gynecology
oj
kk
Dr. Maad
ملحق محاضرة
3
Done by :
Ali Faleh
2016-2017
مكتب اشور لالستنساخ
1
By : Ali faleh
) دكتور معد3 ةرضاحم قحلم)
Endometritis
A- acute (apart from infections acquired at operations and by instrumentation) it is
either: puerperal or gonococcal
B- chronic:
T.B
Senile
other causes
The regrowth of new surface of endometrium during each cycle prevents the
persistence of any infection (rendering the infection from becoming deep seated) so
this disease rarely occurs in the period between the menarche and menopause
It occurs when the uterus is permanently injured or when there is a chance for the
infection to persist. for example:
foreign body
Malignant disease of the uterus
Infected polyp
Retained gestational products
Chronic salpingio-oopheritis
Pelvic cellulitis after radiation
Endometrial burn secondary to radiation
Microscopically
there is a large collection of plasma cells
Clinical features:
purulent discharge from the uterus + menorrhagia
IN ANY SIGNS OF INFCETION SEND FOR CULTURE TO EXCLUDE T.B
Treatment:
find the cause and treat accordingly. If there is a wide spread infection
then the treatment is by hysterectomy
Senile endometritis :
with aging, the endometrium loses its resistance and will not be shed
repeatedly, so it will be more liable for the development of endometritis. It may be
associated with senile vaginitis.
2
By : Ali faleh
The endometrium becomes infiltrated by macrophages known as foam cells, the
epithelium becomes destroyed leading to granulation tissue formation and pus
exudation which if accumulate in the cavity can lead to pyometra. Because the cervix
is narrow due to senility there will be atrophied myometrium.
The uterus is enlarged and thin, pyometra may cause squamous metaplasia or rarely
rupture spontaneously.
Clinical features:
very offensive purulent post menopausal discharge, sometimes bloody stained.
may present as intermittent discharge
uterus is enlarged
Differential Dx:
1. Ca of the uterus
2. if there is pyometra then dilatation of the cervix is required that leads to
drainage of the pus + antibiotics for 1-2 weeks and then do curettage for DD
Treatment
: if the patient is fit for surgery then do hysterectomy after exclusion of Ca
UTERINE POLYPS
1. ENDOMETRIAL POLYPS:
usually multiple and may be a part of hyperplastic
endometrium. At menopause, endometrial polyps are single or few in number.
Pathology:
small pink pale mass projecting from the endometrium, sometimes
having a long stalk that makes it project through the cervix or the vulva. Atypical
cellular changes or squamous metaplasia can occur which may predispose to
adenocarcinoma.
2. FIBROID POLYPS:
sub mucosal fibroids can protrude in to the cavity or pass
through the cervix into the vagina. Its surface is covered by endometrium, it causes
spasmodic dysmenorrhea and menorrhagia.
3. ADENOMATOUS POLYPS (
Contains smooth muscles + endometrial elements)
3
By : Ali faleh
Usually coexist with adenomyosis, causing heavy but regular menses with
cramping, sometimes causing intermenstrual spotting. Can predispose to malignant
changes too.
Placental polyp:
It is rare condition that occurs due to organization of small
retained pieces of placental tissue. it cause intermenstrual bleeding, treatment is by
excision (send for biopsy) but it may cause severe hemorrhage on removal.
Asherman΄s syndrome:
When there is damage of the whole thickness of
endometrium, i.e. beyond the basal layer. it is caused by :
1. excessive curettage for retained products, after miscarriage or for 2ndry PPH
2. T.B, schistosomasis
3. endometrial resection (ablation)
It cause fibrosis and adhesion and the patient represents with hypomenorrhea,
amenorrhea or infertility.
Treatment:
Resection by hysteroscopy + inert IUCD + HRT
Uterine fibroid (Uterine leiomyoma)
is a benign tumor composed of uterine muscles plus fibrous connective tissue
.
It is common and present in 20% of all females. It is more in Negros than in white
women
It is of unknown cause and may be found outside the uterine organs (Vagina,
broad ligament, vulva)
Female sex hormones have been incriminated as a cause because it rarely
appears before puberty and after menopause. In addition, there is a rapid growth
during pregnancy, and is frequently seen in conditions associated with
hyperestrogenism that are not antagonized by progesterone like anovulation,
endometrial Polyps, and endometrial hyperplasia.
Grossly:
It is a firm round tumor of hypertrophied uterine wall. It has a pseudo
capsule which differentiates it from adenomyosis. Since its blood supply is peripheral,
the center is susceptible to degenerative changes.
Cross section of the tumor reveals a solid, smooth, pinkish or white surface with
whorl- like appearance.
4
By : Ali faleh
Microscopically:
It is composed of groups & bundles of smooth muscles in a
twisted whorl fashion, with some connective tissue .
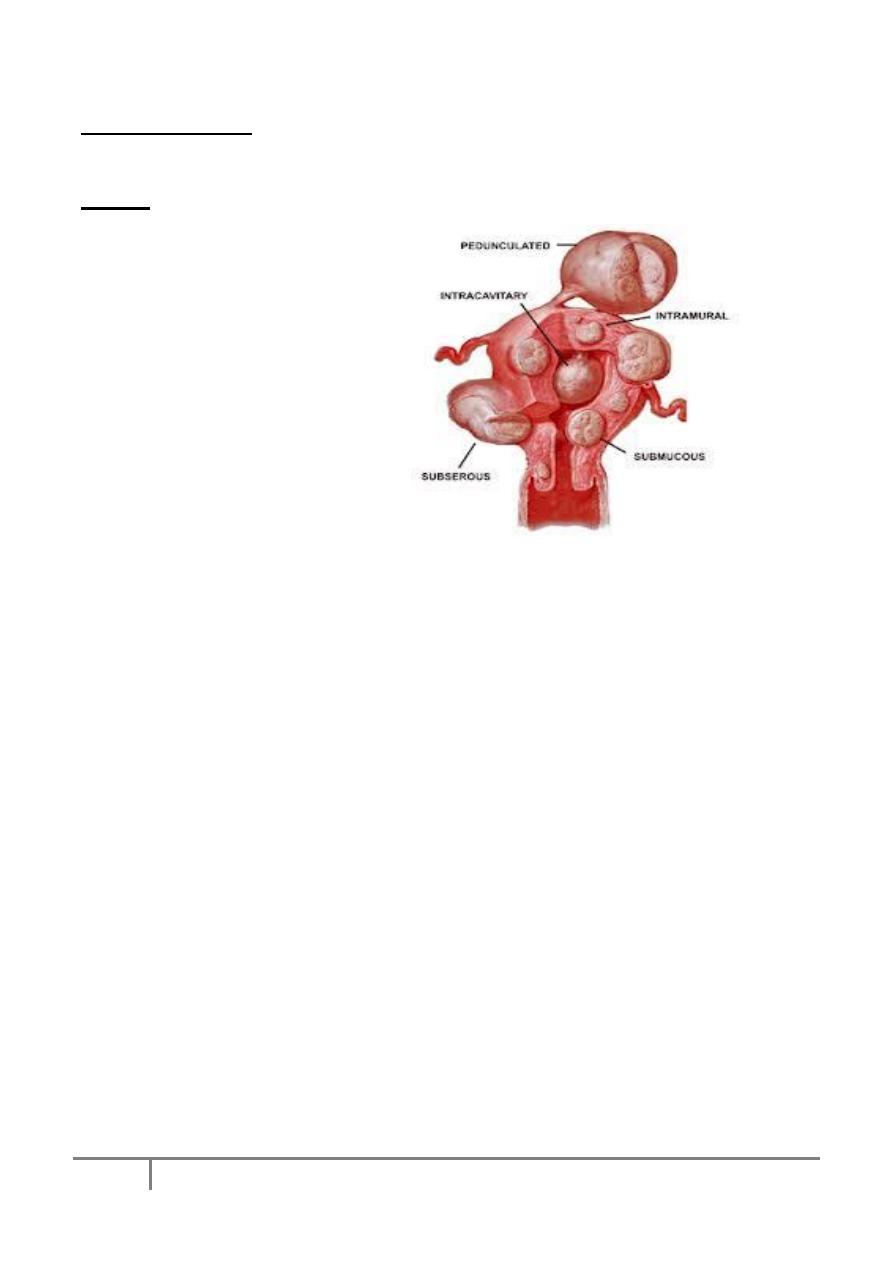
Types:
1) Intramural (the commonest)
2) Sub
serous
myomas:
projecting
towards
the
peritoneal cavity ± pedicle
may
reach a large size without
producing symptoms
3) Interligamentory tumor
4) Sub mucosal
5) Cervical
Fibroids may be single or multiple
The clinical presentation depends on the size, number and location of the fibroid and
could be one of the following:
1) Symptomless: discovered accidentally.
2) Abnormal uterine bleeding: heavy and prolonged.
It may be due to enlargement of uterine cavity by submucous fibroids, increased
vascularity of the tumor, or due to necrosis of endometrium overlying the
submucous myoma. Frequently, myomas may be associated with polyps and
endometrial hyperplasia.
3) Inter menstrual bleeding in case of submucus fibroid
4) pain
a) reappearance of dysmenorrhea (congestive type) due to increase
vascularity
b) Backache incase of posterior fibroids of moderate size with retroversion
c) Colicky pain in case of sub mucous uterus
d) can be caused by torsion
5) Degenerative changes
6) Abdominal distention
7) Pressure symptoms which include:
edema due to pressure on vena cava
urinary frequency due to pressure on bladder
dyspnea
5
By : Ali faleh
Degenerative changes of uterine fibroids:
Occur due to arterial, venous, secondary infections or malignant transformation. There
are several types:
1) Hyaline degeneration:
Here the tumor becomes soft and jellylike, the cells fuse together and
form a structureless esonophilic mass.
2) Cystic degeneration: Liquefaction may occur after menopause leading to
cystic cavity formation.
3) Red degeneration (Necrobiosis): could be diffuse or local. Usually occurs in
pregnancy or near menopause that leads to a fibromyomatous pattern.
Pathology: There is thrombosis of peripheral vessels with absence of cell nuclei.
The blood vessels are distended with thin wall and are engorged with R.B.C.s.
Thus the tumor is stained red and resembles raw meat.
It gives a fishy odor on cutting due to presence of fatty acids. Cystic
degeneration may occur in the center and the cyst becomes full with greasy
brown debris.
4) Fatty degeneration
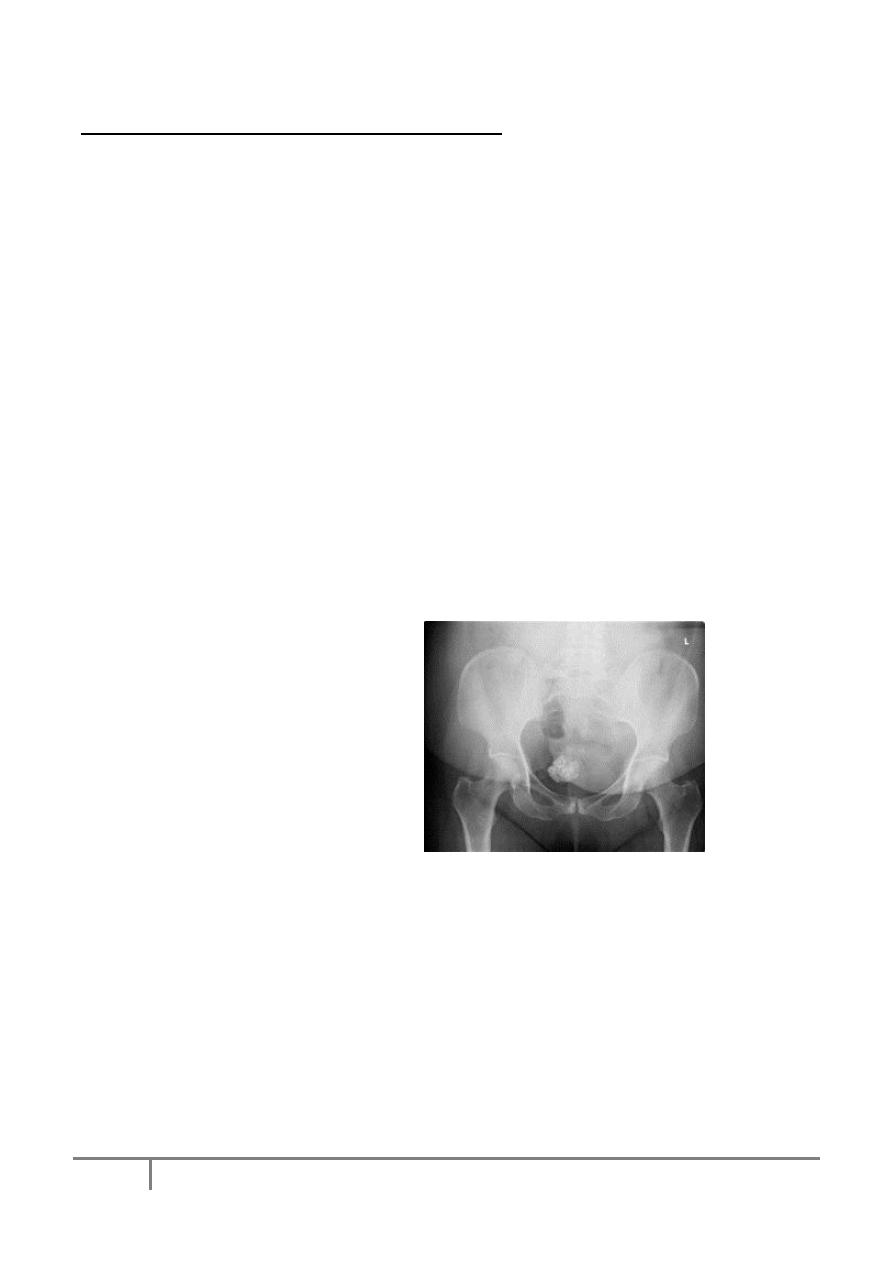
5) Calcifications: Fat may be
deposited
in fibroid which undergoes
saponification. Co3 and Po4 in
blood
react with the soppy mass
leading to
deposition
of
CaCo3
and
calcium
phosphate
Grossly:
It
has
a
gritty
appearance on cross section
A thin peripheral shell can be
seen by X
-ray
In addition to degenerative changes, complications of fibroids include:
Sarcomatous (malignant) changes Sarcomatous changes that occur in 0.5% of
fibroids, 2/3 of sarcoma of the uterus arise from uterine fibroids.
Necrosis
Infection
Atrophy
Torsion
6
By : Ali faleh
Differential diagnosis (of an abdominal mass)
o
Pregnancy
o
Ovarian tumor
o
Endometrial or cervical polyp
o
Adenomyosis
Treatment
A.
Conservative for small and asymptomatic fibroid.
o
Frequent U/S every 6 months.
o LH RH agonist
B.
Surgical
o
Myomectomy either by laparotomy or laparoscopy
o
Hysterectomy
o
Uterine artery embolisation
Endometrial hyperplasia:
Endometrial hyperplasia is when the endometrium becomes too thick. It is not
cancer but it can lead to cancer formation in some cases.
Etiology:
Endometrial hyperplasia most often is caused by excess estrogen without
progesterone. If ovulation does not occur, progesterone is not made, and the lining is
not shed. The endometrium may continue to grow in response to estrogen. The cells
that make up the lining may crowd together and may become abnormal (This is called
Hyperplasia).
Factors predisposing to endometrial hyperplasia:
Postmenopausal women, when ovulation stops and progesterone is no longer
made. It can also occur during perimenopause, when ovulation may not occur
regularly.
Long-term use of high doses of estrogen after menopause (in women who have
not had a hysterectomy) or estrogen like drugs.
Irregular menstrual periods, especially associated with polycystic ovary
syndrome or infertility
7
By : Ali faleh
Other risk factors include:
Age older than 35 years
White race
Never having been pregnant
Early onset of menarche
Personal history of certain conditions, such as diabetes mellitus, polycystic
ovary syndrome, gallbladder disease, or thyroid disease
Cigarette smoking
Family history of ovarian, colon, or uterine cancer
Obesity
Types of endometrial hyperplasia
Endometrial hyperplasia is classified as simple or complex. It is also classified
by whether certain cellular changes are absent or present as typical or atypical
respectively. These terms are combined to describe the exact kind of hyperplasia:
Simple hyperplasia
Complex hyperplasia
Simple atypical hyperplasia
Complex atypical hyperplasia
Clinical presentation:
The most common sign of hyperplasia is abnormal uterine bleeding.
o Bleeding during the menstrual period that is heavier or lasts longer than usual
o Menstrual cycles that are shorter than 21 days (counting from the first day of
the menstrual period to the first day of the next menstrual period)
o Any bleeding after menopause
Diagnosis:
o Transvaginal ultrasound may be done to measure the thickness of the
endometrium.
o Endometrial biopsy, dilation and curettage, or hysteroscopy is done in cases
suspicious of malignancy.
8
By : Ali faleh
Treatment:
many cases are treated with Progestin (orally, in an intrauterine device, or as a
vaginal cream). Duration of treatment depends on the age of the patient and the
type of hyperplasia.
Treatment with progestin may cause vaginal bleeding resembling menstruation.
If there is atypical hyperplasia, especially complex atypical hyperplasia, there is
an increased of cancer so Hysterectomy is done. It is the best option for those
who do not want to conceive.
Prevention of endometrial hyperplasia:
Estrogen treatment after menopause should be combined with progestin or
progesterone.
If there is irregular menstrual period combined oral contraceptive pills may be
recommended.
Decrease weight if obese.
