
MEDICINE
haematology
oj
Lec.05
Dr.Ali M. Jawad
Acute Leukemia, Chronic
Leukemia
Lec . 5
9/3/2017
Done by : Taher Ali Taher
2016-2017
مكتب اشور لالستنساخ
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
1
By : taher ali taher
Objectives
By the end of this lecture, the student should be able to:
1-recall a broad classification of hematological malignancies.
2-describe the types, clinical presentation and diagnosis of acute leukemias
and principles of treatment.
3-describe the types, clinical presentation and diagnosis of common chronic
leukemias and principles of treatment.
Case Scenario
A 23 year old man presented with 3 weeks history of intermittent fever,
increasing pallor and repeated epistaxis.
His clinical examination revealed him to be febrile, pale, with multiple
cervical lymph nodes, multiple ecchymoses and slightly enlarged spleen.
What is your differential diagnosis?
Introduction to leukemia
Leukemia is a malignant disease characterized by unregulated proliferation of
one cell type.
- It may involve any of the cell lines or a stem cell common to several cell lines.
- Leukemias are classified into 2 major groups
o Acute in which the onset is usually rapid, the disease is very aggressive,
and the cells involved are usually poorly differentiated (blast cells)
o Chronic in which the onset is insidious, the disease is usually less
aggressive, and the cells involved are usually more mature cells
2008 WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues
Basic principle: Classification for all neoplasms based on:
Morphology and biologic features
Genetic
Immunophenotype
Clinical features
Introduction to leukemia :-
Both acute and chronic leukemias are further classified according to the cell
origin whether it is myeloid or lymphoid :
- If the prominent cell line is of the myeloid series it is a myelocytic
leukemia (sometimes also called granulocytic)
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
2
By : taher ali taher
- If the prominent cell line is of the lymphoid series it is a lymphocytic
leukemia
TAHA ABBAS
Therefore, there are 2 basic types of leukemia
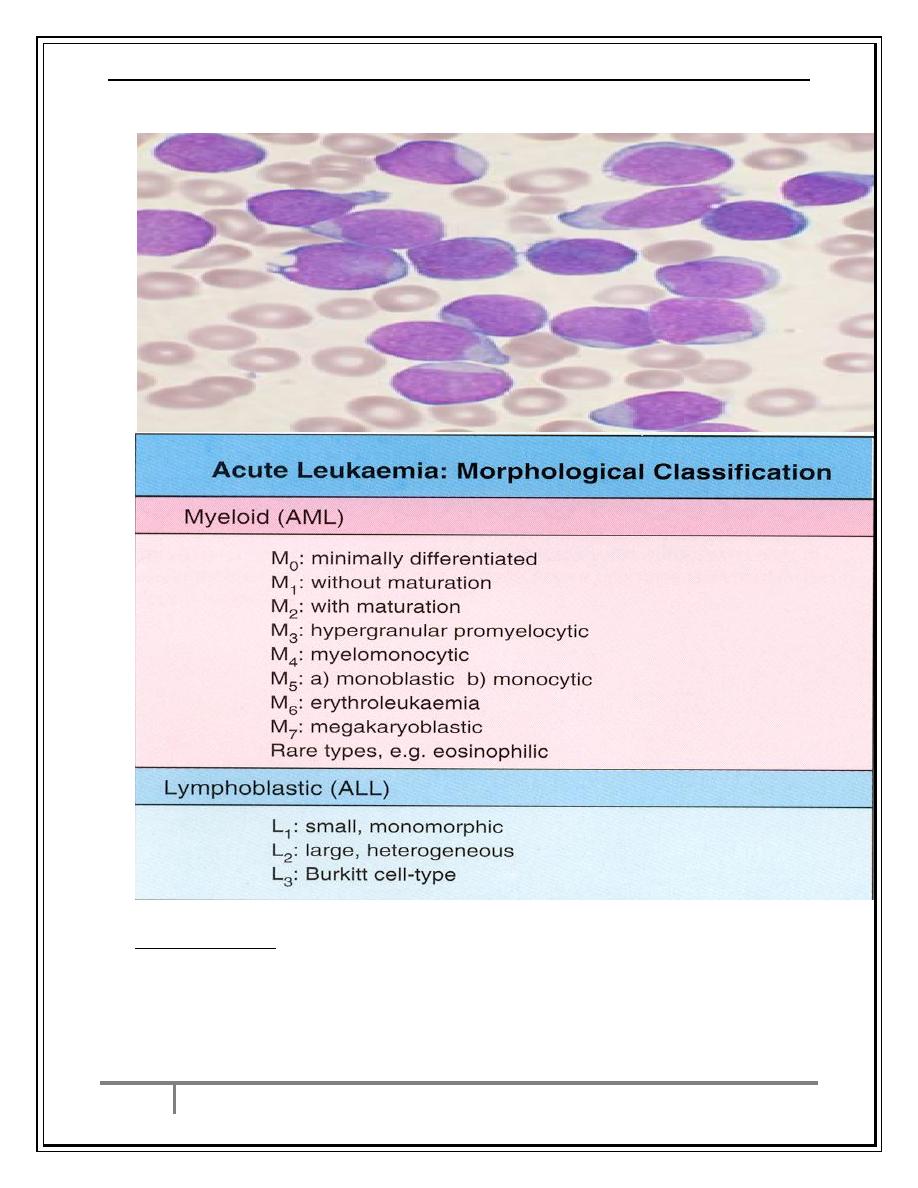
1-Acute Leukemia:
A-Acute myelocytic leukemia – AML- (includes myeloblastic, promyelocytic,
monocytic, myelomonocytic, erythrocytic, and megakaryocytic)
B-Acute lymphocytic leukemia – ALL- (includes T cell, B cell, and Null cell)
2-Chronic Leukemia:
A-Chronic myelocytic leukemia – CML - (includes myelocytic and
myelomonocytic)
B-Chronic lymphocytic leukemia – CLL - (includes classical CLL, Hairy cell
leukemia, prolymphocytic leukemia)
Acute vs. chronic leukemia
:
Acute leukemias:
I.
Young, immature ( blast ) cells in the bone marrow (and often blood)
II.
More fulminant presentation
III.
More aggressive course
Chronic leukemias:
I.
Accumulation of mature, differentiated cells
II.
Often subclinical or incidental presentation
III.
In general, more indolent (slow) course
IV.
Mature appearing cells in the B. marrow and blood
Etiology of Leukemias
Incidence: 100/ 100 000 /y .
Acute Leukemia: Affect all ages , ALL > in children, AML > in old.
Risk Factors:
1. Ionizing radiation
2. Cytotoxic drugs
3.Retroviruses.
4.Genetics
5.Immunological.
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
3
By : taher ali taher
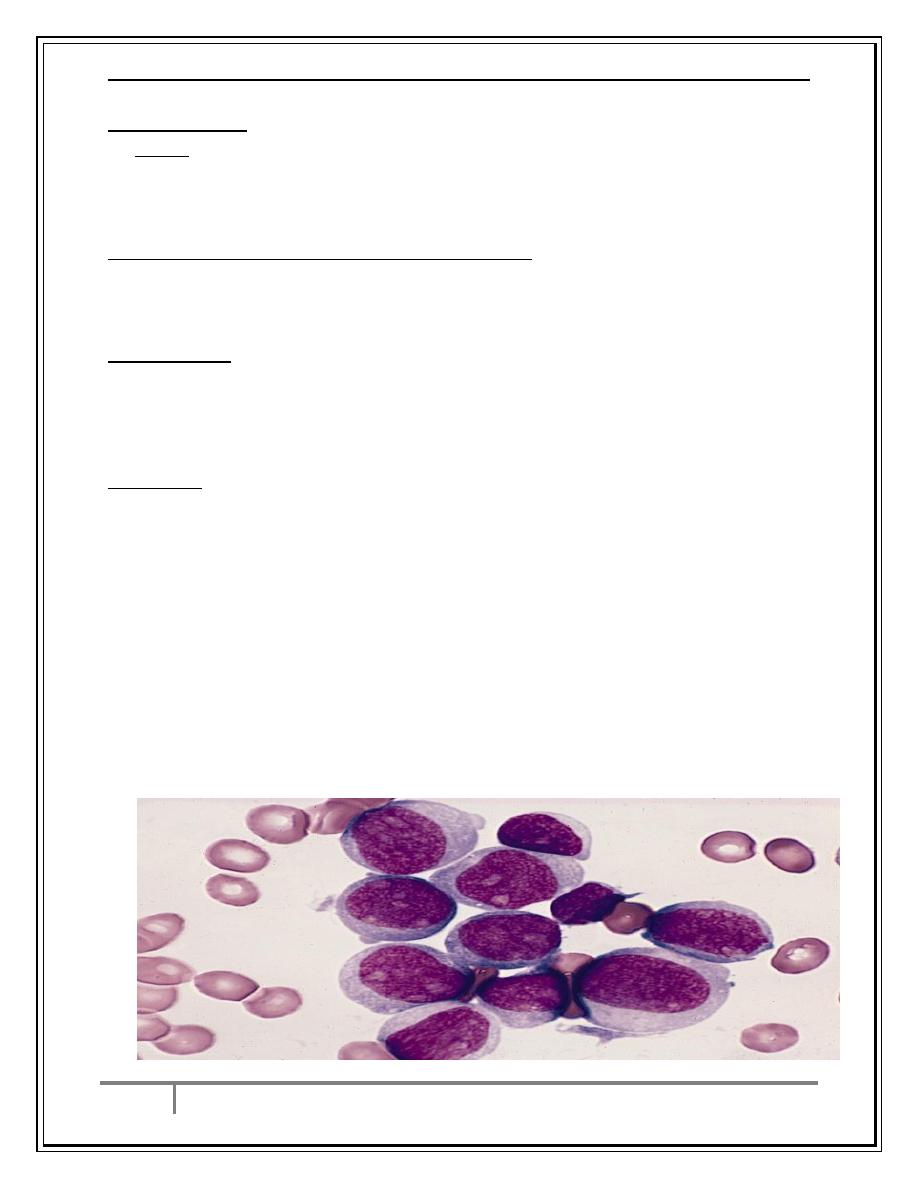
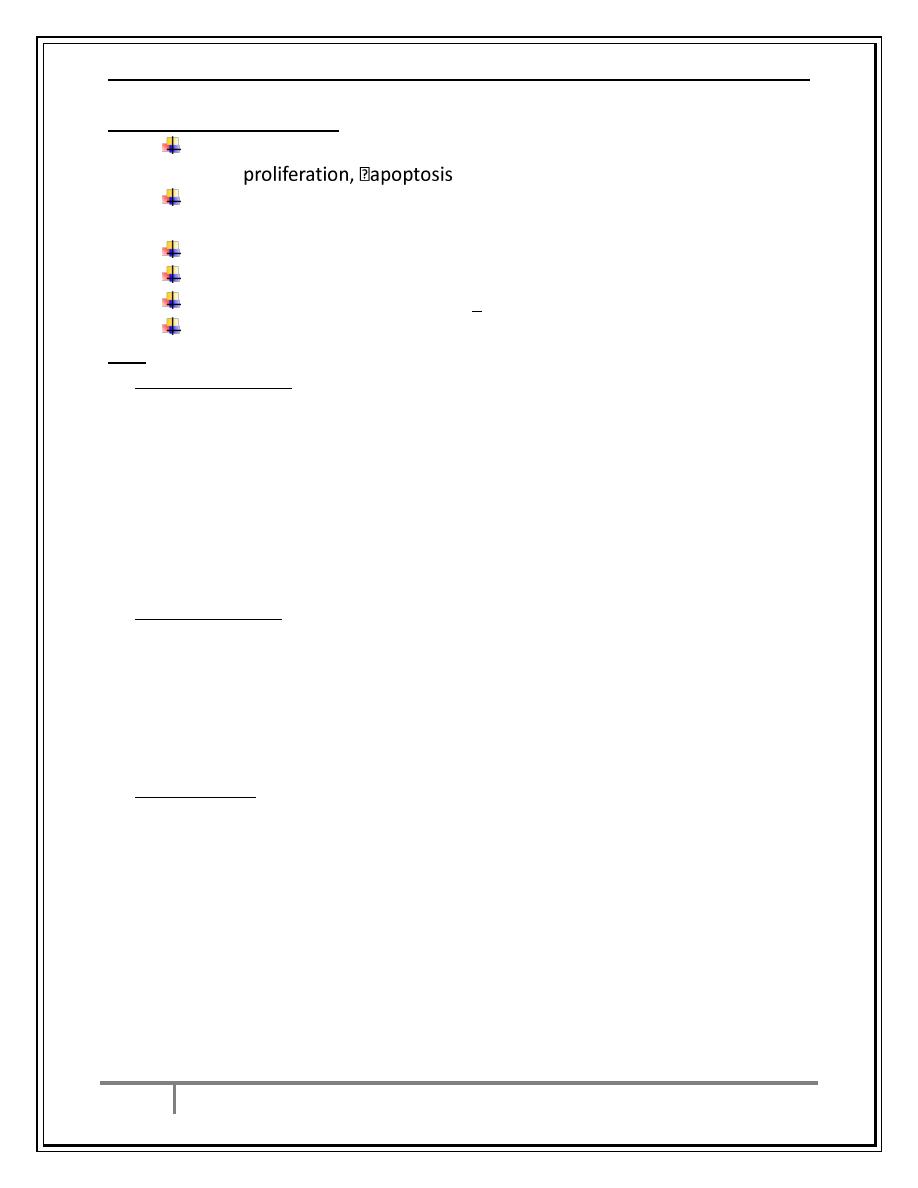
Acute Leukemia
Acute Leukemia : ALL & AML
*Failure of cell maturation, accumulation of useless immature cells in bone
marrow on the expense of normal haemopoeitic elements, with spilling of
immature cells into Blood.
Clinical Features are due to bone marrow failure
Anemia due to decreased RBC production.
Bleeding due to thrombocytopenia.
Infection due to leukopenia.
Physical signs:
1-Pallor
2-Bleeding spots on skin and mucus membranes.
3-sometimes lymphadenopathy and or splenomegaly.
Diagnosis :
Investigations:
1-CBP : Anaemia ,WBC count could be decreased, normal or increased. Usually
we find blast cells in peripheral blood.WBC may reach 100x109/l.Platelets :
usually very low.
2- Bone Marrow study : Confirm the diagnosis, we find replacement of normal
elements by leukaemic blast cells ˃ 20 % of the cells (normal < 5%)
*presence of Auer rodes in the cytoplasm of the blast cells = AML.Special
stains help to differentiate AML (sudan black +ve) from ALL (PAS+ve).
3-Immunophenotyping for CD markers.
4-Cytogenetics for specific chromosomal abnormalities.
5-Molecular studies by PCR for fusion genes and oncogens.
AML
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
4
By : taher ali taher
ALL
Special Features
1-Meningeal involvement more in ALL.
2-Mediastinal mass in ALL.
3-DIC and severe bleeding in AML-M3.
4-Gum hypertrophy: AML-M4 and AML-M5
5-Children ALL> AML , Adults AML> ALL.
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
5
By : taher ali taher
6-Auer rods in cytoplasm of blasts in AML.
7-Cure with Chemotherapy ALL> AML.
8-Prognosis better with ALL.
Principles of Treatment
1-Supportive Treatment:
A-Correction of anemia, platelet units if platelet count < 20 x109/l and there is
bleeding , prevention of infection by high standard sanitation. Allopurinol and
good hydration and adequate nutrition.
B-Treatment of febrile episodes ( mostly due to infections) by broad spectrum
antibiotics and antifungals when needed.
2-Chemotherapy protocols.
3-Allogeneic Bone Marrow transplantation for AML and relapsed ALL.
4-Targeted or biological Therapy :
ATRA and ATO for AML-M3 , Rituximab for ALL-L3, Imatinib for Philadelphia +ve
ALL, anti-CD33 monoclonal Ab in AML.
Chemotherapy
ALL Therapy :Explain Therapeutic regimen to patients & obtain consent.
-Aim of Treatment = destroy leukaemic cells without destroying the normal
stem cells. Protocol UKALL XII (contains multiple drugs )
1-Remission induction :Bulk of tumour is destroyed by combination
chemotherapy leading to severe bone marrow hypoplasia (require intensive
support .Aim is blast count in BM < 5%.
2-Remission consolidation :If Remission is achieved .Residual disease is
attacked by additional courses of chemotherapy to prevent relapse.
CNS prophylaxis = Intathecal (IT) Methotrexate ±cranial radiation to prevent
meningeal relapse.
Remission maintenance :If still in Remission: weekly methotrexate + daily
mercaptopurine for 2-3 years to prevent relapse.
*Failure of Remission induction. →Alternative combination of drugs.(poor
prpgnosis) then allogeniec BMT.
*Relapse during or after treatment → poor prognosis.
AML Therapy: Induction and Consolidation and may be offered allogeneic
BMT. High relapse rate and mortality in old patients.
Protocol 3&7 is the standard protocol (daunorubicine +cytosine arabinocide)
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
6
By : taher ali taher
Student activity
Mention 4 causes of death in acute leukemia. Take 3 minutes to discuss and
then answer.
Poor Prognostic Factors
1-Old age and comorbidities.
2-High WBC count.
3-Certain cytogenetic and molecular abnormalities.
4-AML following chemotherapy.
5-Failure of induction.
6-Relapse after treatment.
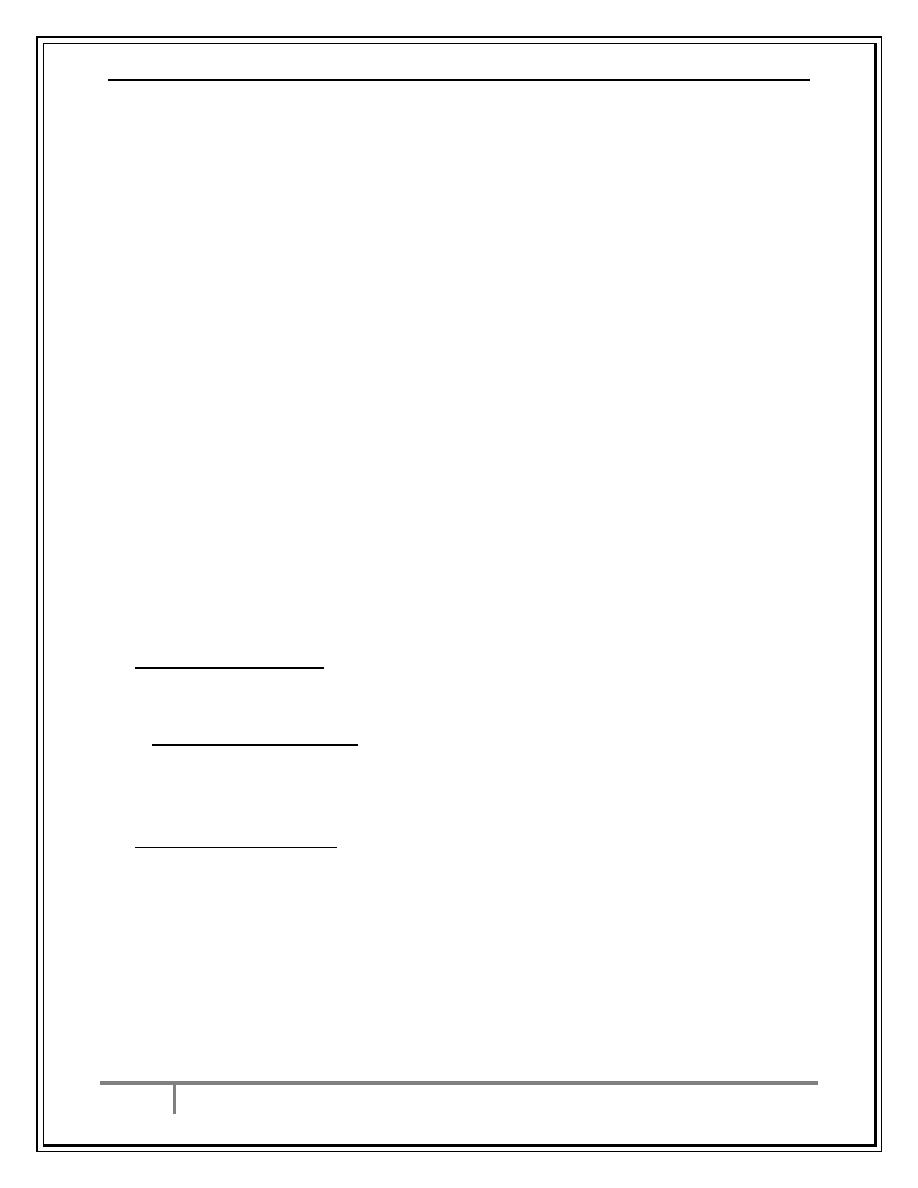
Survival Curve of AML According to Age
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
7
By : taher ali taher
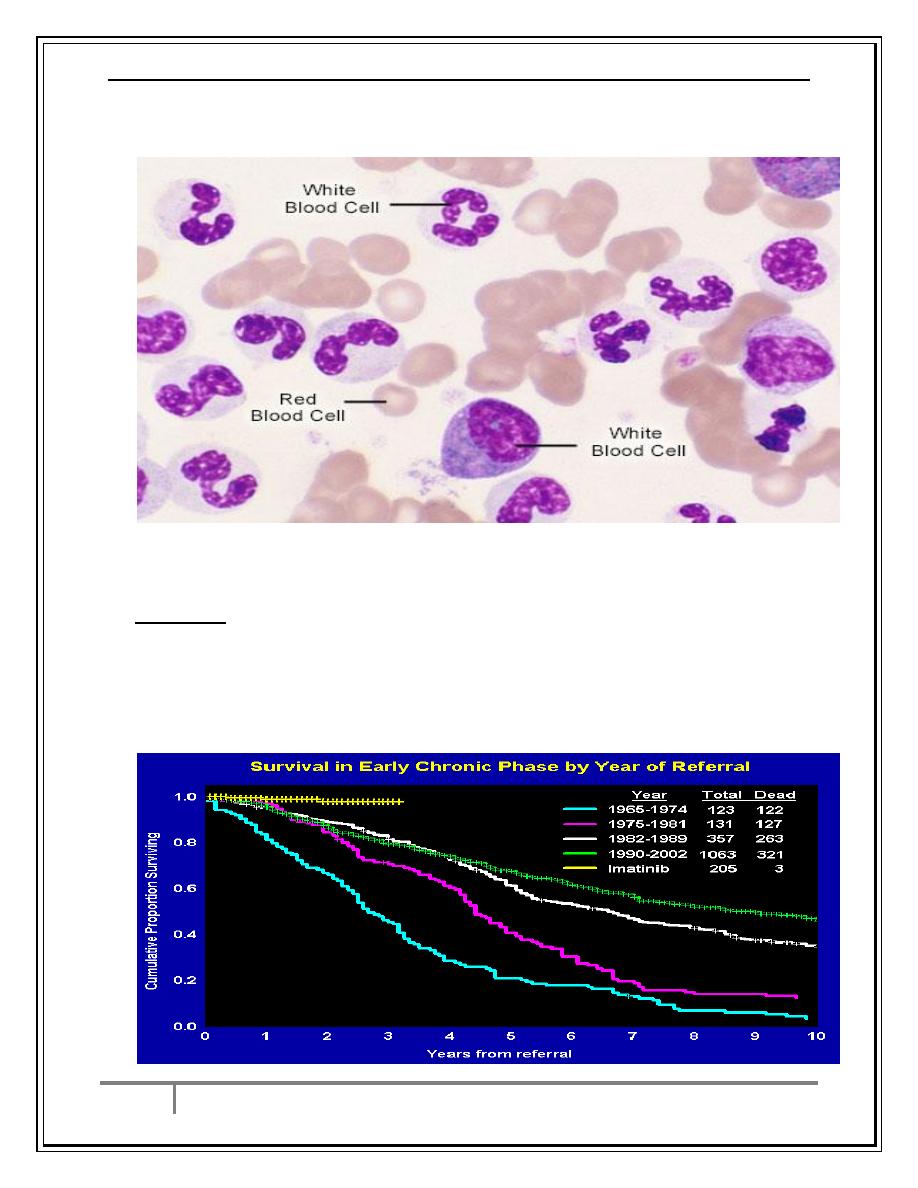
Chronic Myeloid Leukemia
Clonal myeloproliferative disorder of pluripotent stem cells
Cytogenetic hallmark: Philadelphia Chromosome=t 9;22
Molecular hallmark: BCR/ABL fusion oncogene
BCR/ABL initiation-causative event in CML
7% to 15% of adult leukemias
Median age 45-55 years; 20-30% >60 yrs
Younger in Iraq with annual incidence in Iraq 80-120/year.
CML
CML has 3 phases:
1.Chronic phase:. The disease is stable and responsive to treatment, lasting 3-5
y.
2.Accelerated phase :(not always seen), disease progression, control more
difficult.
3.Blast crisis: disease transforms into acute leukemia (AML%70 , ALL30%)
,Refractory to treatment, It is the major cause of death. Prior to imatinib
therapy, 10% CML patients transform to AML/y, now only 0.4-2.5% after up to
5y of treatment.
Clinical Features:
1-Chronic: abdominal heaviness, splenomegaly, sweating, bleeding tendency
after procedures.
2-Accelerated: anemia, huge splenomegaly, weight loss, bleeding tendency,
fever,bone pain.
3-Blastic : acute leukemia like picture due to bone marrow failure
Investigations
1.FBC:
Chronic Phase: Anemia (normochromic normocytic).WBC 15-600X10
9
/L , full
range of granulocytes precursors from myeloblast to mature neutrophils,
myeloblast ˂ 10%, Eosinophilia &Basophilia.
Platelets: ↑ in ⅓ (up to 2000x109/L) .Nucleated RBC are common.
Accelerated phase: ↑ % of blast cells.
*Blast transformation: Dramatic ↑ in Blast cells in peripheral blood and bone
marrow > 20%, ↓platelets. Basophils ↑
2. Bone marrow study: to confirm diagnosis & phase of disease.
3- increased serum LDH & Uric acid.
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
8
By : taher ali taher
CML
4-Conventional Cytogenetics: Ph. Chromosome.
5-FISH study: Fusion gene BCR/ABL.
6-PCR study: P210 protein detection.
Treatment:
1-Chronic Phase: *Tyrosine kinase inhibitors (TKI):
Imatinib, Nilotinib, Dasatinib. Improved survival.
*Others: hydroxyurea, alfa interferone.
2-Accelerated: new generation TKI, allogeneic BMT.
3-Blastic crises: Acute Leukemia treatment then allogeneic BMT.
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
9
By : taher ali taher
Chronic Lymphatic Leukemia
Most common Type of leukemia(30%).
M:F is 2:1, median age at presentation 65-70y.
B lymphocytes fail to transform to plasma cells leading to accumulation of
immortal immuno-incompetent lymphocytes → impaired immune function
BM dysfunction.
Clinical Features:
*insidious onset. Some cases discovered incidentally on routine FBC.
1-Painless Lymphadenopathy may be present for a long time.
2-systemic symptoms e.g. fever ,night sweats and weight loss in advanced
cases.
3-Hepato-splenomegaly.
4-Repeated infections, pallor and bleeding tendency in advanced cases.
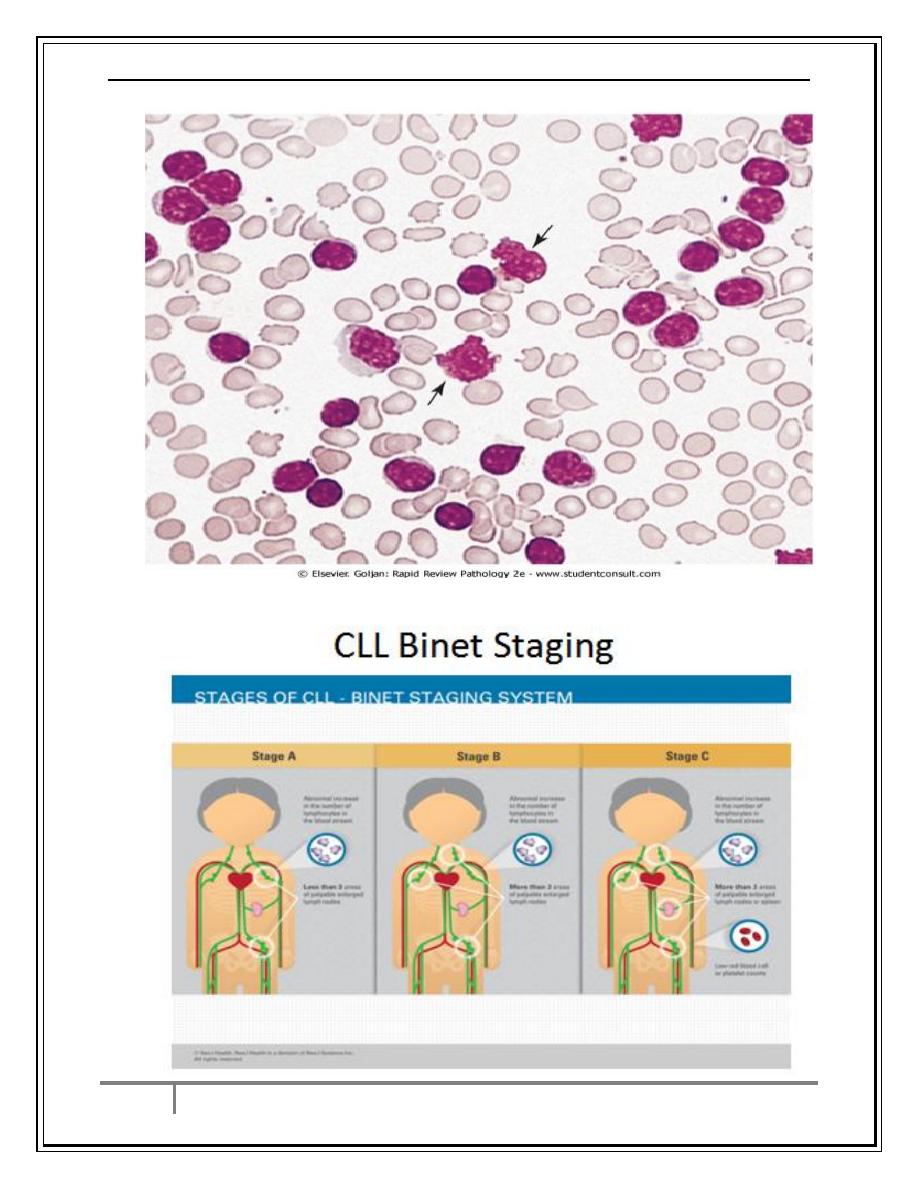
CLL investigations
Investigations:
1.FBC: Mature looking lymphocytes ˃ 5x 10
9
/L. characteristic morphology &
markers, CD19 & CD23. +ve .WBC count between 15-200x10
9
/l.We can find
low hemoglobin and platelet count.
2.↑ Reticulocyte count & +ve coombs test.= immune haemolytic Anemia
(may occur).
3.Serum Immunoglobulins : decreased in some cases.
4.B.Marrow exam is not essential for diagnosis, but helpful for prognosis(
diffuse involvement = poor prognosis),& to monitor response to therapy.
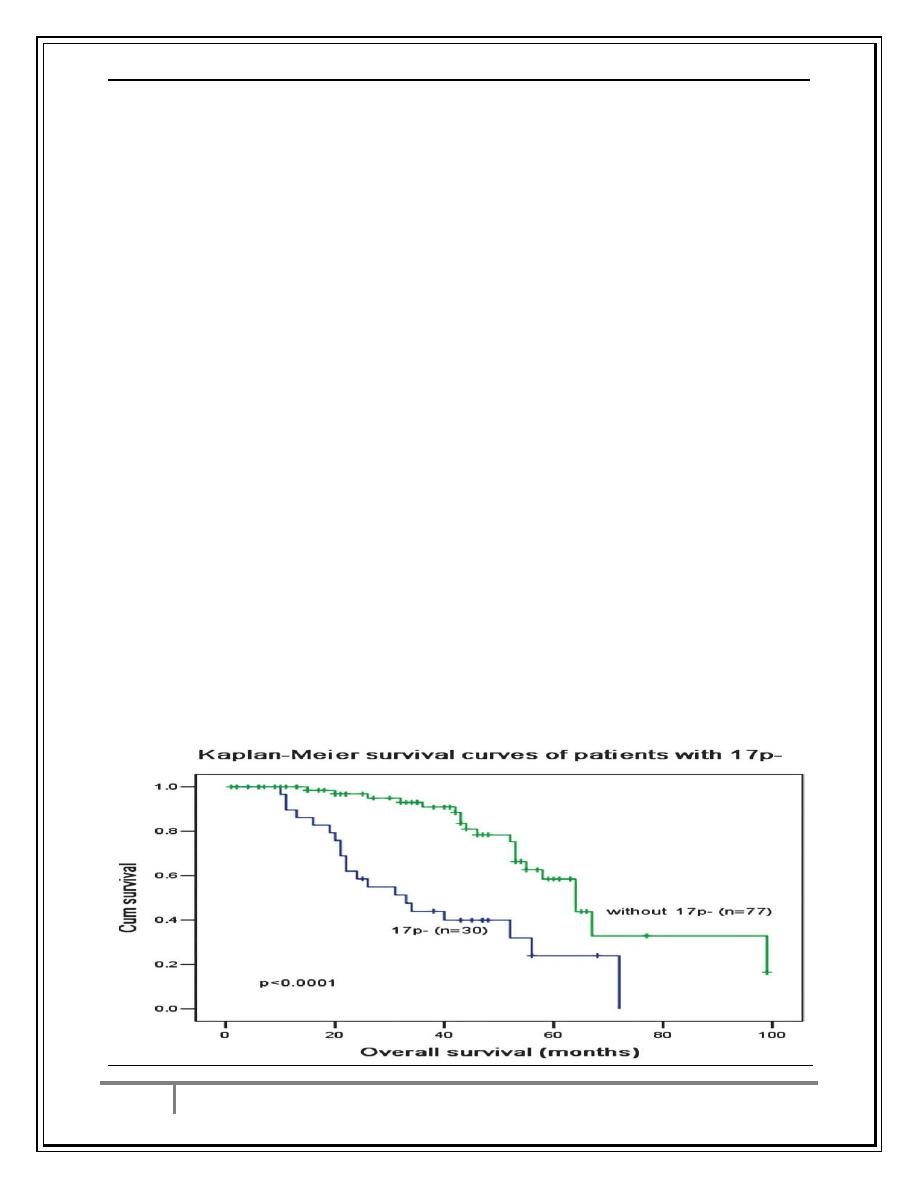
Main prognostic factor are :advanced stage of the disease ,CD38 +ve,
Mutation of IgVH Genes, 17 p deletion: suggest poor prognosis.
5-Chest x-ray, US of abdomen.
6-Lymph node biopsy: indicated only if we suspect NHL.
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
10
By : taher ali taher
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
11
By : taher ali taher
Treatment
*Stage A :no treatment for most patients.
*Stage B and C:
Indications for Treatment:
1. BM failure.
2. Massive or progressive lymphadenopathy or Splenomegaly.
3. Systemic symptoms e.g. wt. loss or night sweat.
4. Rapidly ↑ lymphocyte count.
5. Autoimmune haemolytic An., or ↓ Platelets
CLL Treatment
*For fit patients < 65 y of age: Rituximab +Fludarabine + Cyclophosphamide
→ good remission rate & disease free survival .
For older patients or frail patients: Chlorambucil + Prednisolone.
*For B.M. Failure or autoimmune cytopenias → corticosteroid.
*Supportive care: Symptomatic, Anemia or thrombocytopenia →
Transfusion.
Treatment of infections , IV immunoglobulins for hypogammaglobulinaemia.
Radiotherapy: LN causing discomfort or obstruction.& for symptomatic
splenomegaly.
Prognosis: Overall survival is 6y, stage C 2-3y, ,50% die from infection.
Rarely it may transform into aggressive high grade Lymphoma(Richters
syndrome).
Survival of CLL Patients
Ali M. Jawad Acute Leukemia, Chronic Leukemia
9/3/2017
12
By : taher ali taher
Prolymphocytic Leukemia
Variant of CLL, mainly in Male ˃ 60y. 25% T cell variety
Massive splenomegaly, + Little Lymphadenopathy.
* WBC often ˃ 400 x 10
9
/ L (Characteristic cell is large lymphocyte with
prominent nucleolus).
Treatment: Is generally unsuccessful & prognosis very poor.
Leukapharesis, Splenectomy, & chemotherapy may be tried.
Hairy cell Leukemia
Rare,chronic lymphoproliferative B cell disorder, > in males, median age 50y.
General ill health, & recurrent infection.
Splenomegaly 90%, LN unusual.
Lab.: Severe Neutropenia, Monocytopenia,& characteristic HAIRY CELL in
Blood & B.M.
Treatment: Cladribine & Deoxycoformycin.
Prognosis is good.
Conclusion
1-Acute Leukemias are due to accumulation of blast cells and are rapidly fatal if
not treated but some patients can be cured with chemotherapy ± BM
transplantation ( ALL better than AML).
2-Chronic myeloid leukemia is due to t 9;22 and is of chronic course. It can be
controlled with tyrosine kinase inhibitors.Acute transformation needs BMT.
3-Chronic lymphatic leukemia is a disease of old age and has an indolent
course. It can not be cured by current chemotherapy or immunotherapy.
…the end…
