Baghdad College of Medicine / 5
th
grade
Student’s Name :
Dr. Shatha Al-Kawaz
Lec. 2
Biliary Artresia &
Choledochal cyst
Sun. 25 / 12 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2016 – 2017
Biliary Atresia Dr. Shatha
25-12-2016
2
©Ali Kareem 2016-2017
Biliary atresia
Objective: to learn what is biliary atresia, types, the etiology and
pathogenesis, presentation, how to diagnose and how to treat.
Biliary atresiais a relatively rare obstructive condition of the bile
ducts causing neonatal jaundice.
o It is slightly more common in female than male
o It is more common in Asian countries.
Two distinct forms are described:
1. Syndromic B.A ( embryonic) type account for 10-20% of all cases
associated congenital anomalies are found (interrupted
IVC,preduodenal portal vein , intestinal malrotation , situs inversus,
cardiac defects and polsplenia )
2. Non –syndromic (perinatal).
Etiology and pathogenesis:
Despite the intensive investigation, the cause of B.A remains unknown,
various etiologic mechanisms have been postulated including;
1. perinatal viral infection ; CMV,reovirus type 3 ,rotavirus ,papilloma
virus and Epstein- Barr virus all have been proposed as possible
etiologic agent , but there is no conclusive evidence.
2. Genetic mutation that result in defective morphogenesis may be
important in syndromic B.A
3. Other causes; including vascular or metabolic insult to the
developing biliary tree, immunologically mediated inflammation.
Biliary Atresia Dr. Shatha
25-12-2016
3
©Ali Kareem 2016-2017
Classification and pathology:
Although the term B.Aimplies a static process with complete obstruction or
absence of bile ducts, it is more a dynamic process of progressive bile duct
obliteration and sclerosis.
It is divided into 3 main types; the most common one is type III.
o Early in the course of B.A the liver is enlarged, firm and green.
The gall bladder is small and filled with white mucus, or it may be
completely atretic.
o The biliary tracts contain inflammatory and fibrous cells surrounding
miniscule ducts that are probably remnants of the original duct
system.
o Liver parenchyma is fibrotic and shows signs of cholestasis.
Proliferation of biliary neoductules.
This process develops into end state cirrhosis if good drainage cannot be
achieved.
Biliary Atresia Dr. Shatha
25-12-2016
4
©Ali Kareem 2016-2017
These early changes are not specific to B.A and may be confused with
neonatalhepatitis and metabolic disease.
Physical findings:
o The cardinal sign and symptoms of B.A are jaundice, clay -
colored stools, and hepatomegaly.
o In neonatal period feces are yellow or light yellowish in more than
half of patients.
o The newborn pass dark brown urine.
o Infants with B.A are typically active, full term and may manifest
normal growth and weight in the first few months of life. Anemia,
malnutrition and growth retardation develop gradually because of
malabsorption of fat-soluble vitamins.
o Jaundice that persists beyond 2 weeks of life should no longer be
considered asphysiological, particularly if the elevation in bilirubin
is mainly in the direct fraction.
Diagnosis:
Routine examination
o Color of stool
o Consistency of the liver
o Liver function test
Serum bilirubin (total and direct) conjugated
hyperbilirubinemia ,defined as any level exceeding either
0.2mg/dL or 20%of total bilirubin, infants with B.A typically
show moderate elevation in total bilirubin, which is
commonly 6-12mg/dL with the direct(conjugated) fraction
composing 50-60% of total serum bilirubin
Biliary Atresia Dr. Shatha
25-12-2016
5
©Ali Kareem 2016-2017
Alkaline phosphatase (AP), 5’nucleotidase, gamma-glutamyl
transpeptidase (GGTP), serum aminotransferase, serum bile
acid
o Coagulation time (PT, PTT)
Special examination
Special biochemical studies
o Hepatitis A, B, C serologic studies
o TORCH titer
o α1-antitrypsin level
o Serum lipoprotein-X
o Serum bile acid
Confirmation of patency of extrahepatic bile duct.
o Duodenal fluid aspiration.
o Ultrasonography.
o Hepatobiliry scintigraphy.
o Needle biopsy of the liver for histopathologic studies
o Laparoscopy.
o Surgical cholangiography.
Treatment:
Once B.A is suspected, surgical intervention is the only mechanism
available for a definitive diagnosis (intraoperative cholangiogram) and
therapy (Kasaiportoenterostomy).
Pre operative management:
Biliary Atresia Dr. Shatha
25-12-2016
6
©Ali Kareem 2016-2017
o V K daily
o Oral antibiotics
o Bowel preparation glycerin enema
o Oral feeding is discontinued for 24-72 hours before operation.
Surgical technique
Hepatic Portoenterostmy
Complications:
1. Cholangitis
2. cessation of bile flow
3. portal hypertension
Choledochal cyst
Objectives: to study choledochal cyst, its types, etiology, clinicalfeature,
diagnosis and treatment
.
Choledochal cyst is a congenital dilatation of the biliary tract. The
dilatation can be found along any portion of the biliary tract.
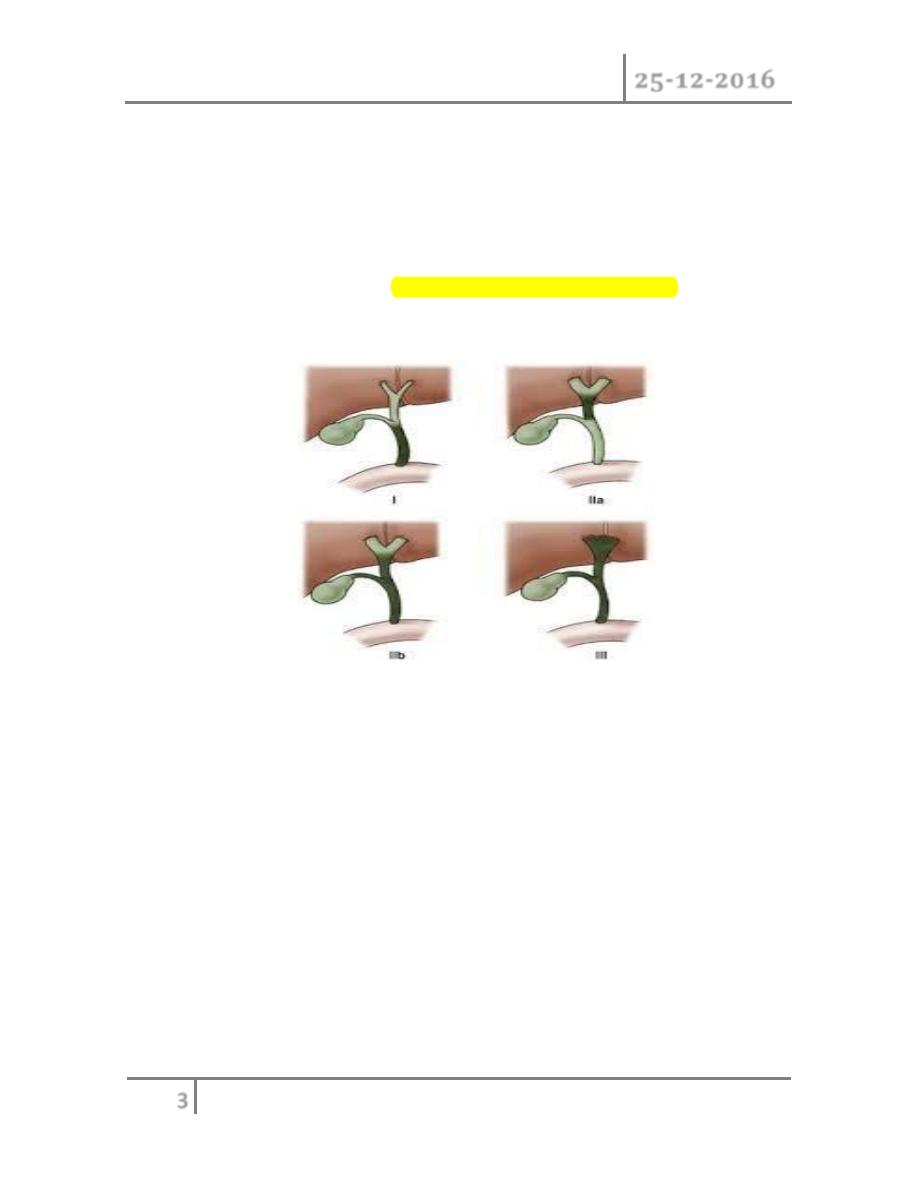
Classification
Choledochalcyst (CC) is classified into five types (Todani's classification):
1. Type I
Biliary Atresia Dr. Shatha
25-12-2016
7
©Ali Kareem 2016-2017
• Ia: cystic dilatation of the CBD
• Ib: fusiform dilatation of the CBD
2. Type II: diverticulum of the CBD
3. Type III: choledochocele (dilatation of the terminal CBD within
the duodenal wall)
4. Type IV
• IVa: multiple cysts of the extrahepatic and intrahepatic ducts
• IVb: multiple extrahepatic duct cysts
5. Type V—intrahepatic duct cyst (single or multiple, as in Caroli
disease).
Type I CCs predominate. Together with type IVa cysts, they account for
more than
90% of cases. Caroli disease is characterized by segmental saccular
dilatation of the intrahepatic bile ducts. It may affect the liver diffusely
or be localized to one lobe.
Etiology
There are many theories to explain the development of a CC. However,
none of these can explain the formation of the formation of the five
different types of CC.
CC either congenital or acquired.
Congenital cysts develop during fetal life,as a result of a prenatal structural
defect in the bile duct.
CC which develops later in life is considered "acquired", the theory of the
long common bilio-pancreatic channel is widely accepted.
Biliary Atresia Dr. Shatha
25-12-2016
8
©Ali Kareem 2016-2017
An inflammatory reaction within the CC is noted in most cases. It is
minimal in infants and gradually becomes more marked as the patient gets
older. The degree of mucosal ulcerations and pericystic inflammation
becomes more severe after repeated bouts of cholangitis. Liver histology
varies from normal to cirrhosis, depending on the patient’s age and degree
of cholangitis
Clinical Features
o Female to male ratio was 3.2 to 1. Clinical presentations differ
according to the age of onset and the type of cyst.
o An abdominal mass or jaundice is a common finding in an infant
with CC, whereas abdominal pain is more often seen in older
children.
o Malignant change is a late complication, mostly seen in adults
Imaging
o Ultrasonography (US) is the initial imaging method ofchoice.
Contour and position of the cyst, the status of the proximal ducts,
vascular anatomy, and hepatic
o echotexture can all be evaluated on ultrasound.
o ERCP allows excellent definition of the cyst as well as the entire
anatomy, including the pancreatobiliary junction. However, this
investigation is invasive and has complications such as pancreatitis,
perforation of the duodenal or biliary tracts, hemorrhage, and
sepsis.
o Magnetic resonance cholangiopancreatography (MRCP) is highly
accurate (96-100%) in the detection and classification of the
Biliary Atresia Dr. Shatha
25-12-2016
9
©Ali Kareem 2016-2017
cystsshould be considered a first choice imaging technique for
evaluation.
o Intraoperative cholangiography is indicated when the anatomic
detail of the biliary tract cannot be demonstrated by MRCP or ERCP
Surgical Techniques
o Cyst excision and a bilio-enteric anastomosis is the preferred
approach for most patients.
Preoperative Preparation
o Biliary infection should be treated before operation
o A prolonged prothrombin time secondary to cholestasis should be
corrected with intravenous vitamin K.
o Bilio-Enteric Anastomosis after Cystectomy,many surgeons use
hepaticojejunostomy, while others prefer hepaticoduodenostomy
o Caroli disease partial hepatectomy is indicated for the localized type
of Caroli disease and liver transplantation is usually needed for
diffuse disease.
Complications included cholangitis, anastomotic stricture, intrahepatic
calculi, and bowel obstruction.
#END of this Lecture …
**Note : For all lectures I do(the previous lectures also) , always check the slides to see
all the pics because the lecture contain some of them.
Best Regards
