BURN
Definition:Burn is coagulative necrosis of tissues due to either physical or chemical agents.
Aetiology:
Physical agents (either thermal or electrical),Chemical agents (strong acids and alkalies).
Thermal injury is the most common cause of burn, about 95% of the causes.
Thermal injury means that both extremes of temperatures can injure the tissues. The low extreme also can cause tissue injury e.g. frost bite, also cryotherapy at some time ago was one of the modalities of treatment of some skin lesions.The high extreme of temperature as a cause of burn is the one which we meet in almost all cases of thermal injury.
It may be flame, hot liquid (scalds), or vapors and the third is contact with hot solid object.
The intensity of burn varies according to the temperature of the affector and the time of contact or exposure
Electrical burn:
Most of the damage is beneath the skin surface and therefore the actual injury can easily be underestimated.The pathway of current can be somewhat unpredictable, but, in general, current passes from a point of entry through the body to a grounded site .
Extremely high voltage sources usually exit in multiple areas in an explosive fashion.
Current passing from hand to hand or hand to thorax has a high risk of producing cardiac fibrillation compared to hand to foot passage.Passage through the head is likely to cause an initial respiratory arrest and subsequent severe neurologic impairment.
Electrical burns more closely resemble a crush injury than they do a thermal burn.
The damage below the skin where the current passes is usually far greater than the appearance of the overlying skin would indicate.
The immediate damage to muscle is caused by the heat, which is usually patchy in distribution along the course of the current, often most severe near the bones
Chemical agents:
Chemical burns are commonly seen in the home but especially in the workplace.These chemicals can produce local tissue injury and some have potential to be absorbed resulting in body poisoning.
Chemical burn is usually deeper than it looks as the skin is destroyed mainly by chemicals.
.
Its appearance is often brown to gray as opposed to the typical white or char with a flame burn. It continues to get deeper and later appearance is usually worse.
Severe persistent pain is often present indicative of ongoing skin damage.
Chemical toxins like phenol or hydrocarbons like gasoline may cause only skin irritations, but absorption can lead to systemic poisoningBurn Depth:
To understand the burn depth we should review the histology of the skin.
Skin is the largest organ in the human body. It consists of two layers, the epidermis and the dermis.
The outermost epidermal layer is the stratum corneum . It is continually sloughed off and regenerated by keratinocytes, and it serves as a protective barrier to the environment.
.
The dermis is composed primarily of fibrous connective tissue.
Embedded within the dermis are blood vessels, cutaneous nerves, skin appendages, hair follicles, and sebaceous and sweat glands.Because these skin appendages are lined with epidermal cells, they are a source of regenerating epidermal cells after thermal injury
When the skin is burned, these functions are lost. The loss of the stratum corneum allows the invasion of microorganisms, and the Langerhans’ cells, which mediate local immune response, are also gone.
severely burned patients, the systemic immune response is suppressed, which renders the patient highly susceptible to serious infections.
Thus, topical antimicrobial dressings are essential in controlling wound surface pathogens.
The loss of the epidermal barrier causes increased fluid losses until the wound is completely reepithelialized, not just during the initial resuscitation period.
Deep thermal injuries that destroy the dermis and subcutaneous tissue often heal with significant wound contractures and impaired mobility, especially across joint surfaces.
According to the depth of burn, the burn is classified into 4 degrees: 1st degree:
# Only epidermal injury.# Simple erythema can be produced from relatively hot liquids or solid objects or flash flame burn.
# The pain is severe.
# Mild to moderate oedema may occur but no external fluid loss or ooze and no vesicles.
# Healing usually occur within 5 to 7 days without any residual color changes.
# No treatment is necessary except analgesia.
2nd degree:
The burn is deep in the superficial dermis but leaving the dermal deep layer intact not including the whole depth.Clinically, there is erythema and vesicles and bullae variable in size containing transudate rich in proteins; if ruptured, the wet surface will continue oozing in addition to the regional oedema.
The pain is more severe.
Superficial 2nd degree burn:In which burn reach the level of papillary dermis.
It heals within 10 to 15 days with minimal residual color
changes without any hypertrophic scarring if treated well using sterile dressing and no infection occurred.
(a) A superficial partial-thickness scald 24 hours after injury. The dermis is pink and blanches to pressure.
) At 2 weeks, the
wound is healed but lacks pigment.
.
At three months, the pigment
is returning.Deep 2nd degree burn:
In which the reticular dermis is affected.Healing occurs within 15 to 25 days with some hypo or
hyperpigmentation and sometimes complete loss of pigmentation (Leukoderma).Fibroplastic reaction is manifested producing excessive collagen fiber hypertrophic scar and may be keloid with partial or complete loss of skin elasticity.
Wound infection may convert this burn to 3rd degree burn.
3rd degree:
It affects the whole skin depth.The skin losses its elasticity becoming dry and changes to parchment like,
painless,
no oozing but oedema is more.
In general it is more dangerous than the 2nd degree. Being the hair follicles are burned, easy, painless hair epilation is well known and the pin brick test is painless also.
The dead skin (Eschar) separates within 2 to 3 weeks leaving underneath healthy granulation tissue ready to accept skin graft if the general condition of the patient still good and the wound flora within the acceptable low level of contamination.
4th degree:
Burns are deeper injuries involving the underlying muscle, bone, and other structures.Burn Surface Area:
The fluid loss from the burn wound is either oozing externally or collecting interstitially as oedema which is very valuable to the body due to its high content of proteins and electrolytes and also the body water itself.
The more surface area affected by burn, the more loss and more disarrangement of the body general condition.
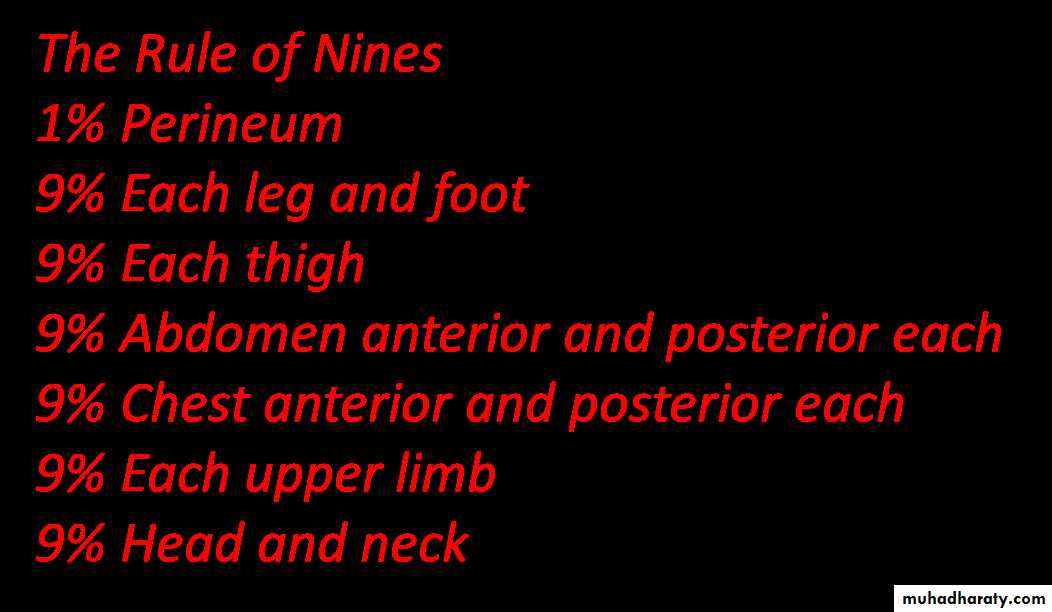
Due to that , we always estimate the surface area burnt as % of the body surface area. The most popular more accurate in adults and the simplest is The Rule of Nines .
It is sometimes useful to use the fact that the patient’s palm is 1% of his/her body surface area.
Burn surface area 10% or more of the body surface area (BSA) is considered to be hospitalized and fluid therapy should be administered.
The severity of burn depends on 2 items, the depth and extent of burn.
The danger increases if the BSA burnt is larger and also more dangerous if most of the area burnt is deep.Burn Shock:
types of shock can affect the burn victim.#Neurogenic shock : It is due to severe pain which can be fatal in extensive burns. Its treatment is pain killers, the best and more effective is I.V. morphine.
# Hypovolaemic shock: It is due to fluid loss and sometimes blood loss. Paralysis of capillary tone which starts to occur short time after the accident and reaches its maximum in few hours. With the best circumstances, the body reacts to compensate after 8 hours and the capillary tone starts to come back.
Gradual absorption of the oedema fluid which is supposed to be corrected completely after the 1st 48 hours. This is the scientific bases of the fluid therapy.
Factors contributing to hypovolaemic shock:
Increased capillary permeability (leading to increased interstitial edema).Increased fluid sequestration in muscle cells.
Increased evaporative water loss from destruction of the skin-water barrier.
Red blood cell destruction from initial thermal insult.
.
Septic shock:
It is due to bacteremia caused by burn wound infection or secondary infection.It is characterized by: Hypotension, Tachypnea, Spiking fever, Tachycardia, Altered mental status, Decreased urine output, Progressive leukocytosis with left shift, Thrombocytopenia, Hyperglycemia, Metabolic acidosis, and Hypoxia.
Resuscitation Fluid Therapy:
Indications for resuscitation:Adults: burns involving more than 20% TBSA
Children: burns involving more than 10% TBSA
Electric injury:
any burn patient with hemochromogens in urine.
The extremes of age or with preexisting disease that would likely reduce normal compensatory responses to even minor hypovolemia (e.g. cardiac or pulmonary disease)
Resuscitation formulas: Parkland’s formula :
In the 1st day: lactated Ringer’s solution, 4ml/kg/% burn
½ total in first 8 hr ,
¼ total in next 8 hr,¼ total in next 8 hr
In the 2nd day: 0.5 cc/Kg/%TBSA (700-2000 cc) Colloids (adult) as required to maintain normal urine output
Monitoring resuscitation
Urine output 30-55cc/hr in adults and1.2cc/Kg/hr in children < age 12
A clear sensorium, pulse <120/min, HCO3 > 18 meq/L, cardiac output >3.1 L/M2 >CVP in acute major burns is unreliable
Inhalational Injury:
Inhalation injury has a significant impact on the survivability of a burn injury. It has three components:Carbon monoxide intoxication,
Upper airway swelling,
Acute respiratory failure.
These components may occur alone or in combination, and they may vary in severity from inconsequential to life-threatening.
Inhalation injury is usually evident by a characteristic history and physical examination.
.
.
Patients are usually injured in an enclosed space, such as a house or car. They may be coughing up carbonaceous sputum.
Physical stigmata include:
Facial burns,
Singed nasal hair,
Soot in the pharynx.
A new onset of hoarseness may indicate vocal cord swelling, and a bronchoscopy can help to make a definitive diagnosis of inhalational injury
.
Carbon monoxide is a colorless, odorless gas that binds to hemoglobin 200 times more avidly than oxygen, thereby limiting the ability of the hemoglobin to transport oxygen.
The toxicity of CO is directly related to the percentage of hemoglobin it saturates.
Treatment for carbon monoxide intoxication is based on the ability of increased concentrations of oxygen to increase the rate at which CO is diffused.A concentration of 100% oxygen increases the rate of CO diffusion from hemoglobin from 4 hours to 45 minutes
Although hyperbaric oxygen is useful in treating patients with isolated CO intoxication, its use complicates the care of patients with skin injuries.
Upper airway swelling is a very dangerous sequelae of inhalation injury because swelling can quickly progress to total airway obstruction.
This process begins several hours after injury and lasts for 2 to 4 days as tissue edema wanes.
The diagnosis is made by a direct visualization of the upper airway. If swelling, erythema, or soot is present, the patient should be intubated. The airway should be visualized again at 48 hours and daily thereafter to assess airway edema.
Extubation is safe when soft tissue swelling has waned. If the patient can breathe or talk with the endotracheal tube occluded and the cuff deflated, airway swelling has usually subsided.
Acute respiratory failure can occur hours to days after a burn injury. This process is a type of chemical pneumonitis caused by the toxic products of combustion.
Complications of Burns:
Early complications:Shock Neurogenic Hypovolaemic Septic
Asphyxia, due to oedema of the glottis. It needs urgent tracheostomy.Toxaemia Acute toxaemia Septic toxaemia
Fluid and electrolyte disturbances.
Injury of blood vessels and nerves.
Acute gastric dilatation or paralytic ileus.
Acute duodenal ulcers (Curling’s ulcer): It may occur in the stomach or duodenum. In the stomach, it’s usually multiple, small, elongated ulcers (Stress ulcers).
In the duodenum, it’s characteristically solitary, posteriorly located, large and deeply penetrating. The only symptom is epigastric discomfort which usually passes un-noticed until massive bleeding occurs.
Retension of urine, in perineal burns.
Pulomary complications: As; Acute respiratory obstruction (Upper resp. obst.) Inhalation injury of the tracheo-bronchial tree, due to inhalation of fumes and also heat
Adult respiratory distress syndrome is a late complication, treated by Oxygen, Steroids, and assisted respiration.
Pneumonia, and Atelectasis are common among critically ill patients.
Urinary complications, as cystitis and urethritis due to prolonged catheterization.
Gangrene, due to constricting eschars.
Decubitus ulcers and another complications of decumbency
Heart failure, due to myocardial depression.
Supra-renal failure, due to septic shock.
Hepato-renal failure.
Abortion OR pre-term labour.
Late complications:
Disfigurement due to scars and keloids.
Contracture of the joints.
Chronic ulcers that may be complicated by malignancy.
Endocrine complications, as Amenorrhoea, Hursuitism, Testicular
atrophy.
Psychological upset, up to mania.
Management of Burns:
Initial management
A patent airway should be assured. If there is evidence of airway obstruction, an endotracheal tube should be inserted.
A strong analgesic as 50mg Pethidine is administered by IV route
Tetanus prophylaxis is followed.
Saline or tap water, at room temperature, can be poured over the burnt area for 15min to decrease edema and relieve the pain. Using ice is contraindicated as it may induce more tissue damage.
Minor burn (less than 15% in adults and 10% in children): can be treated as outpatients: Dressing using the proper chemotherapeutic. Analgesics. Systemic antibiotic prophylactic.
All major and most moderate burns (except very superficial ones) should be admitted to the burn unit:
A wide bore IV cannula is inserted rapidly before the veins get collapsed.
A Foley’s urethral catheter is introduced to check the urine output.Fluid therapy to compensate for the extensive losses. (as previously mentioned)
Local care of the burn wound.Wound care Escharotomy / Fasciotomy Escharectomy + homograft Dressing / hydrotherapy Debridement Application of autograft Splinting contractures management
The aim is to avoid infection
Only constricting eschars (in the limbs and chest) may have to be released immediately.
Escharotomy In large burns with generalized edema, circumferential burn eschar of the extremities can prevent swelling of the underlying tissue.
The surgical division of these constricting eschars (escharotomies) is performed to maintain the blood flow to the distal extremities. Because the eschar itself is insensate, this procedure can be performed in most patients at the bedside using sedation and analgesics. Both sharp division and electrocautery are effective.
Thorough cleansing, removing loose skin, and initial conservative debridement can be performed.
Topical antimicrobial agents should be applied e.g. silver sulfadiazine, silver nitrate solution, and mafenide acetate
A full-thickness burn on admission just prior to escharotomy
Excision of the same full-thickness burn, down to healthy fat.Exposed method:
The wound is managed by leaving it exposed. It requires isolation of the patient in completely aseptic atmosphere and following all aseptic rules by the personnel dealing with the patient.Advantages: It is more comfortable to the patient. >It avoids the needs for repeated change of dressings which implies a great burden on nursing staff and is rather expensive.
It inhibits the growth of bacteria by the dry air surrounding the burn. Indications: Burns of the face, neck and perineum. Burns involving one side of the trunk.
Occlusive method:
The wound is covered by a bulky occlusive dressing that is changed every 2-3 days depending on the state of the burn wound. Dressing change in the occlusive method can be done under anesthesia (especially in children) since it is usually very painful and adherent.
Surgical management:
Indications for surgery:Full-thickness injuries, or
When the wound is unlikely to heal within 3 weeks,
for the risk of hypertrophic scar and contracture formation.
When the depth of the injury is indeterminate
Surgical debridement:
Tangential excision is the debridement of graduated amounts of necrotic tissue until viable tissue is reached. This usually can be determined by punctate hemorrhage in the wound bed. The advantages of this technique are an accurate removal of nonviable tissue and the preservation of as much subcutaneous tissue as possible. The disadvantage is blood loss.Wound closure
The second phase of surgical treatment is wound closure. Some small burns can beexcised and closed primarily. This obviates donor site morbidity and gives an excellent result, but it is seldom possible.