
MEDICINE
haematology
oj
Lec.55
Dr.Ali M. Jawad
Myeloproliferative Disorders
Lec . 7
23/3/2017
Done by : Taher Ali Taher
2016-2017
مكتب اشور لالستنساخ
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
1
By : taher ali taher
Objectives
By the end of this lecture, the student should be able to:
1-classify myeloproliferative disorders.
2-list the clinical features of myeloproliferative disorders.
3-discuss briefly the diagnosis and treatment of polycythemia rubra vera,
myelofibrosis and essential thrombocythemia.
Case Scenario
A 60 year old male presented with 4 months history of progressive
pallor , weight loss and heaviness in the abdomen. He bled after tooth
extraction.
An US of abdomen revealed a hugely enlarged spleen.
His Hemoglobin was 9 gm/dl.
What is your differential diagnosis?
Myeloproliferative Disorders
o Neoplastic (clonal) disorders of hemopoietic stem cells
o Over-production of all cell lines, with usually one line in particular
o Fibrosis is a secondary event
o Transformation to Acute Myeloid Leukemia may occur
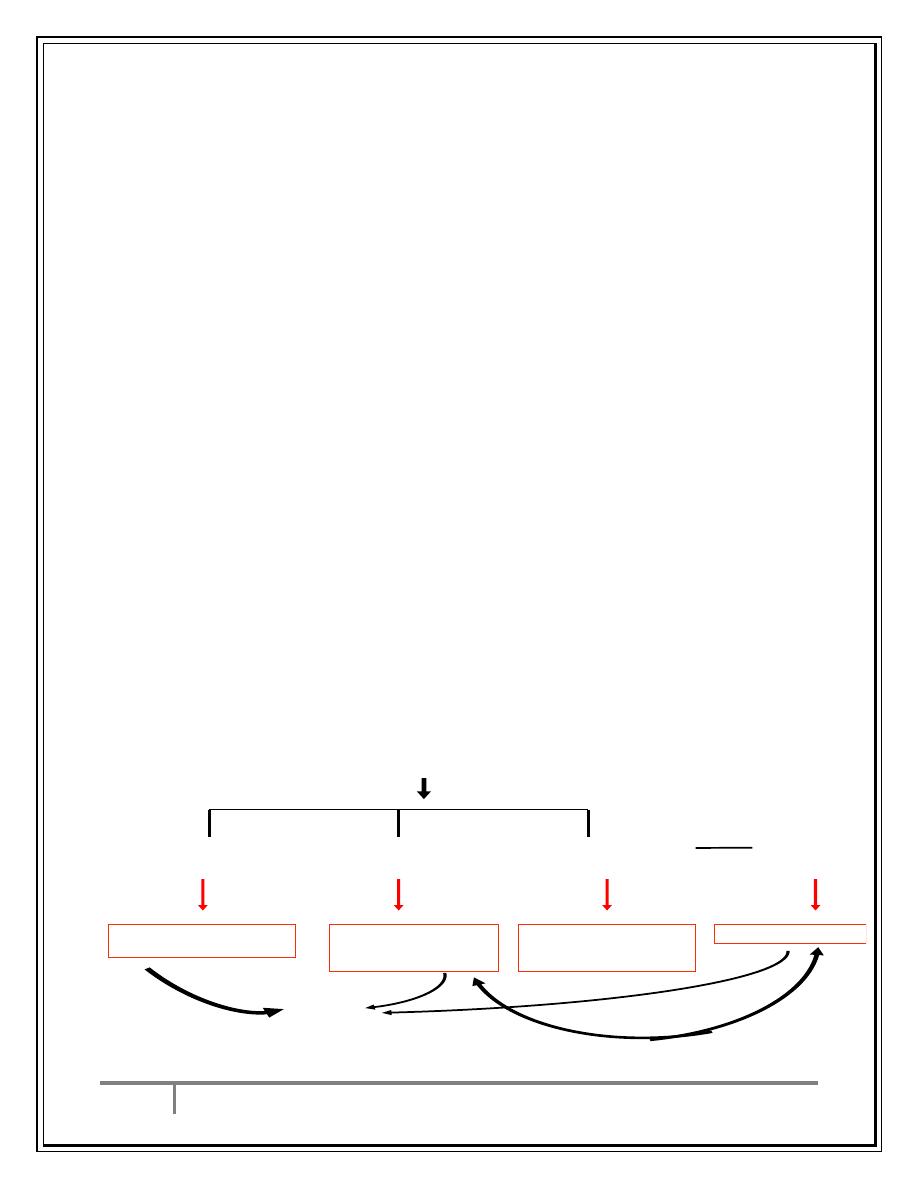
MPD
–Classification
1. Polycythemia (Rubra) Vera (PRV, PV)
2. Myelofibrosis (with Myeloid Metaplasia)
3. Essential (Primary) Thrombocythemia
Bone marrow stem cell
Clonal abnormality
Granulocyte
precursors
Red cell
precursors
Megakaryocytes
Reactive
fibrosis
Essential
thrombocytosis
(ET)
Polycythaemia
rubra vera
(PRV)
Myelofibrosis
AML
Chronic myeloid
leukemia
70%
10%
10%
30%
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
2
By : taher ali taher
Polycythemia
True / Absolute
Primary Polycythemia
Secondary Polycythemia
1- Epo dependent
- Hypoxia dependent
- Hypoxia independent
2- Epo independent
Apparent / Relative
- Reduction in plasma volume
Causes of secondary polycythemia :-
ERYTHROPOIETIN (EPO)-MEDIATED
- Hypoxia-Driven
Chronic lung disease
Right-to-left cardiopulmonary vascular shunts
High-altitude habitat
Chronic carbon monoxide exposure (e.g., smoking)
Hypoventilation syndromes including sleep apnea
Renal artery stenosis or an equivalent renal pathology
- Hypoxia-Independent (Pathologic EPO Production)
Malignant tumors
Hepatocellular carcinoma
Renal cell cancer
Cerebellar hemangioblastoma
Nonmalignant conditions
Uterine leiomyomas
Renal cysts
Postrenal transplantation
Adrenal tumors
POLYCYTHEMIA VERA
o Chronic, clonal myeloproliferative disorder characterized by an
absolute increase in number of RBCs.
o Incidence:2-3 / 100000.
o Median age at presentation: 55-60 y.
o M/F: 0.8:1.2 .
o The hallmark is JAK2 mutation.
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
3
By : taher ali taher
Clinical features
Plethora and Headaches
Splenomegaly
Generalized pruritus (after bathing)
Vascular occlusion
- Venous thrombosis
- TIA, stroke, MI
Erythromelalgia (acral dysesthesia and erythema)
Gouty attacks due to hyperuricemia
Lab Investigations
1-CBP: erythrocytosis, increased Hb> 17gm/dl, may find basophilia and
eosinophilia and thrombocytosis.
2-BM study: hypercellular marrow with increased fibrous tissue and
megakaryocytes.
3-Hyperuricemia, increased serum vit B12.
4-US of abdomen usually reveals Splenomegaly.
5-Decreased serum erythropoietin.
6-+ve JAK2 mutation by PCR study.
Diagnostic Criteria
Major Criteria
1- Hemoglobin >18.5 g/dL in men, >16.5 g/dL in women, or other evidence of
increased red blood cell volume.
2- Presence of JAK2 V617F.
Minor Criteria
1- Bone marrow biopsy showing hypercellularity for age with trilineage
growth (panmyelosis) with prominent erythroid, granulocytic, and
megakaryocytic proliferation
2- Serum erythropoietin level below the reference range for normal
3- Endogenous erythroid colony formation in vitro
*Diagnosis Requires the presence of both major criteria and one minor criterion
or the presence of the first major criterion together with two minor criteria
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
4
By : taher ali taher
Treatment
The mainstay of therapy in PV remains phlebotomy to keep the PCV
below 45 percent in men and 42 percent in women
hydroxyurea in high-risk patients for thrombosis (age over 70, prior
thrombosis, platelet count >1,000,000/microL, presence of
cardiovascular risk factors)
Aspirin (75-100 mg/d) .
Interferon alfa in patients with refractory pruritus, and for pregnants.
Anagrelide is used mainly to manage thrombocytosis in patients
refractory to other treatments.
Allopurinol
JAK2 inhibitors like ruxolitinib for refractory cases.
Prognosis:
After many years progression to myelofibrosis and few will go to AML.
Causes of Death:
1-Thromotic episodes.
2-Bleeding.
3-Transformation into AML.
Student Activity
o Take 3 minutes to discuss why some cases of polycyhema vera develop
anemia after a time.
o Try to give 3 explanations for that.
Primary Myelofibrosis (MF)
Clonal hemopoietic stem cell disorder.
Ending in bone marrow failure.
There is myeloid metaplasia (extra-medullary hemopoiesis)
JAK 2 mutation in around 50% of cases.
Tendency to transformation to AML.
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
5
By : taher ali taher
Clinical Features
Fatigue, weight loss, nocturnal sweating, pruritus.
Splenomegaly .
Anemia .
Portal hypertension due to huge splenomegaly .
Splenic infarction and hypersplenism.
GI bleeding (melena or hematochezia).
Hypertrophic osteoarthropathy.
Bone and musculoskeletal pain.
Thrombotic and bleeding episodes.
Laboratory Investigations
1-CBP: anemia, WBC count increased or normal or decreased, Platelet
increased and later decreased.
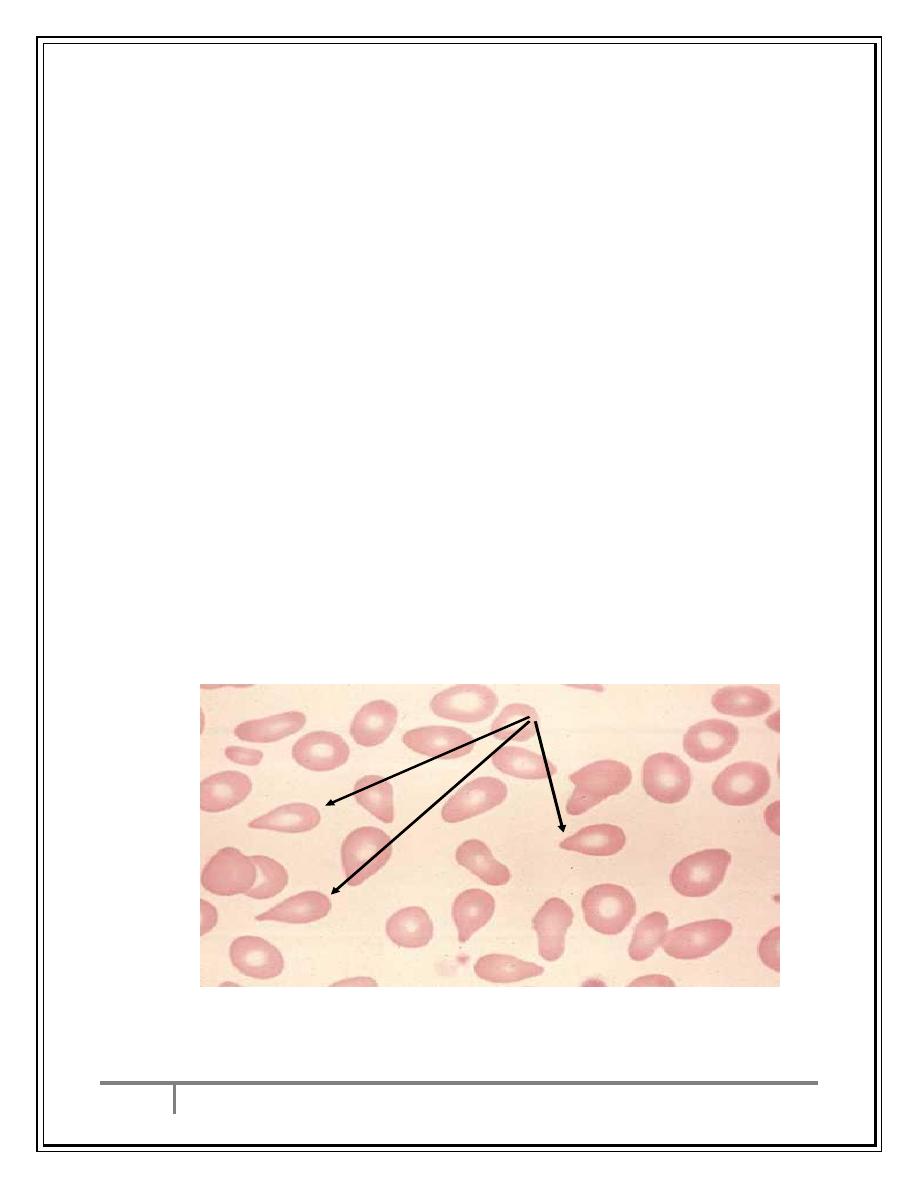
Blood film: tear drop cells with leuco-erythroblastic blood picture(immature
RBC+WBC).
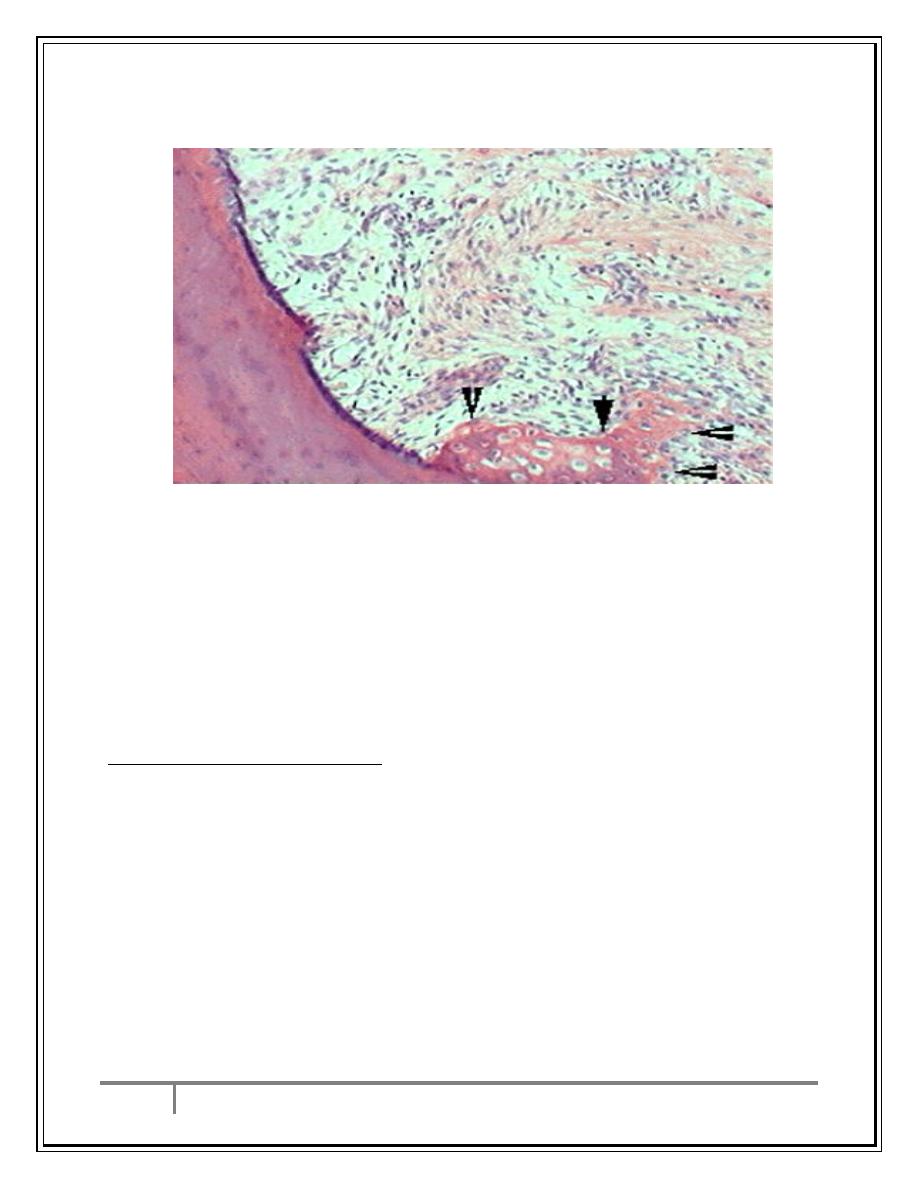
2-BM Biopsy: megakaryocyte proliferation +Fibrosis and later sclerosis.
3-Increased S.uric acid and LDH.
4-Splenomegaly by US of Abdmen.
5- 50% have JAK 2 mutation.
Tear Drop Cells (or Tear
Drop Poikilocytes)
Blood Film of MF
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
6
By : taher ali taher
Bone Marrow biopsy of MF
fibrosis
new bone (arrows)
Treatment
1-correction of anemia .
2-prevention of thrombotic events by aspirin.
3-allopurinol.
4-hydroxyurea or alfa interferone to control systemic symptoms ,
thrombocytosis and to decrease size of spleen.
5-JAK 2 inhibitors in resistant splenomegaly.
5-Allogeneic BMT for refractory cases and on AML transformation.
Essential Thrombocythemia (ET)
o ET is the second-most-common MPN .
o The median age at diagnosis is approximately 60 years, although the
diagnosis increasingly is made in younger adults.
o Women with ET outnumber men 1.5- to 2-fold, particularly among ETs
diagnosed in the third
o to fifth decade of life.
o Morbidity and mortality from ET predominantly
o related to thrombo-embolic and less commonly, hemorrhagic
complications.
o 40% have JAK2/MPL mutation
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
7
By : taher ali taher
Clinical Features
1- Vasomotor:
A. “Vascular” headaches, visual disturbances, dizziness, burning
B. dysesthesia of the palms and soles (erythromelalgia),
C. acrocyanosis, paresthesias, cutaneous ulcers.
D. cognitive or psychiatric deficits, seizures.
2- Thrombotic:
I.
Arterial: cerebral (TIA, CVA), coronary, ophthalmic, distal/
extremities
II.
Venous: deep extremities, pelvic, mesenteric, hepatic, portal.
3- Hemorrhagic:
- Gastrointestinal, mucosal, epistaxis, urogenital, deep hematoma.
4- Obstetric:
- First-trimester spontaneous abortion
5- Splenomegaly occur in some cases.
6- AML transformation is rare.
Laboratory Investigations
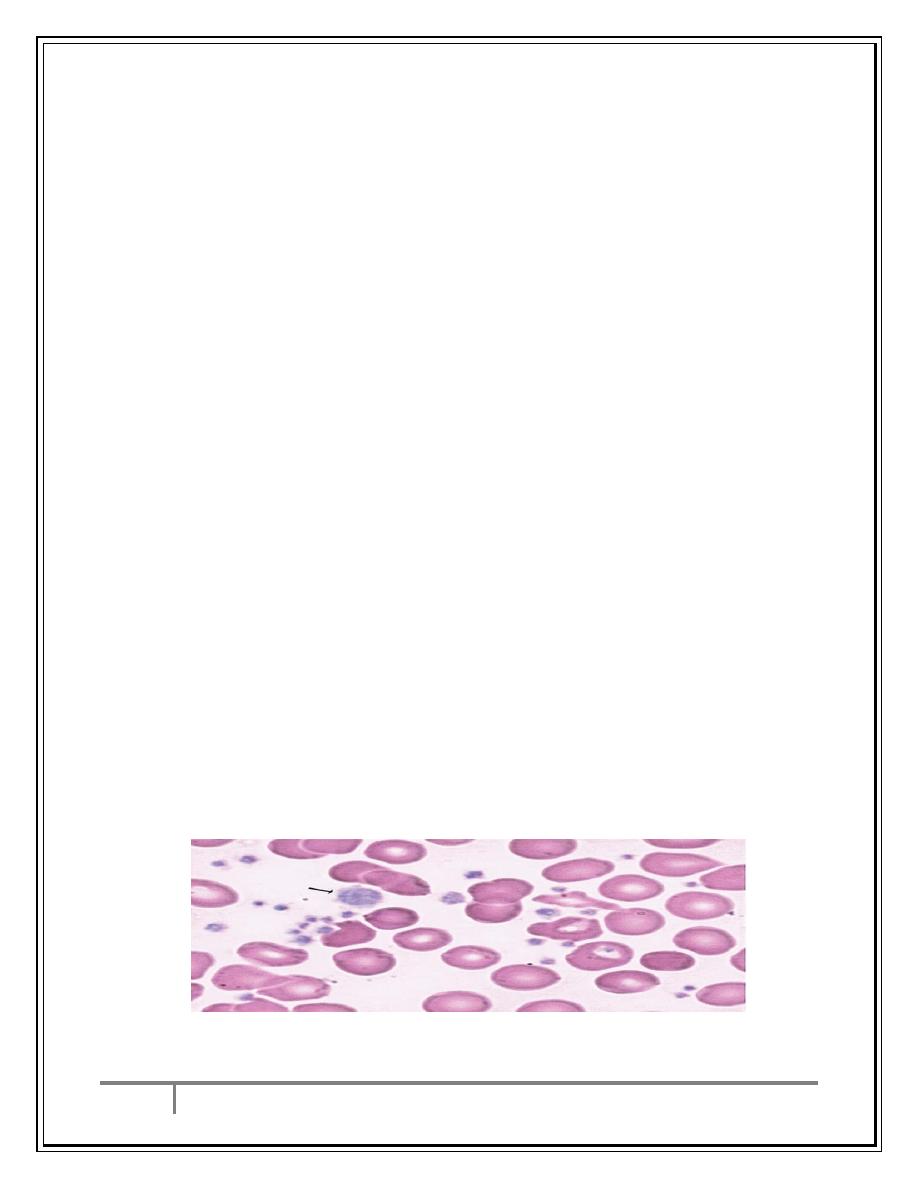
1-CBP: persistant thrombocytosis with large size platelets.WBC count may be
increased.
2-+ve JAK 2/MPL mutation.
3-BM study: clusters of large megakaryocytes.
4-Need to exclude:
Iron Deficiency
CML
Myelofibrosis
ET Blood Film
Dr.
Ali M. Jawad
Myeloproliferative Disorders
23/3/2017
8
By : taher ali taher
Risk stratification for ET
Low risk (all of the following)
1- Age <60 years old
2- No history of thromboembolism
3- No cardiovascular risk factors (smoking,hypercholesterolemia)
Indeterminate risk
- Neither low nor high-risk disease
High risk (one or both)
A. Age ≥60 years old
B. History of thromboembolism
Treatment
According to Risk categories:
Low Risk: Low-dose aspirin
Intermediate Risk: Low-dose aspirin
High Risk : Low-dose aspirin + hydroxyurea
Conclusion
1-Myeloproliferative neoplasms are chronic disorders arising from BM stem
cells .The hallmark is JAK 2 mutation and variable tendency for AML
transformation.
2-Polcythemia vera present with erythrocytosis, splenomegaly and thrombotic
tendency, control is by phlebotomy ,aspirin and hydroxyurea.
3-Primary myelofibrosis presents with anemia and huge splenomegaly. It is
treated with blood transfusion and hydroxyurea.
4-Essential thrombocythemia presents with thrombotic tendency and in high
risk patients it is treated with aspirin and hydroxyurea.
…the end…
