Lecture 16th (9-13th April 2016)Urinary system
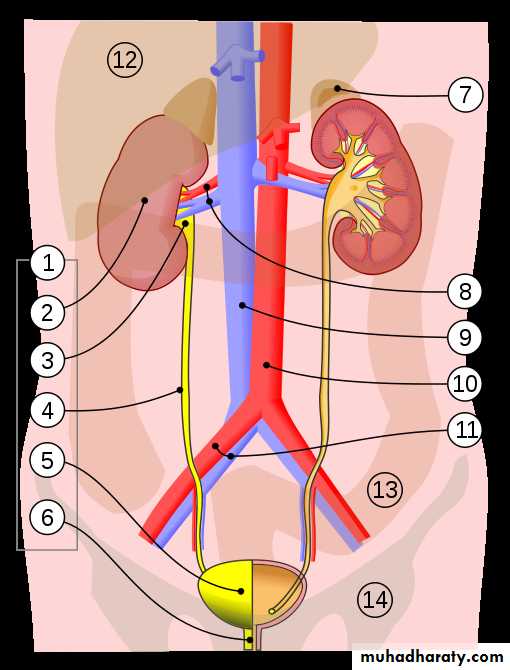
The urinary system (renal system), consists of two kidneys, two ureters, a bladder, and a urethra. The waste products of metabolism are excreted through the urinary system (Fig.1). Each kidney consists of millions of functional units called HYPERLINK "https://en.wikipedia.org/wiki/Nephrons" \o "Nephrons" nephrons. The kidneys have extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Almost 1,800 liter of blood passes through the kidneys in one day, out of which 1.8 liter of glomerular filtrate is formed and only about 1.5-1.8 liter of urine is excreted. Following filtration of blood and further processing, wastes (in the form of urine) exit the kidney via two ureters which are tubes made of smooth muscle fibers that propel urine towards the urinary bladder, where it is stored and subsequently expelled from the body by urination. The female and male urinary system are very similar, differing only in the length of the urethra.Urine is formed in the kidneys through filtration of blood. The urine is then passed through the ureters to the bladder, where it is stored. During urination, the urine is passed from the bladder through the urethra to the outside of the body. Almost 800-2,000 milliliters (mL) of urine are normally produced every day in a healthy human. This amount varies according to fluid intake and kidney function.
(Fig.1): 1. Human urinary system: shows (2). Kidney, (3). Renal pelvis, (4). Ureter, (5). Urinary bladder, (6). Urethra; (7). Adrenal gland Vessels: (8). Renal artery and vein, (9). Inferior vena cava, (10). Abdominal aorta, (11). Common iliac artery and vein; (12). Liver, (13). Large intestine, (14). Pelvis
Structure:
The urinary system refers to the structures that produce and conduct urine to the point of excretion. The human body normally has a pair of kidneys (one in each side). Urine is formed by HYPERLINK "https://en.wikipedia.org/wiki/Nephron" \o "Nephron" nephrons, the functional unit of the kidney, and then flows through a system of converging tubules called collecting ducts. The collecting ducts join together to form minor calyces, then major calyces, which ultimately join the pelvis of the kidney (renal pelvis). Urine flows from the renal pelvis into the HYPERLINK "https://en.wikipedia.org/wiki/Ureter" \o "Ureter" ureter, a tube-like structure that carries the urine from the kidneys into the bladder (Fig.1).
During urination, the urine stored in the bladder is discharged through the urethra. In males, the urethra begins at the internal urethral orifice in the HYPERLINK "https://en.wikipedia.org/wiki/Trigone_of_urinary_bladder" \o "Trigone of urinary bladder" trigone of the bladder, continues through the external urethral orifice, then becomes the prostatic, membranous, bulbar, and penile urethra. Urine exits through the external urethral meatus. The female urethra is much shorter, beginning at the bladder neck and terminating in the vaginal vestibule.
Circulation of Blood through kidney:
The renal arteries are short and broad to maintain hydrostatic pressure for proper filtration of blood. Each renal artery on entering the kidney divides into dorsal and ventral branches, which subsequently, subdivide to run between the adjacent pyramids and are termed interlobar arteries. At the base of the pyramid, interlobar artery divides dichotomously into branches which run at right angle to the parent stem called arcuate arteries. Neither interlobar nor the arcuate arteries of each lobe do anastomous with the adjacent arteries. Arcuate artery gives rise to numerous straight interlobular arteries. Each interlobular artery gives off the afferent arterioles for the cortical glomeruli and for the juxtamedullary glomeruli. These break up into glomeruli plexus of the glomerulus and rejoin to form efferent arterioles. Efferent arterioles at cortical glomeruli form cortical interlobular capillary network, which drains into interlobular vein. This in turn ends into arcuate, interlobular and finally renal vein. Efferent arterioles of the juxtamedullary glomeruli break up in the medulla into bundles of thin walled veins, the vasa recta which make hair-pin bends at varying levels and reach back into the cortex. Vasa recta serve as arcuate, interlobar and finally into the renal vein. .
Histology
Under microscopy, the urinary system is covered in a unique lining called HYPERLINK "https://en.wikipedia.org/wiki/Urothelium" \o "Urothelium" urothelium, a type of transitional epithelium. Unlike the epithelial lining of most organs, transitional epithelium can flatten and distend. Urothelium covers most of the urinary system, including the renal pelvis and ureters.
Functions of the Urinary system:
Removal of waste product from the body (mainly urea and uric acid)
Regulation of electrolyte balance (e.g. sodium, potassium and calcium)
Regulation of acid-base homeostasis (pH).
Controlling blood volume and maintaining blood pressure.
Urine formation:
Average urine production in adult humans is about 1–2 mL/day depending on state of hydration, activity level, environmental factors, weight, and the individual's health. Producing too much or too little urine requires medical attention. HYPERLINK "https://en.wikipedia.org/wiki/Polyuria" \o "Polyuria" Polyuria is a condition of excessive urine production (>2.5 mL/day). HYPERLINK "https://en.wikipedia.org/wiki/Oliguria" \o "Oliguria" Oliguria when <400 mL (millilitres) are produced, and HYPERLINK "https://en.wikipedia.org/wiki/Anuria" \o "Anuria" anuria one of < 100 mL/day.
The first step in urine formation is the filtration of blood in the kidneys. In a healthy human the kidney receives between 12 and 30% of cardiac output, but it averages about 20% or about 1.25 L/min.
The basic structural and functional unit of the kidney is the HYPERLINK "https://en.wikipedia.org/wiki/Nephron" \o "Nephron" nephron. Its chief function is to regulate the concentration of water and soluble substances like sodium by filtering the blood, reabsorbing what is needed and excreting the rest as urine.
In the first part of the nephron, Bowman's capsule filters blood from the circulatory system into the tubules. Hydrostatic and osmotic pressure gradients facilitate filtration across a semi permeable membrane. The filtrate includes water, small molecules, and ions that easily pass through the filtration membrane. However larger molecules such as proteins and blood cells are prevented from passing through the filtration membrane. The amount of filtrate produced every minute is called the HYPERLINK "https://en.wikipedia.org/wiki/Glomerular_filtration_rate" \o "Glomerular filtration rate" Glomerular Filtration Rate or (GFR) and amounts to 180 litres/day. About 99% of this filtrate is reabsorbed as it passes through the nephron and the remaining 1% becomes urine. The urinary system is regulated by the endocrine system by hormones such as HYPERLINK "https://en.wikipedia.org/wiki/Antidiuretic_hormone" \o "Antidiuretic hormone" antidiuretic hormone, HYPERLINK "https://en.wikipedia.org/wiki/Aldosterone" \o "Aldosterone"aldosterone, and parathyroid hormone.
Histology of the Kidney:
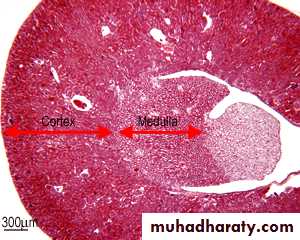
Two bean shaped kidneys are attached to the posterior abdominal wall, one on each side of the vertebral column (Fig. 1). The kidneys have a tough fibrous capsule (irregular dense connective tissue) and adipose tissue for protection. Otherwise they have very little connective tissue between the HYPERLINK "http://www.histology.leeds.ac.uk/urinary/nephron.php" nephrons. The kidney is divided into many lobes 6-18 conical masses with a pyramidal structure (renal pyramids), where the outer portion is made up of cortex, and the inner portion is made up of the medulla (Fig. 2). The bases of the pyramids are directed peripherally and the apices directed inward towards the renal sinus. Each pyramid and the cortical tissue capping is called a lobe of kidney. The extensions of medulla into the cortex are called the medullary rays which within cortex are called columns of Bertini. The kidney contains about 1 million functional units called HYPERLINK "http://www.histology.leeds.ac.uk/urinary/nephron.php" nephrons, which are continuous with a system of collecting tubules. The HYPERLINK "http://www.histology.leeds.ac.uk/urinary/nephron.php"nephrons are responsible for filtration, excretion and re-absorption, and they regulate ion balance, water content, help to stabilize blood pressure. This regulation of ion balance and water content (Osmo-regulation) of the blood plasma means that all the other body fluids will also be regulated. Urine leaves the kidney via the HYPERLINK "http://www.histology.leeds.ac.uk/urinary/ureter.php" ureter for temporary storage in the bladder.
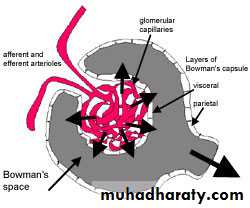
Renal Corpuscle:
The renal corpuscle is formed when a mass of glomerular capillaries grows into the blind ending of a nephron. The nephron encapsulates this mass of capillaries, and it invaginates to form Bowman's capsule. The lining epithelium (simple squamous epithelial cells) on the inside (visceral layer) of become closely associated with the capillaries. The outer layer of epithelium is called the parietal layer (simple squamous epithelial cells). Blood is filtered out from the capillaries through the visceral layer of epithelium into the capsular (Bowman's) space, and can move out from here into the proximal convoluted tubule (PCT).
(Fig. 2): CS of kidney shows the cortex and the medulla in low power (H&E).
(Fig. 3b): A schematic diagram shows the major features of the renal corpuscle.
(Fig.4): A CS in renal corpuscle, shows a Bowman's capsule, and the renal corpuscle.
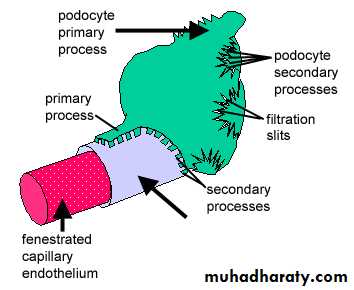
(Fig. 5): A diagram shows how a representative visceral epithelial cell, known as podocytes is wrapped around a capillary because of their unusual shape. Primary processes radiate from the cell body, and form branched secondary processes called podocyte feet that extend onto the basement membrane.
Large amounts of glomerular filtrate are produced for two reasons:
1). The glomerular capillaries do not drain into veins, but into an efferent arteriole. Both afferent and efferent arterioles have smooth muscle cells in their walls. Contraction of this smooth muscle, maintains a relatively high hydrostatic pressure along the length of the capillaries.2). The glomerular capillaries are fenestrated, which enables blood to be filtered out.
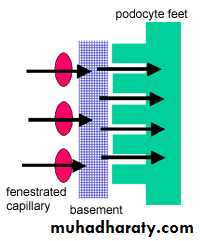
(Fig. 6): The passage of blood out from the fenestrated capillary through the basement membrane into the podocyte, through the feet. These 'feet' interdigitate with those from other podocytes to form filtration slits that are only 20-30 nm wide.
Molecules from blood plasma must:
1. pass through the fenestrated capillary epithelium (fenestrations are 50-100nm in diameter)2. pass through the thick basement membrane (main filtration barrier)
3. pass though filtration slits between the podocyte feet.
(Fig. 7): An (SEM) micrograph demonstrates the primary foot processes of the podocytes.
(Table 1): Histological and physiological comparison between PCT and DCT.Proximal Convoluted tubules (PCT)
Distal convoluted tubules (DCT)
Locate closer to the Bowman's capsule which leads from Bowman's capsule to the loop of Henle
Locates distal to the Bowman's capsule
Have a small lumen
Have larger lumen
Have large brush border cells for extra absorption
No brush border cells and the cells are smaller than those of PCT.
The cytoplasm of the cells is densely packed with mitochondria in the basal region. The high quantity of mitochondria gives the cells an acidophilic appearance.
Molecules can be sorted by this 'sieving' mechanism by size (up to about 70,000kDa can pass) and charge (Negative charge of heparin sulphate proteoglycan in the basement membrane repels negatively charged proteins such as albumin).
Nephron:
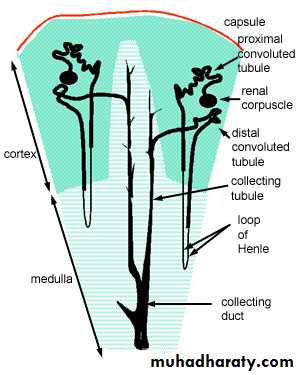
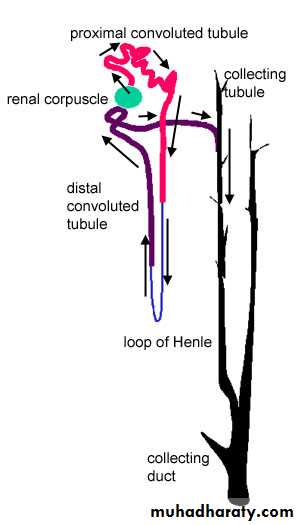
The nephron consists of the renal corpuscle and the renal tubule. The nephron is responsible for filtration, excretion and resorption. It filters out small molecules from plasma, selectively re-absorbs most of the water, and some of the molecules, and also secretes some secretory products into the filtrate. The end product is urine. This schematic diagram shows where the different parts of the nephron are found in the cortex and medulla of the kidney.
(Fig. 8 a& b): This schematic diagram shows where the different parts of the nephron are found in the cortex and medulla of the kidney. (b): The beginning of the distal convoluted tubule is found close to the renal corpuscle, in a structure known as the HYPERLINK "http://www.histology.leeds.ac.uk/urinary/juxta_glom.php" juxtaglomerular complex.
Filtration of the blood plasma takes place in the renal corpuscle. This is the proximal end of the nephron, which is expanded into an ovoid structure. The renal corpuscles are always found in the renal cortex. Here a compact mass of looped fenestrated capillaries called the glomerulus (latin for 'small ball') is encapsulated by the proximal end of the renal tubule (Bowman's capsule). After leaving the renal corpuscle, the filtrate passes through the renal tubule in the following order:
Proximal convoluted tubule [PCT] (found in the renal cortex)
loop of Henle (mostly in the medulla)
distal convoluted tubule [DCT] (found in the renal cortex)
collecting tubule (in the medulla)
collecting duct (in the medulla)
The beginning of the distal convoluted tubule is found close to the renal corpuscle, in a structure known as the HYPERLINK "http://www.histology.leeds.ac.uk/urinary/juxta_glom.php" juxtaglomerular complex.
Ureter:
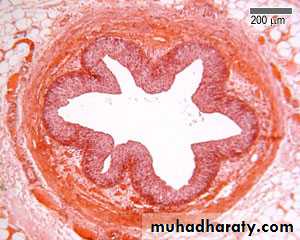
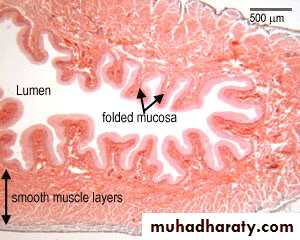
(Fig. 9): The ureter (one per kidney) is a long, straight, muscle-walled tube. The epithelium lining this tube is stratified, transitional epithelium. Why do you think this is?
A thick, fibroelastic, lamina propria lies underneath the epithelium.
This mucosa (epithelium and lamina propria) is protective.There are no mucosal or submucosal glands, and no submucosa.
There is a layer of smooth muscle outside the mucosa:
The upper two-thirds has two layers of smooth muscle: inner longitudinally arranged, and outer circularly arranged.
The lower third has three layers of smooth muscle; Inner longitudinal, middle circular, outer longitudinal.
Urine is squeezed into the bladder by peristalsis.
Outer adventitial layer has fibroelastic connective tissue, with blood vessels, lymphatics and nerves.
Folds of mucosa help to protect against reflux of urine when the bladder is full.
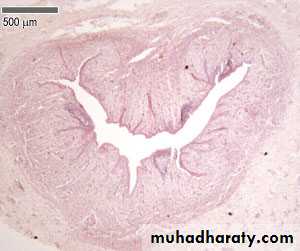
The bladder has three layers of smooth muscle, and a transitional epithelium. It's harder to make out the three layers, because the bladder is sac like, not a tube.
The mucosa is heavily folded - this helps to accomodate for large volume changes.
The transitional epithelial lining can stretch until it looks like stratified squamous epithelium.
(Fig. 10): Section in urinary bladder demonstrates the folds of mucosa (transitional epithelial tissue) inside the lumen. Note the muscular layer made up of smooth muscles arranged in various directions.
Calculi in ureter: Small stones or uretic calculi are seen in ureter. Many of them are formed in kidney, slip down the ureter and get lodged in the constricted parts of ureter. A severe acute pain could generate due to blockage in the path of urine.
Stones in urinary bladder: Calculi could be passed down to bladder where they may increase in size. Stones, sometimes, may generate in the urinary bladder if there is chronic inflammation or urethral obstruction.
Urethra:
(Fig. 11): The urethra conveys urine from the bladder to the exterior of the body. It is similar in structure to the ureter, though shorter. The lumen is kept closed, unless urine is being passed. The female urethra is lined by stratified columnar epithelium, with a few small mucosal glands that secrete mucus, and is bound to the anterior wall of the vagina by an external layer of fibrous connective tissue.
Regulation of concentration and volume
The urinary system is under influence of circulatory system, nervous system and endocrine system. Aldosterone plays a central role regulating blood pressure through its effects on the kidney. It acts on the distal tubules and collecting ducts of the nephron and increases reabsorption of sodium from the glomerular filtrate. Reabsorption of sodium results in retention of water, which increases blood pressure and blood volume. Antidiuretic hormone (ADH), is a HYPERLINK "https://en.wikipedia.org/wiki/Neurohypophysial_hormone" \o "Neurohypophysial hormone" neurohypophysial hormone found in most mammals. Its two primary functions are to retain water in the body and to constrict blood vessels. Vasopressin regulates the body's retention of water by increasing water reabsorption in the collecting ducts of the kidney nephron. Vasopressin increases water permeability of the kidney's collecting duct and distal convoluted tubule by inducing translocation of aquaporin-CD water channels in the kidney nephron collecting duct plasma membrane.Urination:
Urination is the ejection of urine from the urinary bladder through the urethra to the outside of the body. In healthy humans (and many other animals), the process of urination is under voluntary control. In infants, some elderly individuals, and those with neurological injury, urination may occur as an involuntary reflex. Physiologically, micturition involves coordination between the central, autonomic, and somatic nervous systems. Brain centers that regulate urination include the HYPERLINK "https://en.wikipedia.org/wiki/Pontine_micturition_center" \o "Pontine micturition center"pontine micturition center, HYPERLINK "https://en.wikipedia.org/wiki/Periaqueductal_gray" \o "Periaqueductal gray" periaqueductal gray, and the cerebral cortex.
Clinical Significance:
Urologic disease can involve congenital or acquired dysfunction of the urinary system. Diseases of other bodily systems also have a direct effect on urogenital function. For instance it has been shown that protein released by the kidneys in Diabetes mellitus sensitises the kidney to the damaging effects of hypertension. Diabetes can exert a direct effect in urination due to peripheral neuropathies which occur in some individuals with poorly controlled diabetes. Urinary incontinence can result from a weakening of the pelvic floor muscles caused by factors i.e. pregnancy, childbirth, aging and being overweight.
Acute glomerulonephritis, is a disease very common in children and young adults, occur 2-3 weeks after pharyngitis due to grou A haemolytic streptococcal infection (bacterial infection).
Tuberculosis of the kidney is usually due to blood spread infection from the lung. Bacilli (another bacteria), settle in cortex, caseous foci appear, which spread to medulla, pelvis, ureter and urinary bladder. The disease can destroy renal structure.