina pectoris, drug of choice is a nitrate,
commonly nitroglycerine, sublingual tablet, translingual or
transmucosal spray. Management of a patient with suspected
acute myocardial infarction involves administration of
morphine, oxygen, nitroglycerine, and aspirin (MONA)
in addition to emergency medical service. If morphine is
unavailable, the specialist can also substitute nitrous oxide/
oxygen in a 50:50 concentration.
[2]
Haemorrhage
Haemorrhagic disorders, though uncommon, should always
Figure 5: Schematic representation of the areas to be observed
for signs and symptoms of Anaphylaxis
Figure 6: Management of anaphylaxis
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]

Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
16
Prasad, et al.: Emergencies, complications and their management
be considered, as dental specialists deal with blood routinely
and there are instances when significant bleeding could lead
into an emergency. Emergency management begins by gently
cleaning the mouth and locating the source of bleeding and
the application of cold compress, pressure packs, or styptics.
Suture the area under L.A when necessary. Tranexamic
acid –500 mg in 5 ml by slow IV injection is the drug of
choice.
[2,5]
Seizures
Patients who convulse in dental office generally have a seizure
history and are often characterized as having epilepsy.
Management: If the patients experiencing seizure is
unconscious, they should primarily be placed in the supine
position and the head tilt‑chin lift manoeuvre is performed.
Dental specialist should remove all instruments from patient’s
mouth and protect the patient. Clear airway, loosen clothing
and help patient breath adequately.
If seizure continues for long, then the condition is known
as status epilepticus. This is a life‑threatening emergency
and is best managed with I.V. diazepam 5 mg IV/IM or
by maintaining BLS till patient is shifted to emergency
medical care.
Dental Complications
More than dental emergencies which require an immediate
attention and management, the occurrence of “complications”
are of higher incidence in dental practice. The complications
may be immediate or delayed and are related to patient’s
tolerance level, materials used and treatment procedures.
In an interdisciplinary dental practice the most common
complication is aspiration. Aspiration may be of the denture
as a whole or a fractured part, a minimal extension acrylic
removable prosthesis, crowns during removal, instrument
slippage especially broaches reamers or files. Aspiration causes
airway obstruction which is manifested as the universal sign
“choking.” Removal of broken instruments is performed using
ultrasonics, operating microscopes or microtube delivery
methods.
[7]
Allergy is another complication commonly encountered by a
dental specialist.
Allergy can be to latex, mercury, rubber dam, and impression
material. Manifestations of allergy include pruritis, erythema,
utricaria, and angioneurotic edema. Minimizing latex exposure
is most effective when treating latex‑sensitive patients. Latex
alternatives (vinyl, nitrite, or silicone) and powder‑free
gloves should be used to prevent sensitization. Fixers like
formacresol and devitalizers to be used carefully to prevent
chemical burns. Allergy to alloys like nickel–chromium and
chromium–cobalt has also been encountered.
Complications involving local anaesthetics are hypersensitivity,
toxic reactions, and allergy.
[8]
The most severe form of
hypersensitivity is anaphylaxis which is a life‑threatening
generalized or systemic reaction.
[9]
Anaphylaxis can be either
allergic or non‑allergic. Allergic hypersensitivity can be
immediate due to IgE or delayed which is T‑cell mediated.
[10]
Management
involves
administering
prophylactic
antihistamines, such as diphenhydramine or corticosteroids
such as prednisone before dental treatment to those at known
risk
[8,9]
and the drug of choice is 0.3‑0.5 ml intra‑muscular or
subcutaneous doses of 1:1000 epinephrine.
[10]
Allergic reactions can also occur to acrylic resins, which can
be minimized by following proper monomer polymer ratio,
correct curing cycle so as to minimize the residual monomer
content in the prosthesis.
Interference of a cardiac pacemaker by an electronic dental
device was studied by Roedig et al. The pacing activity of
both pacemakers and the dual‑chamber ICD was inhibited by
a battery‑operated composite curing light at between 2 and
10 cm from the leads. The use of an ultrasonic scaler interfered
with the pacing activity of the dual‑chamber pacemaker
between 17 and 23 cm from the leads, the single‑chamber
pacemaker at 15 cm from the leads and both ICDs at
7 cm from the leads. Operation of the electric toothbrush,
electrosurgical unit, electric pulp tester, high‑ and low‑speed
handpiece, and an amalgamator did not alter pacing function.
The article concluded that the use of the ultrasonic scaler,
ultrasonic cleaning system, and battery‑operated composite
curing light may produce deleterious effects in patients who
have pacemakers or ICDs.
[11]
An immediate complication usually manifested during an
endodontic therapy is hypochlorite accident wherein sodium
hypochlorite is expressed beyond the apex and patients
manifests with severe pain, swelling or profuse bleeding.
Immediate management involves administration of a regional
block and then wait till maximum drainage occurs.
Antibiotics: Penicillin 500 mg five times a day for 7 days is
prescribed.
Complications and emergencies encountered during
implant therapy
Complications can be either related to the surgery or implant
placement. The intra‑operative complications related to
surgery are haemorrhages, neurosensory alteration, damage to
the adjacent teeth, and mandibular fractures.
[12]
Haemorrhages in the mandible most frequently occur in the
intra‑foraminal region by damage to the descending palatine
artery or the posterior palatine artery. Respiratory obstruction
has also been reported due to perforation of the arteries
supplying the mandible.
[13]
This is believed to be due to the
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
17
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
Prasad, et al.: Emergencies, complications and their management
massive internal haemorrhage caused due to the vascular injury
in the floor of the mouth which creates a swelling, producing
protrusion, and displacement of the tongue, thus obstructing
the airway.
[14,15]
Haemorrhages can be managed by strong
finger pressure at the point of bleeding but if compressions
don’t obtund bleeding then at times anastomoses necessitates
ligation.
[12]
Another complication related to surgery is
neurosensory disturbance which manifests as anaesthesia,
paresthesia, hypoesthesia, or dysesthesia. If the patient suffers
from paresthesia but implant is placed correctly with no
damage to the nerve, then retrieval of implant is not advised;
instead wait for recovery. However, if the nerve is being
compressed, it is always advisable to remove the implant to
avoid permanent neural damage.
[16]
Damage to the adjacent
teeth occurs due to lack of parallelism of the implant with the
adjacent teeth. Hence, it is always mandatory that a distance
of 1.5 mm be maintained from the adjacent teeth.
In case of damage, treatment of the affected teeth include
endodontic therapy, periapical surgery, apicectomy, or
extraction.
[17]
Mandibular fractures are rare and occur when
implants are placed in atrophic mandible.
Complication associated with implant placement most
importantly involves loss of primary stability which can be
attributed to overworking of the implant bed, poor bone
quality or use of short implants.
[12]
An increase in temperature
due to excessive speed of the drill produces necrosis, fibrosis,
osteolytic degeneration, and increased osteoclastic activity.
[18]
Loss of primary stability can be managed by using a wider and
longer self‑tapping implant.
[19]
Another possible complication
is manifestation of dehiscence or fenestration, managing
which involves filling the bone defect with bone grafts and
resorbable or non‑resorbable membranes.
[20]
During implant
placement in the maxilla in areas close to sinus or during sinus
lift procedures, complications involving rupture of Schneider
membrane can occur. Depending on the width of the tear, a
resorbable membrane may be used which serves to contain
the bone graft material, or if the tear is very wide, then surgery
is postponed.
Another complication is the displacement of the implants into
the maxillary sinus during the surgery or in the postoperative
period. In some cases, it can lead to sinusitis or even remain
asymptomatic.
These emergencies and complications can be minimized
by appropriate pre‑surgical planning, use of accurate
surgical techniques, postsurgical follow‑up, respecting
the osseointegration period, appropriate design of the
superstructure, biomechanics, and advocating meticulous
hygiene during the maintenance phase.
Recent advances in the management of emergencies
The most recent advancement is the revised CPR guideline
by the American Heart Association (AHA) in 2010. Instead
of ABC, now compressions come first only then do airway
and breathing.
Initially, it was believed that the chest compressions should
be at least 1‑1.5 inches deep but now at least 2 inch deep
compressions are recommended and also instead of pushing
on the chest at about 100 compressions per minute, AHA
now recommends to push at least 100 compressions per
minute.
[21]
Discussion
As always believed, prevention is the best medicine. Hence,
being prepared for an emergency and believing that emergency
is a real possibility in a dental clinic is of utmost importance.
Preparation for emergencies involves personal, staff, and office
preparation wherein personal and staff preparation include
an in depth knowledge of signs, symptoms, and management
of emergencies, basic life support (BLS) measures, and
cardiopulmonary resuscitation (CPR). Office preparation
involves maintaining emergency equipment, emergency
drugs, and backup medical assistance.
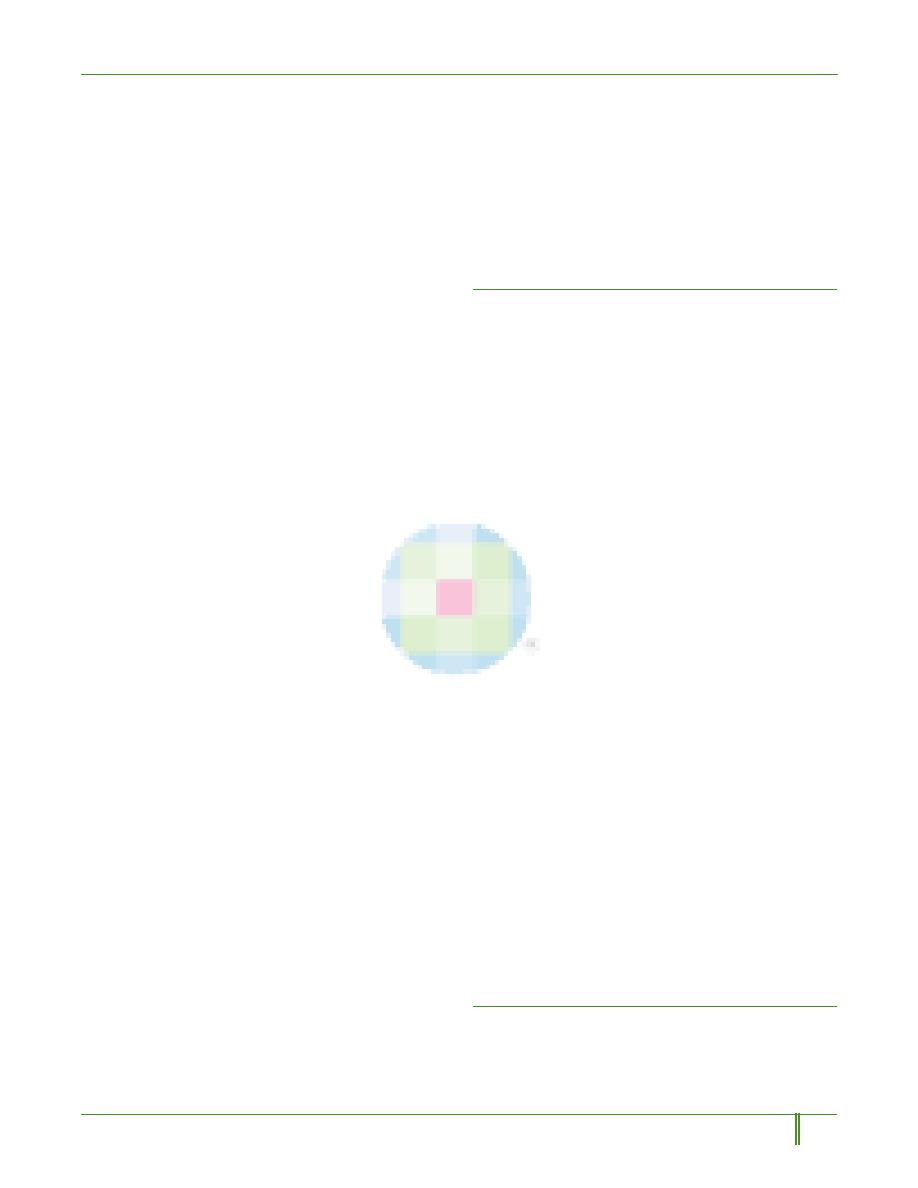
Whenever an emergency has been recognized, most
important is to follow DRS‑ABC Emergency equipments
that are indispensible in a dental set‑up involve a dental chair
which can be readily adjusted to Trendelenburg position, high
volume suction to clear oral secretions, disposable needle and
syringe, oxygen cylinder with face mask and AMBU bag, and
maintenance of IV access. Dental specialist should always
remember that administration of drugs is not necessary for
management of an emergencies and primary management
always involves BLS measures.
Emergency kit should comprise of airway accessories and
pharmacological agents
[1,22]
[Figure 7].
In case of referral dental practice, any positive observations by
the specialist may be shared while referring to another specialist
for the necessary precautions using a medical alert note. The
patient should be psychologically motivated and prepared to
face the emergency situation if arises before commencement
of treatment procedures. The dental specialist should also be
prepared to face any kind of emergencies which could arise
suddenly during treatment any procedure.
“Complications” may be immediate or delayed. They may not
be life threatening but always require attention and proper
protocols to be followed for effective management.
Conclusion
Emergencies cannot be totally prevented but can be managed
appropriately with thorough knowledge of the signs, symptoms,
and accurate treatment of the emergencies. Accomplishing this
depends on the combined effort of the dental specialist, staff,
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
18
Prasad, et al.: Emergencies, complications and their management
and immediate availability of the critical drugs and equipments
for the procedure. However, no drug can replace an efficiently
trained health care professional in managing an emergency but
an emergency drug kit and equipment does play an integral
role in the course and outcome of management of emergencies
and complications in interdisciplinary dental practice.
References
1. Morrison AD, Goodday RH. Preparing for medical emergencies in
dental office. J Can Dent Assoc 1999;65:284‑6.
2. Reed KL. Basic management of medical emergencies: Recognizing a
patient’s distress. J Am Dent Assoc 2010;141 Suppl 1:20S‑24.
3. Malamed SF. Medical Emergencies in the Dental Office. 6
th
ed.
St. Louis: Mosby; 2007. p. 51‑92.
4. Medical emergencies and resuscitation: Standards for clinical practice
and training for dental practitioners and dental care professionals
in general dental practice. A statement from the Resuscitation
council (UK) July 2006;revised May 2008.
5. Emergencies. In: Scully C.,Cawson RA. Medical Problems in dentistry.
5th ed. 2005 .563‑70.
6. Tiwana KK, Mortan T, Tiwana PS. Aspiration and ingestion in dental
practice. J Am Dent Assoc 2004;35:1287‑91.
7. Gencoglu N, Helvacioglu D. Comparison of the different techniques
to remove fractured endodontic instruments from root canal systems.
Eur J Dent 2009;3:90‑5.
8. Grzanka A, Misio
łek H, Filipowska A, Miśkiewicz‑Orczyk K,
Jarz
ąb J. Adverse effects of local anaesthetic allergy, toxic reactions
or hypersensitivity. Anaesthesiol Intens Ther 2010;42:175‑8.
9. Johansson SG, Hourihane JO, Bousquet J, Bruijnzeel‑Koomen C,
Dreborg S, Haahtela T, et al. A revised nomenclature for allergy. an
EAACI position statement from the EAACI nomenclature task force.
Allergy 2001;56:813‑24.
10. Thyssen JP, Menné T, Elberling J, Plaschke P, Johansen JD.
Hypersensitivity to local anaesthetics – update and proposal of
evaluation algorithm. Contact Dermatitis 2008;59:69‑78.
11. Roedig JJ, Shah J, Elayi CS, Miller CS. Interference of cardiac pacemaker
and implantable cardioverter‑defibrillator activity during electronic
dental devices use. J Am Dent Assoc 2010;141:521‑6.
12. Lamas Pelayo J, Peñarrocha Diago M, Martí Bowen E, Peñarrocha
Diago M. Intraoperative complications during oral implantology. Med
Oral Patol Oral Cir Bucal 2008;13:E239‑43.
13. Flanagan D. Important arterial supply of the mandible, control of an
arterial hemorrhage, and report of a hemorrhagic incident. J Oral
Implantol 2003;29:165‑73.
14. Niamtu J 3
rd
. Near fatal airway obstruction after routine implant
placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
2001;92:597‑600.
15. Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous
implant placement in the anterior mandible: A review of the literature.
J Periodontol 2004;75:631‑45.
16. Guarinos J, Peñarrocha M, Donado A. Complicaciones y fracasos. In:
Peñarrocha M, editor. Implantología oral. Barcelona: Ars Médica;
2001. p. 245‑56.
(PHUJHQF\NLWFRPSRQHQWV
3KDUPDFRORJLFDODJHQWV
$LUZD\DFFHVVRULHV
ORDGHGLQD
V\ULQJH
(SLQHSKULQH
'LSKHQK\GUDPLQHRU
&KORUSKHQ\UDPLQH
0DOHDWH
$QWLKLVWDPLQH
'LD]HSDP
$QWLFRQYXOVDQW
'H[WURVH
*OXFDJRQ*OXFRVH
6XJDU
$QWLK\SRJ\OFHPLF
0RUSKLQHIRU0,
$QDOJHVLF
/LJQRFDLQH$WURSLQH
6DOEXWDPRO,QKDORU
2WKHUV
2[\JHQFRQFHQWUDWRU
6HWRIRURSKDU\QJHDO
DQGQDVRSKDU\QJHDO
DLUZD\V
1DVDO&DQXOD
)DFHPDVN
$0%8%$*
Figure 7: Emergency Kit Components
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
19
Journal of Education and Ethics in Dentistry
January-June 2012 • Vol. 2 • Issue 1
Prasad, et al.: Emergencies, complications and their management
17. Kim SG. Implant‑related damage to an adjacent tooth: A case report.
Implant Dent 2000;9:278‑80.
18. Tehemar SH. Factors affecting heat generation during implant
site preparation: A review of biologic observations and future
considerations. Int J Oral Maxillofac Implants 1999;14:127‑36.
19. Guisado B. Complicaciones y fracasos en implantología. In:
Bascones A, editor. Tratado de odontología. Tomo IV. Madrid:
Smithkline Beecham; 1998. p. 3877‑86.
20. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical
complications with implants and implant prostheses. J Prosthet Dent
2003;90:121‑32.
21. Available from: http://firstaid.about.com/od/cpr/qt/09_2010_CPR_
Guidelines.htm [Last accessed on 12.12.2011].
22. ADA Council on Scientific Affairs. Office emergencies and emergency
kits. J Am Dent Assoc 2002;133:364‑5.
How to cite this article: Prasad KD, Hegde C, Alva H, Shetty M.
Medical and dental emergencies and complications in dental practice
and its management. J Educ Ethics Dent 2012;2:13-9.
Source of Support: Nil, Conflict of Interest: None declared
Author Help: Reference checking facility
The manuscript system (www.journalonweb.com) allows the authors to check and verify the accuracy and style of references. The tool checks
the references with PubMed as per a predefined style. Authors are encouraged to use this facility, before submitting articles to the journal.
•
The style as well as bibliographic elements should be 100% accurate, to help get the references verified from the system. Even a
single spelling error or addition of issue number/month of publication will lead to an error when verifying the reference.
•
Example of a correct style
Sheahan P, O’leary G, Lee G, Fitzgibbon J. Cystic cervical metastases: Incidence and diagnosis using fine needle aspiration biopsy.
Otolaryngol Head Neck Surg 2002;127:294-8.
•
Only the references from journals indexed in PubMed will be checked.
•
Enter each reference in new line, without a serial number.
•
Add up to a maximum of 15 references at a time.
•
If the reference is correct for its bibliographic elements and punctuations, it will be shown as CORRECT and a link to the correct
article in PubMed will be given.
•
If any of the bibliographic elements are missing, incorrect or extra (such as issue number), it will be shown as INCORRECT and link to
possible articles in PubMed will be given.
[Downloaded free from http://www.jeed.in on Sunday, June 18, 2017, IP: 159.255.164.73]
