0
Dr. Rabab
Chronic Diarrhea
Lec. 3
14
th
Nov. 2016
Done by: Zainab Abdul Ghan
y.
مكتب آشور لالستنساخ
2016-2017
Lec. 15
Pediatrics
1
Bloody diarrhea in infancy and childhood
BD (bloody d.) often indicates serious gastrointestinal disease
1- Intestinal bacterial infection is the most common cause shigella, EIEcoli (Entero-invasive)
Campylobacter, Salmonella, and Yersinia are important in the developed world
Bacterial gastroenteritis is usually self-limiting—antibiotics are needed only in selected
cases.
2- Dysentery: In the developing world other disorders including bacterial (Shigella) and
amoebic (Entamoeba histolytica) dysentery.
3- Inflamatory bowel disease Crohn’s disease and ulcerative colitis often present with
bloody diarrhoea and should be considered in all ages.
4- Cow milk protein allergy.
5- Vasculitis e.g. HSP, SLE.
6- Surgical causes e.g. intussusceptions , malrotation and valvulus ,polyps and hirschprung
dis.
7- Necrotizing enterocolitis.
Bloody diarrhea:
Amebiasis:
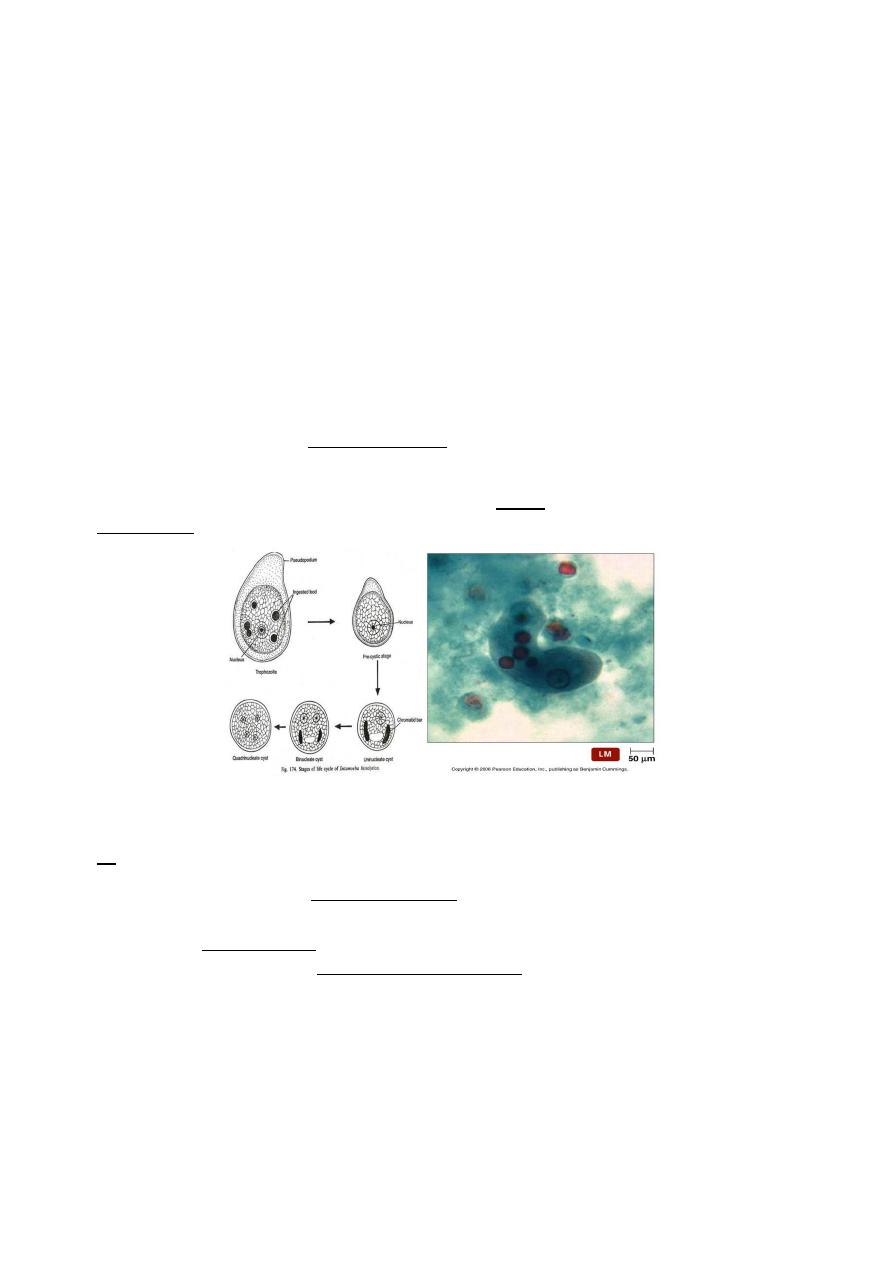
Human infection with Entameba is prevalent worldwide.
Entameba Histolytica is the pathogenic organism in addition to other 5 non-pathogenic
types.
The ingested cyst is resistant to gastric acidity and digestive enzymes, it excysts in the small
intestine to form four trophozoites and colonize the large bowel and may invade the
mucosal lining under conditions which are not known.
Clinical manifestations:
1- Asymptomatic cyst passage in 90% of persons should be treated.
2- Intestinal Amebiasis:
A- IP is 2 weeks – months.
B- Gradual colicky abdominal pains.
C- Bloody mucusy frequent stool, with tenesmus.
D- Fever in 1/3 of cases.
2
3- Amebic colitis:
A- Mostly in the age of 1-5 years.
B- Sudden onset of fever, chills.
C- Severe diarrhea leading to dehydration & electrolyte disturbance.
4- Toxic mega colon or local perforation and peritonitis.
5- Hepatic Amebiasis: Hepatomegaly, liver abscess occurs in <1% of infected individual or
even in no previous infection. Fever, chills, elevation of the diaphragm with effusion or
atelactasis.
Diagnosis:
It is based on detecting the organisms in stool
Samples, Sigmoido-scopically obtained smears, tissue biopsy samples or rarely aspirate
from liver abscess. The trophozoites should be seen motile and containing the
erythrocytes.
Treatment:
All individuals with EH trophozoites or cysts should be treated.
For invasive Amebiasis: oral Metronidazole 50 mg/kg /day in three divided doses. for
10 days
For cysts: oral Diloxanide 20mg/kg/day in 2 divided doses for 10 days.
For amebic liver abscess intravenous metronidazole 7 mg /kg 8 hourly.
3
PATHOGENESIS OF PERSISTENT DIARRHOEA
final common pathway to persistent diarrhea is prolonged small intestinal mucosal injury
or PSIMI (post enteritis syndrome).PSIMI is caused, intensified and perpetuated by the
following factors:
1. Malnutrition
2. Ineffective villous repair.
3. Persistent infection with one or more enteric pathogens.
4. Malabsorption of nutrients, especially carbohydrates and fats.
5. Increased absorption of foreign proteins.
6. Deficient enteric hormones.
All these factors contribute to the vicious cycle of mucosal injury and malabsorption,
leading to PD
INCREASED ABSORPTION OF FOREIGN PROTEINS
In PD, the small bowel mucosa is damaged and hence large protein molecules are
absorbed intact into the blood-stream.
This leads to the formation of circulating immune complexes that aggravate PSIMI.
Classic examples of this phenomenon are cows milk protein intolerance and soya
protein intolerance
Chronic diarrhea in infants
1- Carbohydrate intolerance and Post-infectious secondary lactase deficiency.
2- Coeliac disease.
3- Cow’s milk allergy.
4- Toddlers diarrhea.
5- Infections as giardiasis and HIV.
6- Cystic fibrosis.
7- Acrodermatitis enteropathica
4
Carbohydrate intolerance
Primary Congenital lactose intolerance:
Glucose-galactose malabsorption. Very rare, usually starts early with watery, explosive
diarrhea and failure to thrive. Reduced substance in stool is positive.
Secondary lactose intolerance
Usually post-infectious (Rota virus). Bloating, abdominal discomfort and flatulence that
occur from 1 hour to a few hours after ingestion of milk or dairy products may signify
lactose intolerance.
Stool characteristics: Loose, watery, acidic stool often with excessive flatus and
associated with urgency that occurs a few hours after the ingestion of lactose-
containing substances is typical.
Investigations
1- Reducing substances in the stool is positive.
2- The stool is acidic with PH <5.5.
3- Breath hydrogen test: Carbohydrate malabsorption results in bacterial fermentation of
the unabsorbed sugar. Thus, carbohydrate malabsorption can be determined by
measuring the exhaled hydrogen concentration after a carbohydrate load is
administered.
MANAGEMENT Lactose free diet.
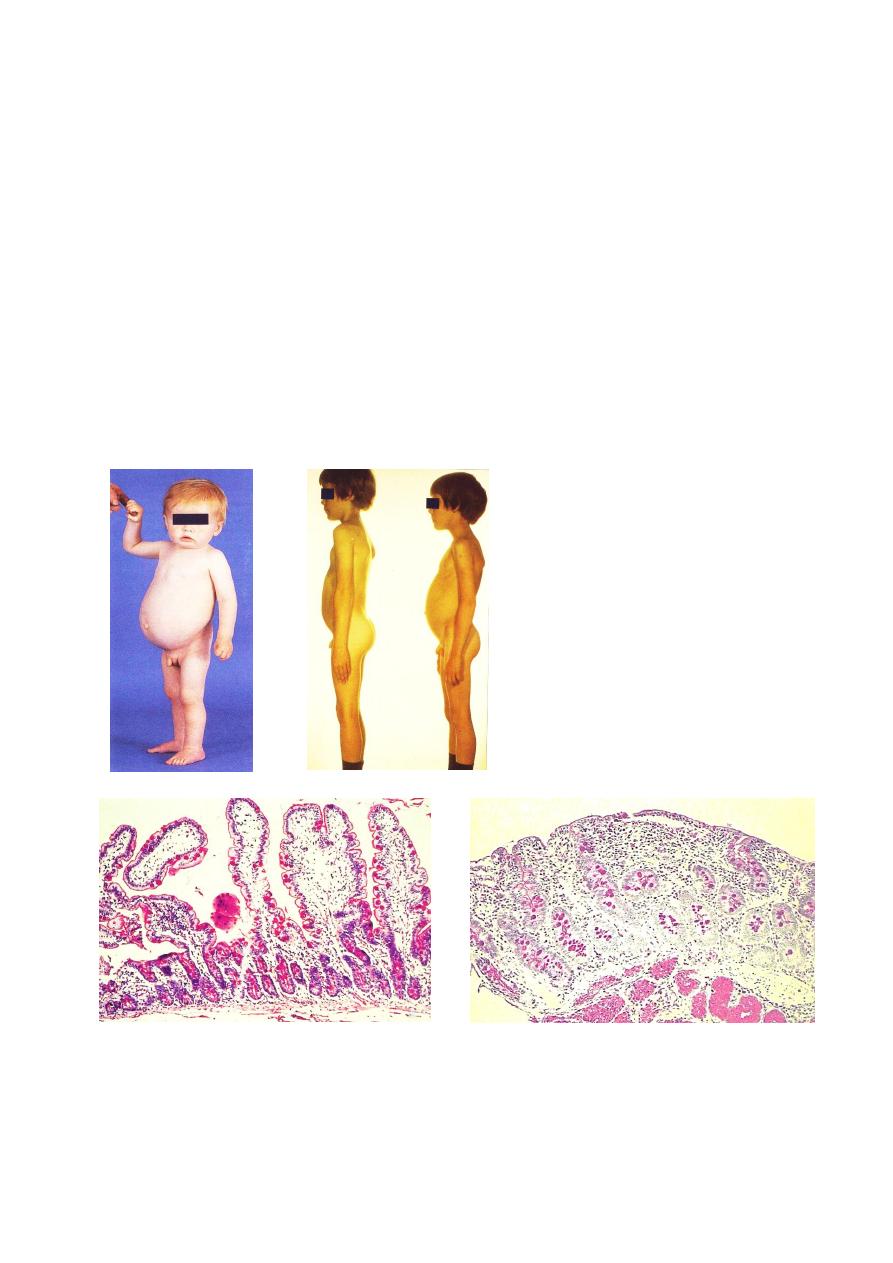
Celiac Disease:
It is an immune mediated inflammatory condition of the proximal small intestinal mucosa
with permanent intolerance to dietary gluten cereals as wheat, rye and barley.
Etiology:
Celiac disease is multifactorial dis. Involving genetic & immunological susceptibility factors
triggered by dietary antigens & other possible envir. factors.
It is the Prolamins which presented in the Gliadin of the gluten which is the toxic fraction.

5
Patterns of presentation:.
A- Classical:
1- Usually presented at 6-18 months.
2- There is a variable period between introduction of gluten & appearance of the
symptoms, breast feeding may delay the disease.
3- Diarrhea may be acute or insidious.
4- Stool is pale, foul offensive smell, large in amount.
5- Failure to thrive & anorexia.
6- Short stature, abdominal distention and sometimes vomiting.
On Examination:
1- Wasting especially in the proximal parts (hip girdle) with increase wrinkling of the skin.
2- Sore throat & smooth tongue.
3- Excessive bruising.
4- Clubbing of the fingers & peripheral edema.
5- No wt. gain .Wt. & Ht. are below the third centile.
6- Iron def. & megaloblastic anemia.
Genetic factors:
Gluten enteropathy is associated with histocompatibilty of HLA DQ2,
HLA DQ8.
HLA DQ2 occurs in more than 90% of celiac pt.
It has Familial tendency.
Incidence: 1/3000- 1/6000.
Diabetes Mellitus & Dermatitis Herpitiformis is commonly ass.
with Gluten sensitivity.
B- Below 9 months of age:
1- Acute onset of vomiting.
2- Severe diarrhea.
3- Abdominal distention.
4- Hypotonia.
5- Growth retardation.
6
C- constipation:
1- Severe anorexia.
2- Hypotonia.
3- Marked abdominal distention.
D- Older children:
1- Short stature.
2- Delayed puberty.
3- Severe iron def. anemia.
4- Rickets.
5- Personality changes.
6- No obvious GIT symptoms.
E- Asymptomatic sibling:
No symptoms, only discovered if there is an index case in the family.
The typical finding in the second part duodenal biopsy are:
1- Total or subtotal villous atrophy.*
2- Crypts hyperplasia. (Increase no. of crypts).
3- Chronic inflammatory cell infiltration. (lympho. Plasma cells)
4- Increase intra epithelial lymphocyte. (> 30/100).
** The definitive diagnosis is by typical biopsy + serology and the follow up is by serology
* Subtotal villus atrophy can be seen also in:
1- Cow milk protein allergy.
2- IgA deficiency.
3- Familial villous atrophy.
4- Eosinophilic gastroenteritis.
Differential diagnosis of Celiac disease:
1- Giardiasis.
2- Acute viral diarrhea with Lactose intolerance.
3- Autoimmune enteropathy.
4- Stagnant loop syndrome with bacterial overgrowth.
5- Cow milk protein intolerance.
6- Familial villous atrophy (enteropathy).
7- IgA def. ( usually since birth).
7
Complications:
1- Protein losing enteropathy and edema.
2- Dimorphic anemia.
3- Growth retardation and delay puberty.
4- Bleeding tendency.
5- Celiac crisis.(severe dehydration ,shock & severe hypokalemia).
6- Long standing Celiac may lead to Lymphoma.
Treatment:
1- Gluten free diet.
2- Symptomatic treatment for anemia, hypo-albuminemia and any superadded infection.
3- Longlife follow up of the patient for compliance & growth measurements.

8
Cow’s milk protein allergy
Usually starts during the first year when children are given milk products. Typical symptoms
are Vomiting, diarrhea, colic and constipation may occur. Other rare presentations are
wheezes, cough, atopic eczema and behavioral changes like irritability, crying and milk
refusal.
A challenge with milk free times may have a good indicators. However, histopathological
examination is a diagnostic test
Toddlers diarrhea Called (chronic non-specific diarrhea of childhood):
It is a common problem. Occurs to children mainly above 2 years. It is a benign condition.
Usually, the children have no failure to thrive and they present in a good nutritional state.
Abdominal pain may be present in a minority.
The stools are foul smelling, watery, and contain mucus with undigested vegetable
material. The parents are likely to report a short mouth to anus transit time.
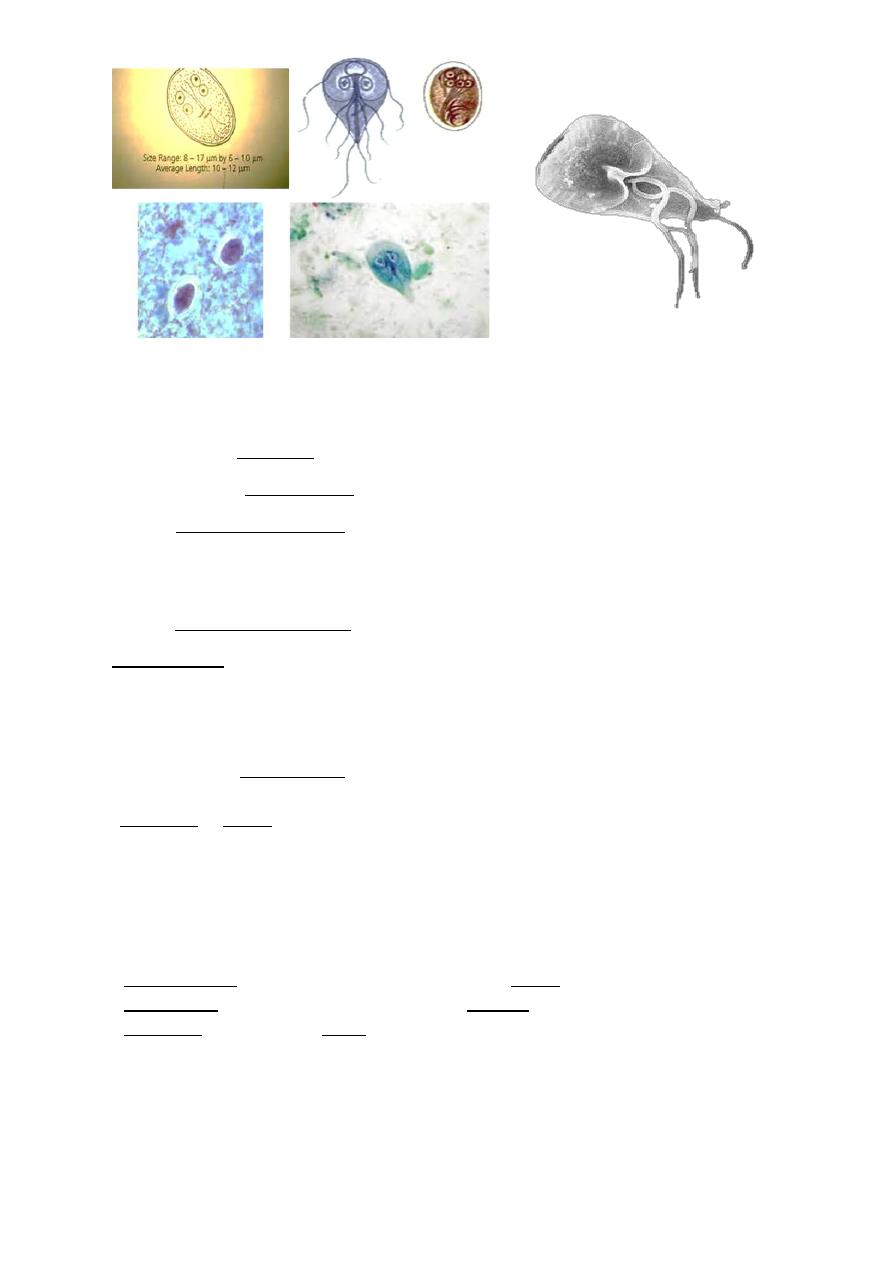
Giardiasis:
Giardia lamblia is a flagellated protozoan that infects the duodenum & small intestine. Wide
range of clinical manifestations results from asymptomatic, acute, chronic diarrhea and
even malabsorption status.
Infection is more common in children than adults.
Etiology:
Ingested cyst produces 2 trophozoites in the proximal small intestine (They attach to the
brush boarder of the intestinal epithelial cells & multiply by binary fission). The body is tear
drop shaped, measuring 10-20 microml in length & 5-10 microml in width. It contains 2
ovals nuclei anteriorly and four pairs of flagella.
The detached trophozoites pass down the intestinal tract and become encysted and
contains 4 nuclei, passed in the stool. Viability is not affected by the usual concentrations of
chlorine used to purify water for drinking.
Person to person spread by fecal- oral contact & crowding.
Giardia is a particularly significant pathogen in people
with malnutrition, immune
deficiencies, and cystic fibrosis.
9
Clinical manifestations:
Incubation period: 1-2 weeks.
1- The child may be asymptomatic,
2- Or have acute watery diarrhea, may be fever, nausea and anorexia.
The stool initially may be profuse watery and later become greasy and foul smelling and
may float, or constipation or normal bowel motion.
3- Signs of fat soluble vitamin def.
4- Malabsorption of sugars, fat and wt. loss.
Diagnosis:
1- Repeated fresh Stool samples examination for the trophozoites, cysts, or Giardia
antigens in stool or duodenal fluid.
2- Aspiration or biopsy of the duodenum or upper jejunum.
3- Blood count is normal.
4- No Eosinophilia in giardiasis.
Treatment:
Metronidazole: 15-25mg/kg/day divided doses for 5 days.
Furazolidine: 6mg /kg/day divided doses for 10 days.
Tinidazole: 30 mg/kg/day single- dose therapy.
10
Cystic fibrosis
AR disorder.Due to abnormal chlorid transport, most patients have respiratory symptoms
as recurrent pneumonia, and adenoid. Those patients have pancreatic insufficiency which
lead to diarrhea with greasy stool. Failure to thrive.
Genetic diagnosis and sweat chloride test are the main investigations
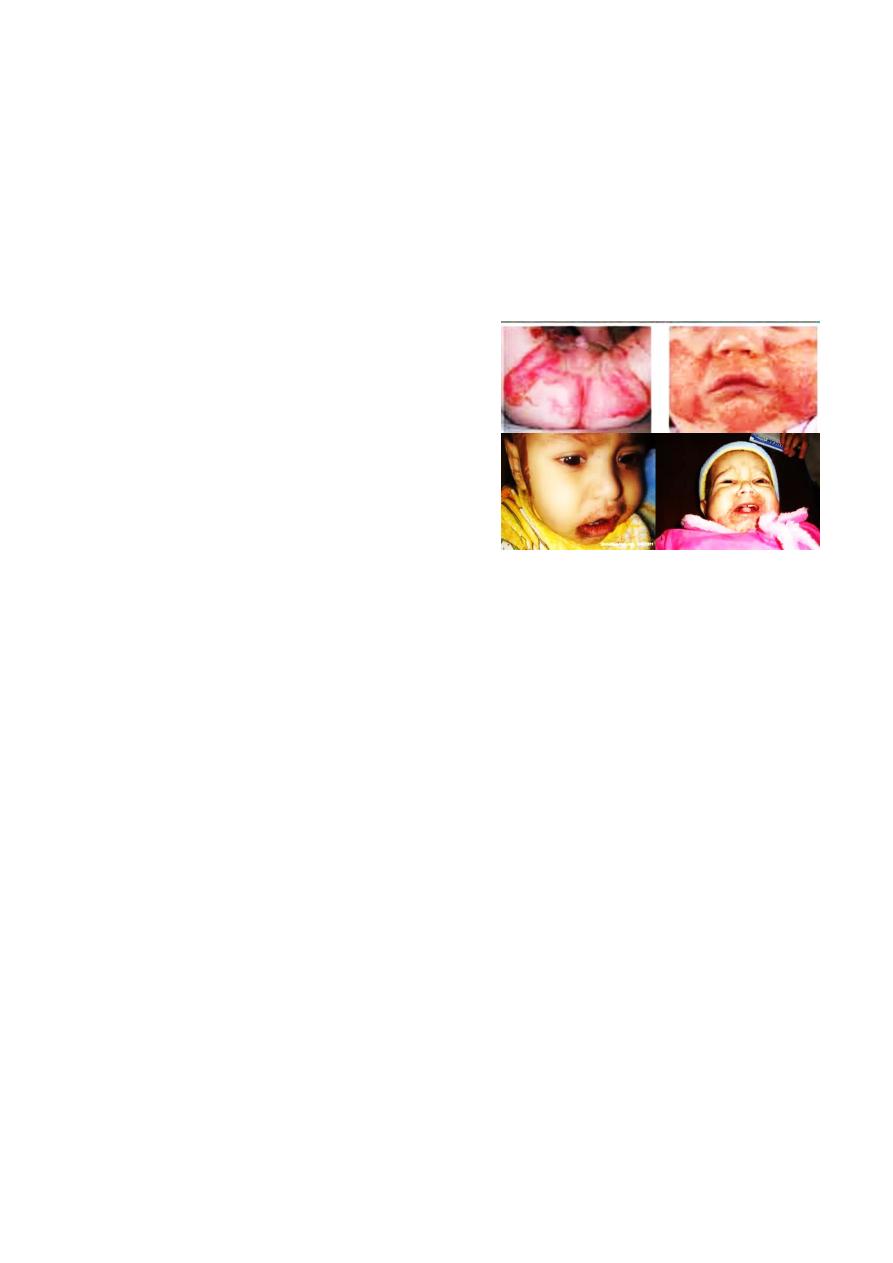
Acrodermatitis enteropathicaa
AR disorder. Abnormal absorbtion of zn ,child
Presents with peri-oral rash, chronic diarrhea,
recurrent infection and napkin rash resistant to
treatment. Usually starts at the time of weaning.
Tent red hair and alopecia.
Diagnosis: Serum Zink in the WBCS OR IN THE
BLOOD.
Management: Serum Zink.
Chronic diarrhea in infants
1- Carbohydrate intolerance and Post-infectious secondary lactase deficiency.
2- Coeliac disease.
3- Cow’s milk allergy.
4- Toddler's diarrhea.
5- Infections as giardiasis and HIV.
6- Pseudo-memberanous colitis.
7- Cystic fibrosis.
8- Acrodermatitis enteropathica
Chronic diarrhea in older children Common causes
1- Post-enteritis syndrome.
2- Coeliac disease.
3- Lactose intolerance.
4- Infections as giardiasis and HIV.
5- Pseudo-memberanous colitis.
6- Irritable bowel syndrome.
7- Inflammatory bowel disease.

11
Post enteritis syndrome
Persistent diarrhea after gastroenteritis is caused by Continuing infection. Further infection.
Carbohydrate intolerance. Post infection malabsorption syndrome. Usually subsides, but
severe cases may persist to longer periods. Stool analysis and stool culture. Treatment of
the cause.
Pseudo-membranous colitis
Also called antibiotic-associated colitis or C. difficile colitis, is inflammation of the colon
associated with an overgrowth of the bacterium Clostridium difficile (C. diff).
This overgrowth of C. difficile is most often related to recent antibiotic use
Inflammatory bowel disease
This is of two types Crohn’s disease and ulcerative colitis. 20%% of cases presents under 20
years old. It has intestinal and extra intestinal manifestations.
Clinical picture: Diarrhea, Abdominal pain, Growth deceleration, Weight loss & Anorexia.
Colonic Crohn disease may be clinically indistinguishable from ulcerative colitis (UC), with
manifestations that include the following:
• Bloody mucopurulent diarrhea
• Cramping abdominal pain
• Urgency to defecate
Perianal involvement in Crohn disease may produce the following:
Simple skin tags, fissures, abscesses, and fistulae
Painful defecation •Bright-red rectal bleeding
Perirectal pain, erythema, or discharge
Examination:
Growth is impaired. Intermittent fever. Tachycardia. Mouth ulcers. Anal tags. Arthritis.
Erythema nodosum. Pyoderma gangeriosum. Tanner staging is important.

12
Investigations:
BLOOD:
CBC, anemia, ESR and CRP
Elevated, Hypo-albuminaemia.
Imaging studies:
A single-contrast upper GI radiologic series with small-bowel follow-through (SBFT).
Endoscopy:
Colonoscopy with several colonic and terminal ileal biopsies is considered a standard
diagnostic procedure.
Upper endoscopy, or esophago-gastro-duodeno-scopy (EGD), should be part of the
first-line investigation.
Video capsule endoscopy is increasingly being used to evaluate for small-bowel Crohn
disease in children
Step-up approach, Patients with mild disease are treated with preparations of 5-
aminosalicylic acid (5-ASA), antibiotics, and nutritional therapy if no response occurs or if
the disease is more severe than was initially thought, corticosteroid and
immunomodulatory therapy Surgery is considered when medical therapy fails
Indications for surgery include the following:
Intractable disease with growth failure
Obstruction or severe stenosis
Abscess requiring drainage
Perianal fistulae Intractable hemorrhage
Perforation
13
هذه المواضيع موجودة في محاضرة العام فقط لكن الدكتورة شرحتها:ةظحلام
Persistent Diarrhea:
Definition: It is the diarrhea that started by either acute or bloody diarrhea and lasted
more than 14 days.
Here we may recover microorganism or its sequel.
The danger of this type of diarrhea is Dehydration, electrolyte disturbances, metabolic
acidosis or Sepsis and eventually malnutrition.
The various risk factors for persistent diarrhea
(Persistent or protracted) starts as acute diarrhea, but continues more than 2 weeks. Risk
factors are:
1. Protein-energy malnutrition
2. Younger age < 18 months
3. Lack of breast-feeding
4. Prolonged IVF therapy & delayed enteral feeding
5. Cows milk .Soya protein
6. Inappropriate use of antibiotics
7. Improper therapy of ADD.
8. Use of anti motility drugs like loperamide.
9. Starvation during ADD.
10. Vitamin A deficiency.
11. Zinc deficiency.
12. Poor hygiene leading to reinfection.
13. Certain extra intestinal infections, e.g., septicemia, UTI
ROLE OF MALNUTRITION IN PSIMI
Normally, in the epithelium of the small bowel, absorptive cells are continuously lost
from the villous tip and replaced by newer cells produced by the crypts of Lieberkuhn,
once in 4-5
In a child with malnutrition, the production of the absorptive cells of the villi is
decreased, as it requires energy and nutrients.
These cells are responsible for the synthesis of disaccharidase enzymes like lactase and
hence their concentration in the gut decreases. This leads to osmotic diarrhoea.
The absorption of nutrients, which also requires energy, is decreased in malnutrition,
Malnutrition can depress the immune functions, leading to infections of the gut .
Gastrin and cholecystokinin are proteins in nature, their secretion is decreased in
malnutrition.
Gastric HCI and pancreatic enzymes are also decreased leading to maldigestion and
diarrhoea
14
Bacterial contamination of the small gut causes PSIMI by the following mechanisms:
1- Release toxins
2- Directly invade and damage the small bowel mucosa > malabsorption
3- Deconjugate bile acids,
releasing free bile acids in the small gut.
Example stugnant loop syndrome
Diagnosis:
1- Total WBC count & def.
2- General stool examination: It may show pus cells & RBC.,PH usually acidic <5.5. &
reducing subs is positive.
3- Stool culture & sensitivity.
4- Urine C&S.
5- ELISA test for Rota virus.
6- Blood C&S.
Management:
1- Rehydration in case of dehydration.
2- Nutritional rehabilitation & changing the milk to a therapeutic formula (Lactose free,
Sucrose free …) if the child is too weak to suck or anorexic, NG tube feeding with gradual
increase in the amount is the best management.
3 -In case of cow milk protein intolerance or allergy we give Soya based formula or Goat
milk in case of allergy to Soya for at least 6-8 weeks ( until regeneration of the int. villi.)
4- Treating infection if present according to the sensitivity.
5- Give Vitamins and Zinc (20 mg daily for 2 weeks).
6- Pre and probiotics (e .g. lactobacillus bifidus bacteriae).
THANK YOU
EDITED BY: ZAINAB ABDUL GHANY.
