Laminitis(Founder)
Definition:- Inflammation Of the laminae of the foot(simple def.). But really it is a complicated, interrelated events that results in varying degrees of foot pathology.Resent research suggests that laminitis is in fact peripheral vascular disease manifested by decreased capillary perfusion within the foot, significant amount of ateriovenous ischemic necrosis of the laminae, and pain, related to systemic metabolic disorder that affects the cardiovascular, renal and endocrine system, blood coagulation and acid base condition.
Etiology:-
1- Ingestion of toxic amount of grain(grain founder), ingestion of greater quantities of grain such as wheat, corns and barley, which are rich with high carbohydrate level.Mechanism of reaction
ِِِAlter
High carbohydrate bacterial balance within the cecum primarily Lactobacillus and streptococcus
Increase
Decrease
streptococcus lactic acid level PH
Lysescell wall of G – ve bacteria
Release
AbsorbedVasoactive lipopolysaccharides(endotoxin)
Circulation causing systemic effect
Onset
Laminitis2- Ingestion of large amount of cold water by overheated horse is considered a cause of laminitis. Although this phenomenon is not fully understood, it may be due to gastroenteritis or colitis. Horses that are overheated should be allowed only small amounts of water until they have cooled.
Concussion :- This type of laminitis is the result of concussion to the feet from hard work or fast work on hard surface.
Endometritis or severe systemic infection(posparturant laminitis). A mare may develop this type of laminitis shortly after foaling as a result of infection arising from retention of part of fetal membranes or of a uterine infection. Laminitis may occurs as a results of severe pneumonia or other systemic infections.
Obesity and ingestion of lush grass pasture. It is common in horses grazed on grass pastures particularly that contain clover and alfalfa which are more likely to cause the condition more than other grass pastures. The cause of this type of laminitis is unexplained, but hormonal factors may be an etiologic agent in some cases if grasses or legumes contain estrogen.
Hypothyroidism has also been considered a possible cause of laminitis, low T3 and T4 level in serum.
Miscellaneous causes, which includes:-
Hormonal imbalance particularly in mares.
Following viral respiratory diseases.
Following administration of some drugs.
Clinical Sings:-
--- Acute laminitis ---
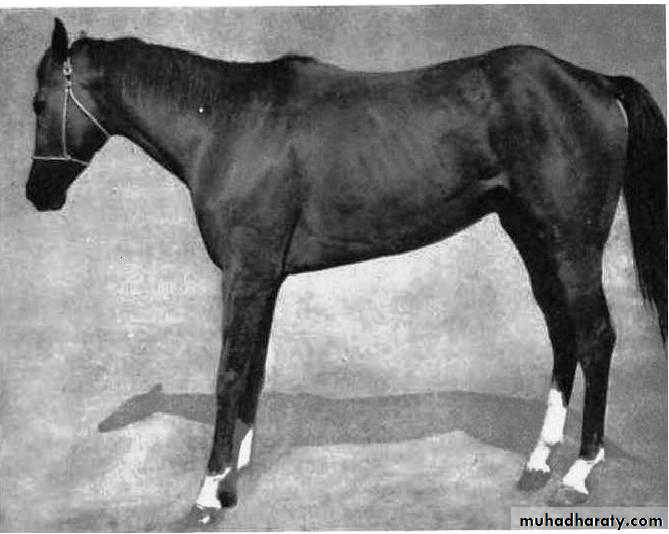
Acute laminitis may affect both front feet or all four feet.
If all four feet are affected the horse tend to lie down for extended period.Most commonly only the two front feet are involved, in this case the hind feet are carried well up under the body and the front feet are placed forward with the weight on the heel of the foot. The horse show great reluctance to move.
Heat is present over the wall of the coronary band.
There is increased digital pulse.
Increased respiration and elevation of temperature and congested mucous membrane.
It is often difficult to lift one foot from the ground.
By using a hoof tester, a uniform tenderness will be noted over the entire area of the sole.
Typical attitude of a horse with laminitis. The hind feet are carried up forward to help take more weight off forefeet, which are extended cranially.
Severity of lameness can be graded by the following criteria:-
Grade 1: At rest the horse will alternately and incessantly lift the feet. Lameness is not evident at a walk but a short stilted gait in noted at a trot.Grade 2: Horses move willingly at a walk, but the gait is stilted. A foot can be lifted off the ground without difficulty.
Grade 3: The horse moves very reluctantly and vigorously resists attempts to have a foot lifted.
Grade 4: The horse refuses to move and will not do so unless forced.
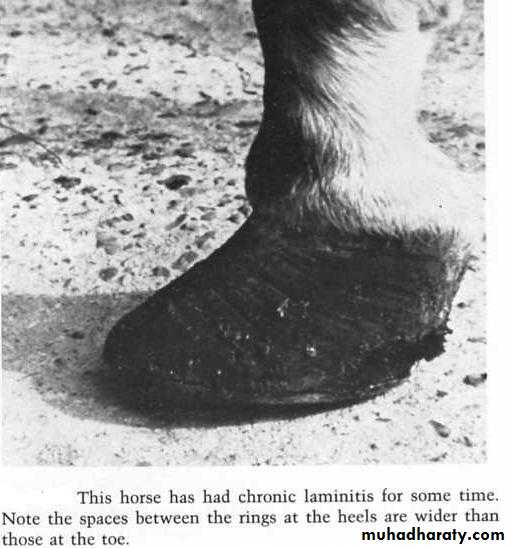
--- Chronic Laminitis ---Laminitis becomes chronic after 48 hours of continual pain or when rotation of the distal phalanx occurs.
Severe lameness may not be present after the acute phase, but an acute recurrence may occur.
When rotation of the distal phalanx occur it can vary from mild to severe.
By examination of the sole, a semicircular separation of the sole just dorsal to the apex of the frog may be noted, indicating that the tip of the distal phalanx is beginning to penetrate the sole.
The hoof wall grow more rapidly than normal and may develop a long toe, and also a heavy ring formation on the hoof wall is seen.
Seedy toe resulting from separation of the laminae is usually present in chronic laminitis.
Hoof tester examination in the chronic phase rarely painful response.
Diagnosis:-
By the typical easily remarkable sings of acute laminitis.Typical attitude of the animal.
Increased pulsation of the digital arteries and heat of the foot.
Hoof tester prove the acute phase of laminitis.
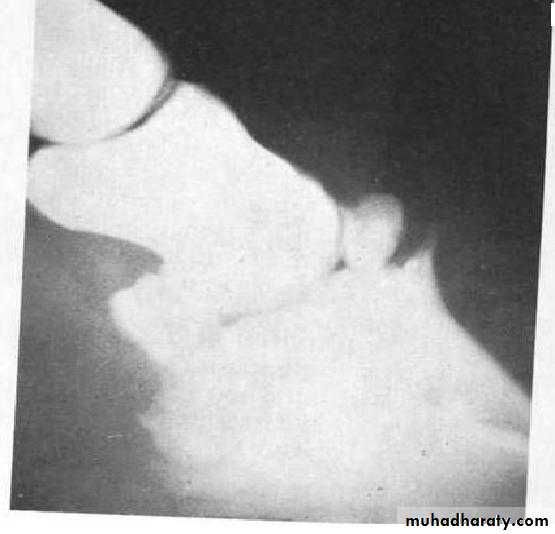
In chronic phase a serial radiographs should be taken from 48-72 hours after the acute onset of laminitis, to monitor the progress of rotation of the distal phalanx, which is identified by divergence of the bone in relationship to the hoof wall.
Treatment:-
Laminitis is considered a medical emergency and treatment for complete recovery should begin prior to rotation of the distal phalanx. The treatment should be initiated within 24 hours after the first onset of lameness, because rotation of the distal phalanx can be observed within 48 hours period.Developmental phase:-
In grain overload, the treatment is directed at neutralizing the effects of the ingested grain and controlling the developmental phase of laminitis. Often the sings of laminitis from this cause do not appear for 12-18 hours after ingestion of the grain, the treatment to clear the intestinal tract is used before the sings of laminitis have yet appear. Mineral oil is commonly used, which act as a bulk laxative and also coat the wall of the intestine perhaps inhibiting absorption of toxins. The treatment can be repeated at 4-6 hours intervals until all grain has been removed from the intestinal tract.Provide short period exercise during the acute onset(10 min./ hour) for the first 24 hours, this will increase the flow of blood through the foot. But it is contraindicated after digital pathology progresses.
Heparin an anticoagulant has been used successfully to prevent laminitis, at a dose of 100 units/ kg given i/v four times a day.
Acepromazine I/M 4 times .
Flunixin meglumine may be beneficial in the prevent and treatment of laminitis because of its anti endotoxic effect. It is given at a dose of 1.1mg/kg 3 times daily for 3-5 days.
In case of septicemia, retained placenta and or Endometritis antibiotics should be added to the previous treatment.
Continuous application of cryotherapy (maintaining hoof wall surface temperature at 5°C–7°C) to the distal aspect of limbs for 48 hours prevents lameness, improves epidermal laminar histologic condition.
Acute phase:-
Using of analgesics and the best one is phenylbutazone at high doses, 4.4mg/kg by I/V rote, since it has an antiplatlet effect may prevent the coagulopathy and the analgesic effect.
Using of acepromazine to reduce vasoconstriction and produce analgesia of pain.
Horse should be placed in stalls with soft sands underfoot, this serves to support the ground surface of the sole and allows the horse to stand in a more comfortable position.
Administration of corticosteroids and antihistamines have been recommended in the past, but recently it is proved they are probably of little benefit in the acutely affected horses.
Using of hot and cold soaks.
Mild exercise recommended for the first 24 hours after the acute onset laminitis.
Prevention of distal phalanx rotation either by application of plaster of paris or using of silicone padded shoes.
Eliminate grain from the diet and giving a good quality of legumes or grass hay.
Injection of diuretics will reduce congestion in the feet.
Ketoprofen analgesic used successfully in the acute phase of laminitis in a dose of 2.2mg/kg four times daily.
More recently a pentafusion analgesic drug are used to decreasing the level of pain. Pentafusion is a combination of drugs which includes Ketamine, Morphine, Lidocaine, Detomidine, and Acepromazine.
Chronic phase:-
Grooving the hoof wall or rasping the quarters to thin the wall and provide their expansion.When infection is present in the sensitive laminae due to sole perforation, the foot should be treated daily by removing the dead and necrotic tissues, local application of Tr. Iodine and bandaging the foot until the infection is over.
Foot trimming and reshaping the hoof by rasping it, to lower the heel so that the distal border of the third phalanx will parallel the surface of the ground when the foot is bearing weight.
Neurectomy of the digital nerve sometimes used to reduce the pain.
Extensor Process Fractures of the Distal (Third) Phalanx
Fracture of the extensor process may occur unilaterally or bilaterally in the forefeet of the horses. It is seen less frequently in the hind feet. It may or may not be accompanied by buttress foot.
Etiology:-
The apparent etiology is excessive tension on the common digital extensor tendon. This can produce enough force to fracture the process.It can also occur from overextension of the coffin joint.
Bilateral cases could be due to congenital fractures.
Clinical Sings:-
Lameness sings are relatively obscure.The cranial phase of the stride is shortened.
There is no reaction to the hoof tester over the frog or other parts of the foot
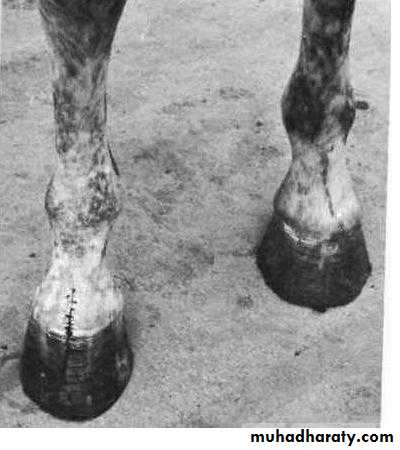
After sometime, there is a change in the shape of the hoof wall, with a tendency for a V- shaped foot.
Lateral radiographs of the foot reveal the fracture or a separated extensor process.
Pain may be shown when pressure is applied over the center of the coronary band.
Fracture of the extensor process of the distal phalanx (Arrow)
Diagnosis:-Diagnosis is established by the changes in the shape of the hoof wall.
Pain on pressure over the extensor process.By radiographs.
Treatment:-
Although conservative treatment consisting of blistering, firing and rest for 3 to 10 months has been used successfully, but it would appear that the convalescent period can be markedly shortened with surgery. Fragments of the extensor process can be removed surgically, or an attempt can be made to fix large fragments with a bone screw.Preoperative preparation:
Preoperative preparation of the hoof should include thorough cleaning, trimming and rasping, and the foot is scrubbed vigorously with povidone iodine and then placed in a pvidone iodine bandage. The surgery is done under general anesthesia with aseptic technique.Surgical technique:
A midline incision is made over the center of the common digital extensor tendon, just above the coronary band.The common digital extensor tendon is separated longitudinally, and the fragment can be palpated and grasped with forceps.
Adhesions to the fragment are dissected and the fragment removed.
The tendon is sutured with simple interrupted sutures of 2-0 synthetic absorbable suture.
The subcutaneous tissues are closed in a similar fashion.
The skin is closed with a 2-0 monofilament nylon with a simple interrupted suture pattern.
The foot is placed in a cast that extends below the carpus for one week.
The cast is removed and the foot kept in a supporting bandage for thirty days.
The horse should not be worked for at least 6 months.
Appearance of the foot after removal of fragment of extensor process of the distal phalanx. Notice the triangular appearance of the affected foot on its dorsal surface as compared to the normal foot. This change is characteristic of long-standing fracture of the distal phalanx.
Ringbone (phalangeal Exostosis)
Ringbone is new bone growth that occurs on the proximal, middle, or distal phalanx. It is the result of a periostitis and may lead to an osteoarthritis or ankylosis of the pastern(proximal interphalangeal) or coffin(distal interphalangeal) joints.Ringbone is classified in two ways:
High or Low RingboneHigh Ringbone: This is new bone growth occurring on the distal end of the proximal phalanx and/or the proximal end of the middle phalanx.
Low Ringbone: This is new bone growth occurring on the distal end of the middle phalanx and/or the proximal end of the distal phalanx, especially at the extensor process of the distal phalanx.
Low ringbone. The upper arrow points to new bone growth on the distal end of the middle phalanx while the lower arrow shows avulsion of a portion of the extensor process of the distal phalanx. These changes are due to tension on the common digital extensor tendon
High ringbone. The top arrow indicates new bone growth at the edge of the pastern joint. The lower arrow indicates new bone growth on the dorsal surface of the proximal end of the middle phalanx.
B- articular or Periarticular Ringbone
Articular Ringbone: Articular ringbone means that the new bone growth involves the joint surface at the pastern (proximal interphalangeal) or coffin (distal interphalangeal) joints.Periarticular Ringbone: Periarticular ringbone means that the new bone growth is around the joint but does not involve the joint surface It is more common in high ringbone.
Etiology:-
Nonarticular ringbone results from a periostitis produced by pulling of the collateral ligaments of the joints involved, pulling of the joint capsule attachments to the bone, pulling of the attachment of the extensor tendon to the proximal, middle, or distal phalanx. Pulling of these structures disturbs the periosteum, and periostitis and new bone growth result.Nonarticular high ringbone is most common in horses with high heels and short toes.
Wire cuts in the pastern region may cause periostitis that will cause ringbone, if the cut extends into the periosteum.
Articular ringbone (osteoarthrosis), particularly high ringbone, occur most frequently in horses used for high speed, that make quick stops, short turns, and rapid twisting movements.
Another cause of articular high ringbone in young horses (3 years or younger) is described as an osteochondrosis- like lesion that appears to most severs in the distal aspect of the proximal phalanx.
In some cases, one of the phalanges will fracture in the region of pastern, and this may lead to osteoarthritis of the pastern joint and to severe ringbone.
Poor conformation may predispose to pulling of the collateral ligaments, joint capsule which lead to ringbone formation.
Clinical Sings:-
Ringbone may occur in either the fore- or hind feet, but it is more common in the forefeet
Sings of lameness are not specific. Lameness is usually evident in all gaits and upon turning.
Heat and swelling will be present over the involved regions, and the horse will sometimes flinch when finger pressure is applied to the region of the active ringbone.
Some cases of ringbone are relatively asymptomatic, especially if they are Periarticular.
Early cases of high ringbone, especially those involving the proximal end of the middle phalanx, may show periodic swelling and lameness that will disappear with rest.
As the disease becomes chronic, the swelling will feel firm and cool to the touch.
Flexion and rotation to the phalangeal region results in a painful response, and reduced flexion is usually present
Diagnosis:-
A positive diagnosis of ringbone cannot be made without radiographic examination.
In early cases, when swelling is not marked, the diagnosis is based on finding heat and pain in the involved regions.Careful comparison with the opposite limb should be made.
In early cases of articular and Nonarticular ringbone soft tissue swelling may be present, but radiographic examination will be negative for findings.
In these cases repeat radiographic examination is recommended in 3 to 4 weeks.
The opposite pastern region should be radiographed for comparison.
Treatment:-
If a case is diagnosed in the very early stages before new bone growth begins, limiting motion of the joints by placing the limb in a cast from the hoof wall just below the carpus is a good method of treatment.
The foot should remain in a cast for a minimum of 4 weeks and should be rested for a minimum 4 months.
When the pastern joint has become ankylosed, sings of lameness may not be present. This is especially true in the hind limb, where fractures of the phalanges may heal by ankylosing the pastern joint, particularly for the articular type, but ankylosis relieves pain by preventing joint movement.
Arthrodesis techniques of the proximal interphalangeal joint include:
Drilling the joint from the lateral to the medial side in an attempt to remove as much cartilage as possible, then it is packed with cancellous bone retrieved from another site.
Direct electrical stimulation after the joint cartilage is removed. This shortens the time required for ankylosis to occur.
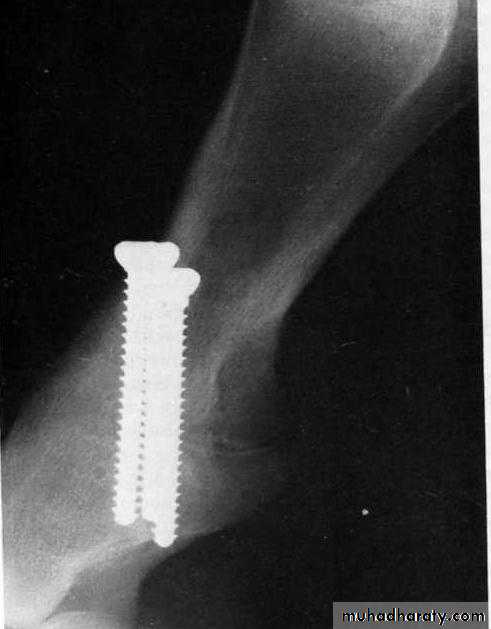
Internal fixation using plates or screws after the cartilage is removed from the joint surface. Good results have been reported with three parallel placed screws that cross the pastern joint and compress it when the screws are tightened.
After surgery the limb is then immobilized to just below the tarsus or carpus in a cast. The foot must be included in the cast.
The cast is removed if needed, but may be left in place for a period of 6-7 weeks if a good fit exists.
If the coffin joint is involved, there is little hope of ever obtaining a sound horse. A neurectomy is sometimes performed to reduce the pain.
A lateral radiograph 7 weeks postoperatively. Arthrodesis of the pastern joint was accomplished with three screws placed across the joint to compress it. The cartilage from the pastern joint was removed prior to screw placement. Good healing has occurred.