
MEDICINE
haematology
oj
Lec.53
Dr.Ali M.
Hodgkin's Disease, non-Hodgkin's
Lymphoma &Plasma Cell
Myeloma
Lec . 6
16/3/2017
Done by : Taher Ali Taher
2016-2017
مكتب اشور لالستنساخ
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
1
By : taher ali taher
Objectives
By the end of this lecture, the student should be able to:
1-recall a broad classification of Hodgkin's disease and non-Hodgkin's
Lymphoma.
2-describe the clinical presentation and diagnosis of Hodgkin's disease and
non-Hodgkin's Lymphoma and principles of treatment.
3-Desribe briefly the clinical features, diagnosis and treatment of plasma cell
myeloma.
Case Scenario
A 20 year old female presented with 8 weeks history of intermittent fever,
multiple cervical and axillary lymphadenopathy.
Her clinical examination revealed her to be febrile, pale, with multiple cervical
lymph nodes and slightly enlarged spleen.
What is your differential diagnosis?
Hodgkin's Disease
Definition:-
A lymphoproliferative disorder of B-lymphocytes.
The hallmark is the presence of Reed –Sternberg cells (RS Cells) in the
involved organs mostly lymph nodes.
Males are slightly more affected.
Etiology is not clear but EBV infection may have some role .
Pathological classification:
1.Nodular lymphocyte predominant,(5%),slow growing, localised , rarely
fatal.
2.Classical HL:
a. Nodular sclerosing (70%), >in young Females, mostly presents with SVC
obstruction.
b.Mixed Cellularity (20%), > in elderly.
c. Lymphocyte-rich: (5%) > in Males.
d.Lymphocyte –depleted:(rare) , widely spread at diagnosis and aggressive.
Clinical Features :-
1-Lymphadenopathy: localized or generalized, painless mobile and rubbery.
2-Less frequent: hepatomegaly, splenomegaly, mediastinal mass, SVC
obstuction, pleural effusion, spinal cord compression, bone marrow
involvement.
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
2
By : taher ali taher
3-Systemic B-symptoms: fever, weight loss ( > 10% over 6 months), sweating.
4- Others : PUO, Itching .
Diagnosis and Staging
*Pathological Diagnosis: Tissue biopsy like LN, BM, Pleural biopsy….
The LN sections will show: loss of normal nodal architecture + inflammatory
cells+ RS cells.
Immunophenotyping(CD markers): +ve for CD15+CD30 in classical HD.
*Staging Procedures:
1-History+Physical Examination
2-CBP: shows lymphopenia+ high ESR, sometimes anemia.
3-Renal + Liver Function tests.
4-Serum Albumin and serum LDH
5-CXR and US of Abdomen.
6-Spiral CT scan of neck+ chest + abdomen or PET-CT scan
7-Bone marrow study in cases of anemia and pancytopenia.
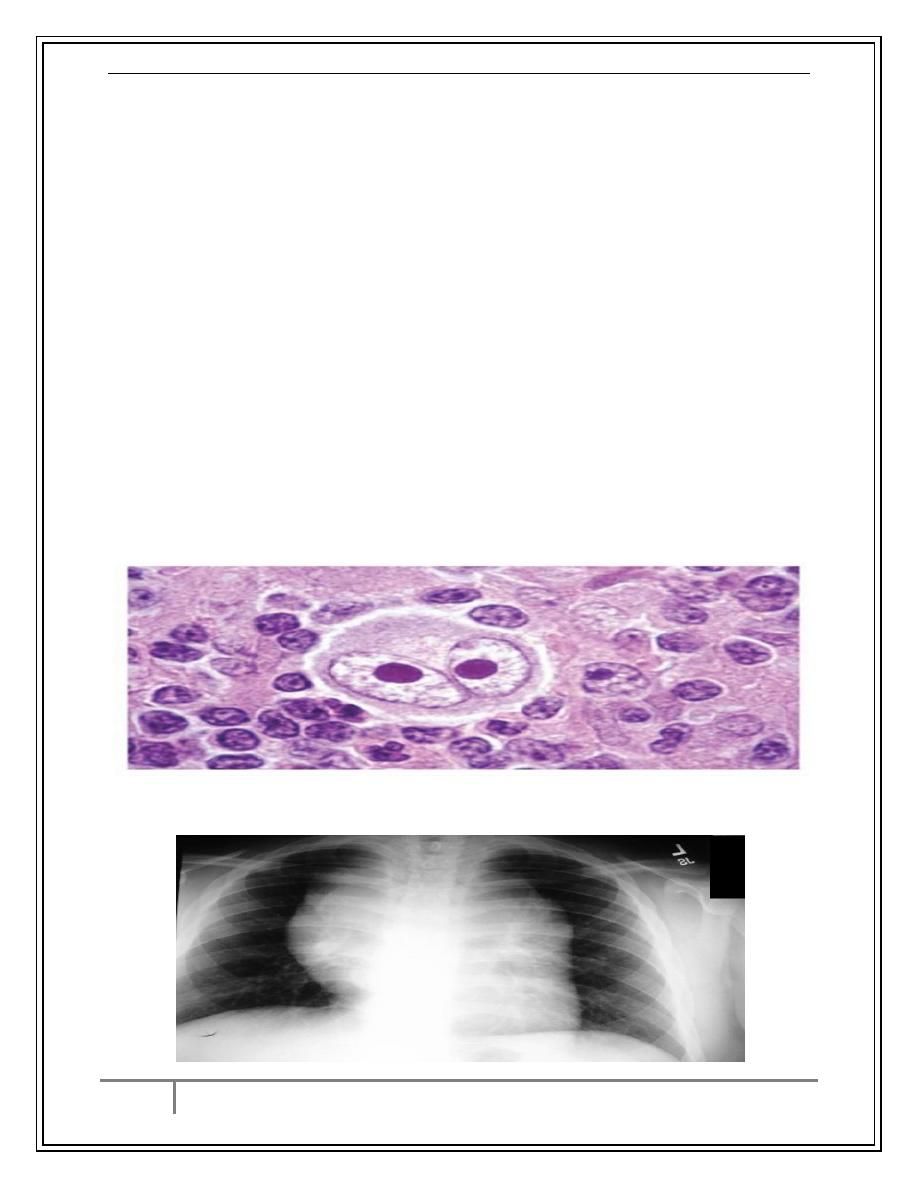
RS Cells
Mediastinal mass
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
3
By : taher ali taher
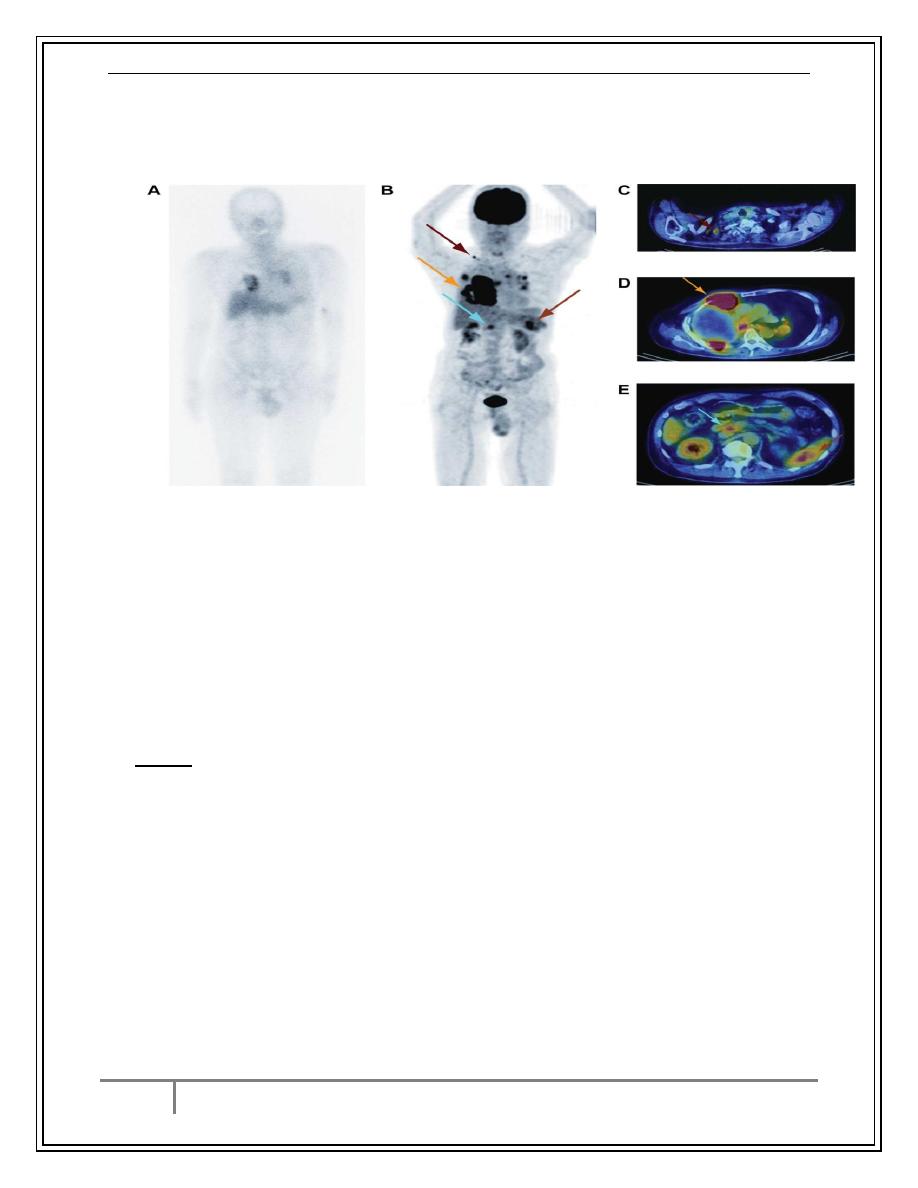
PET-CT scan
Ann-Arbor Staging
Clinical Stages:-
1.Stage I : Single LN region(I)or extra lymphatic site(IE).
2.Stage II: 2 or more LN regions(II),or an extralymph.site & LN regions on the
same side of (above or below) the diaphragm(IIE).
3. Stage III:LN regions on both sides of the diaphragm with (IIIE) or without
(III) localized extra lymphatic or spleen (IIIS) or both (IIISE).
4. Stage IV: Diffuse involvement of one or more extra-lymphatic tissue e.g.
liver or BM.
Notes: 1. Each stage is sub-classified into :
No B-systemic symptoms.
B-Systemic symptoms ( Weight loss, drenching sweat)
2. Lymphatic structure = LN, Spleen, Thymus, Waldeyers ring, Appendix.
Treatment
*Treatment Modalities:
1-Chemotherapy: ABVD or BEACOPP, ICE (2
nd
line)
2-Radiotherapy (RT).
3-Monoclonal Ab: anti-CD30.
4-Autologous BMT , allogeniec BMT.
*Plan: according to stage:
1-I & II: ABVD (x3-4) + involved field RT ,> 90% go into Complete Remission (CR)
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
4
By : taher ali taher
2-III & IV: ABVD (x 6-8) , 80% go into CR.
*The patient will have follow up every 3- months.
3-Relapsed: Second line Chemo followed by auto-BMT.
4-Resistant cases: antiCD30 followed by allo-BMT.
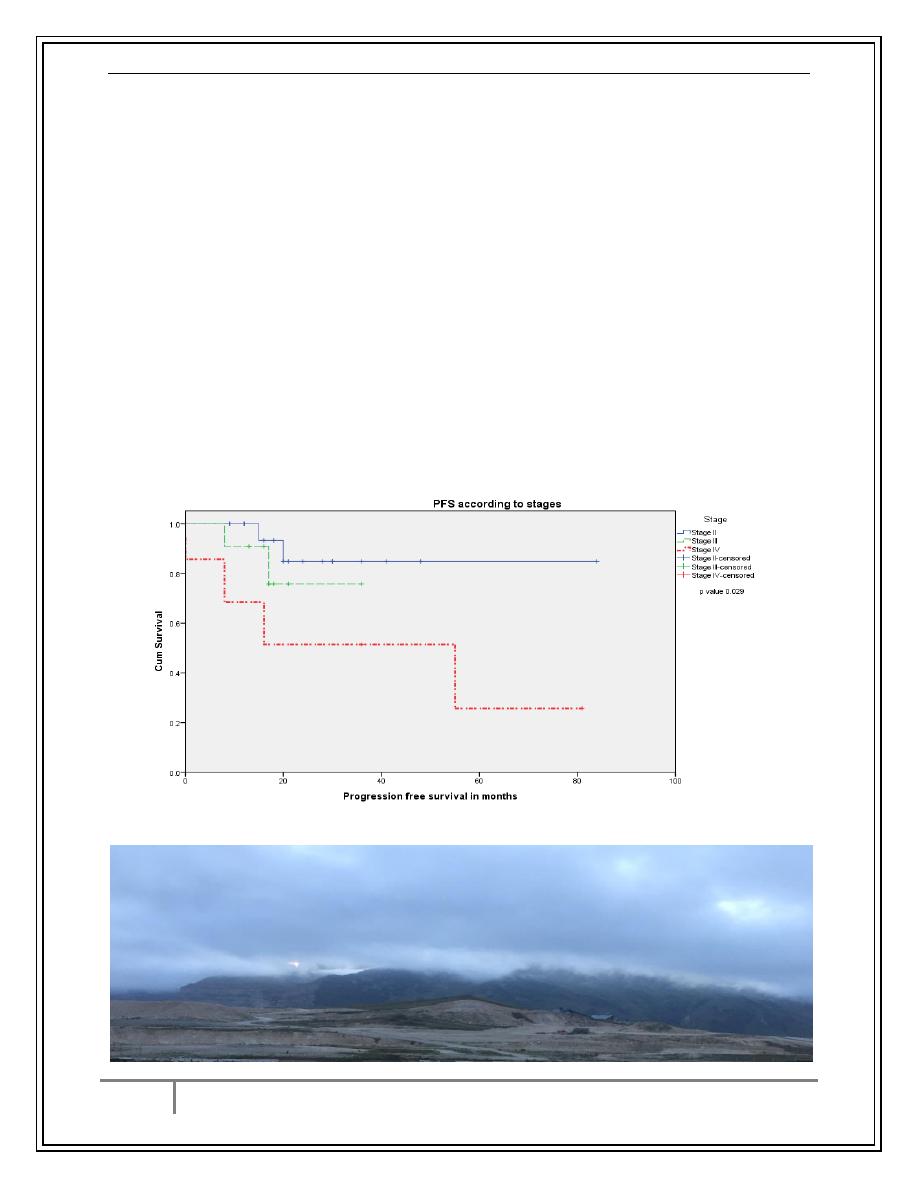
Prognosis
*Poor Prognosis:
1-Advanced stage.
2-Age > 45 y.
3-Male gender.
4-Lymphocyte depletion subtype.
5-high ESR, lymphopenia, anemia, low serum albumin , Bulky mediastinal
mass, high s.LDH
6-Resistance and early relapse.
PFS Survival of HD by stage/Iraqi Data
J Fac Med Baghdad 2015;Vol.57 , No.2
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
5
By : taher ali taher
Non-Hodgkin's Lymphoma
1. Updated REAL/WHO Classification
2. B-cell neoplasms
3. Precursor B-cell neoplasm: precursor B-acute lymphoblastic
leukemia/lymphoblastic lymphoma (LBL).
4. Peripheral B-cell neoplasms.
B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma.
B-cell prolymphocytic leukemia.
Lymphoplasmacytic lymphoma/immunocytoma.
Mantle cell lymphoma.
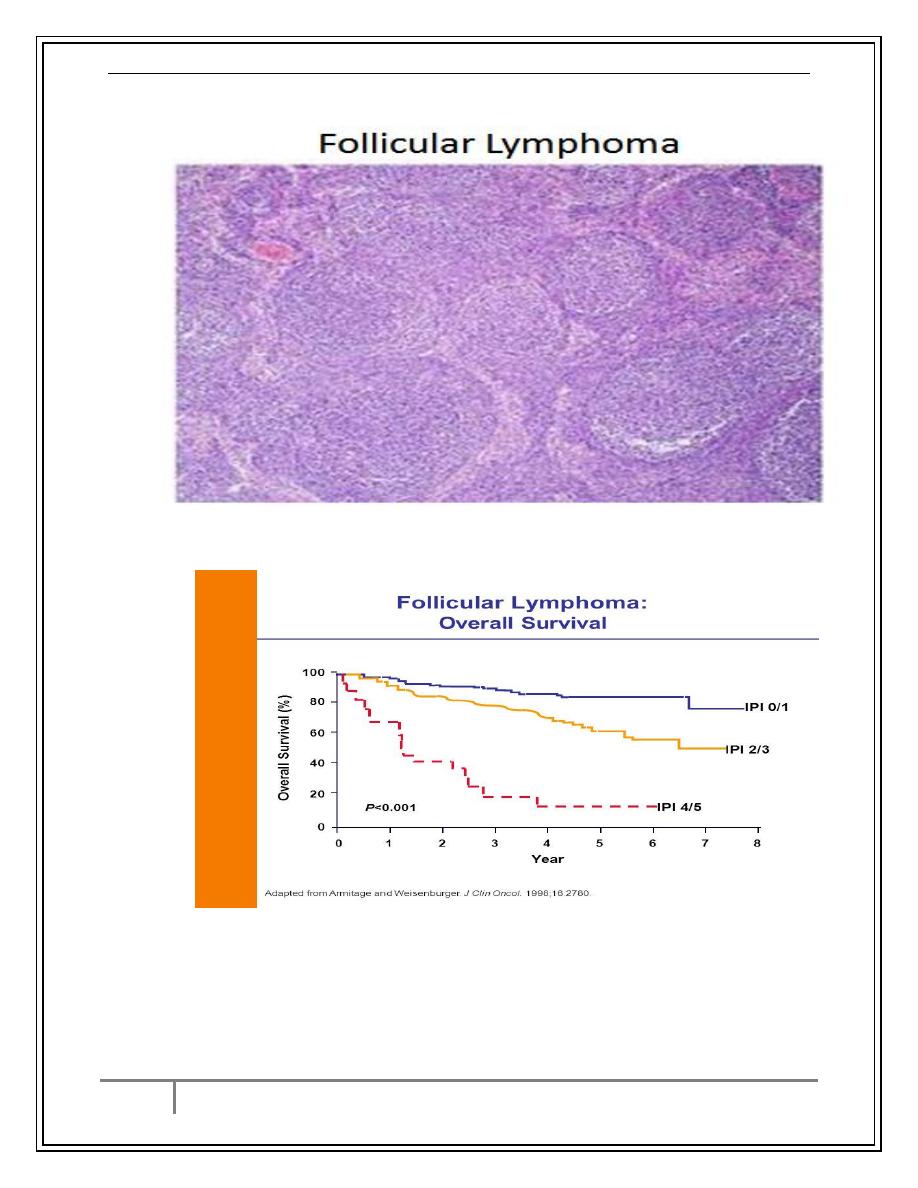
Follicular lymphoma.
Extranodal marginal zone B-cell lymphoma of mucosa-associated
lymphatic tissue (MALT) type.
Nodal marginal zone B-cell lymphoma (± monocytoid B-cells).
Splenic marginal zone lymphoma (± villous lymphocytes).
Hairy cell leukemia.
Plasmacytoma/plasma cell myeloma.
Diffuse large B-cell lymphoma.
Burkitt lymphoma.
Non-Hodgkin's Lymphoma
1) Updated REAL/WHO Classification
2) T-cell and putative NK-cell neoplasms
3) Precursor T-cell neoplasm: precursor T-acute lymphoblastic
leukemia/LBL.
4) Peripheral T-cell and NK-cell neoplasms.
o T-cell chronic lymphocytic leukemia/prolymphocytic leukemia.
o T-cell granular lymphocytic leukemia.
o Mycosis fungoides/Sézary syndrome.
o Peripheral T-cell lymphoma, not otherwise characterized.
o Hepatosplenic gamma/delta T-cell lymphoma.
o Subcutaneous panniculitis-like T-cell lymphoma.
o Angioimmunoblastic T-cell lymphoma.
o Extranodal T-/NK-cell lymphoma, nasal type.
o Enteropathy-type intestinal T-cell lymphoma.
o Adult T-cell lymphoma/leukemia (human T-lymphotrophic virus [HTLV]
1+).
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
6
By : taher ali taher
o Anaplastic large cell lymphoma, primary systemic type.
o Anaplastic large cell lymphoma, primary cutaneous type.
o Aggressive NK-cell leukemia.
NHL
*B-NHL forms 70%,while T-NHL forms 30%.
Aetiology:
Late manifest. Of HIV.
EBV,HTLV.(Certain lymphoma).
H pylori –Gastric lymphoma.
chronic HCV infection
Chromosomal translocations : t(14:18) –Follicular lymphoma.
Immunosuppressed patients after organ transplant, congenenital
immunodeficiency states.
Clinically,the most important factor is grade:
High grade: High proliferation rate, rapidly producing symptoms, fatal if
untreated, potentially curable.
Low grade: Low proliferation rate, may be asymptomatic for many years
before presentation. indolent course, not curable.
85% are either high grade diffuse large B-cell , or low grade follicular
lymphoma.
*Other forms include : mantle cellL.&MALT lymphoma (less common).
B-NHL classification by behavior
# The hallmark is +ve B-cell CD markers : CD19, CD20, CD79
*Indolent: slowly progressive , non curable
Mantle cell lymphoma.
Follicular lymphoma.
Extranodal marginal zone B-cell lymphoma of mucosa-associated
lymphatic tissue (MALT) type.
Nodal marginal zone B-cell lymphoma (± monocytoid B-cells).
Splenic marginal zone lymphoma (± villous lymphocytes).
*Aggressive: Rapidly progressive, potentially curable
precursor B-acute lymphoblastic -leukemia/lymphoblastic lymphoma
(LBL).
Diffuse large B-cell lymphoma.
Burkitt lymphoma.
Indolent: remitting & relapsing ,median survival- 10y.
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
7
By : taher ali taher
*Aggressive : 80% respond initially to treatment but only 35% have disease
free survival at 5y.
T-NK NHL classification by behavior
# The hallmark is T-cell markers: CD3, CD4 & CD8.
*Indolent: slowly progressive , non curable
Mycosis fungoides/Sézary syndrome.
*Aggressive: Rapidly progressive, potentially curable
precursor T-acute lymphoblastic leukemia/LBL.
Anaplastic large cell lymphoma, primary systemic type.
Peripheral T-cell lymphoma, not otherwise characterized
Student activity
Take 3 minutes to discuss how to prove that NHL is causing immune hemolysis
Indolent B- Lymphoma
Examples: Follicular lymphoma, Mantle cell Lymphoma , Marginal zone
Lymphoma.
Clinical Presentation:
Slowly progressive disease , may resemble CLL with lymphadenopathy,
hepatosplenomegaly, anemia, pancytopenia or lymphocytosis, sometimes
jaundice and immune hemolysis.
Diagnosis:
*LN biopsy: infilteration by malignant lymphoid cells with B-cell CD markers.
*CBP: may show anemia(immune and nonimmune), pancytopenia or
lymphocytosis.
*BM study: early bone marrow involvement.
*CT scan of Chest and Abdomen
*Renal and liver function tests.
Staging: similar to HD , Patients are categorized for prognosis by IPI score
Treatment: non-curable.
1-Asymptomatic:watch and wait.
2-Symptomatic:anti-CD20 Ab (rituximab), alkylating agents+prednisolone,
fludarabine, Combination of the above. Radiotherapy for SVC obstruction or
early localized disease.
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
8
By : taher ali taher
Survival of FL
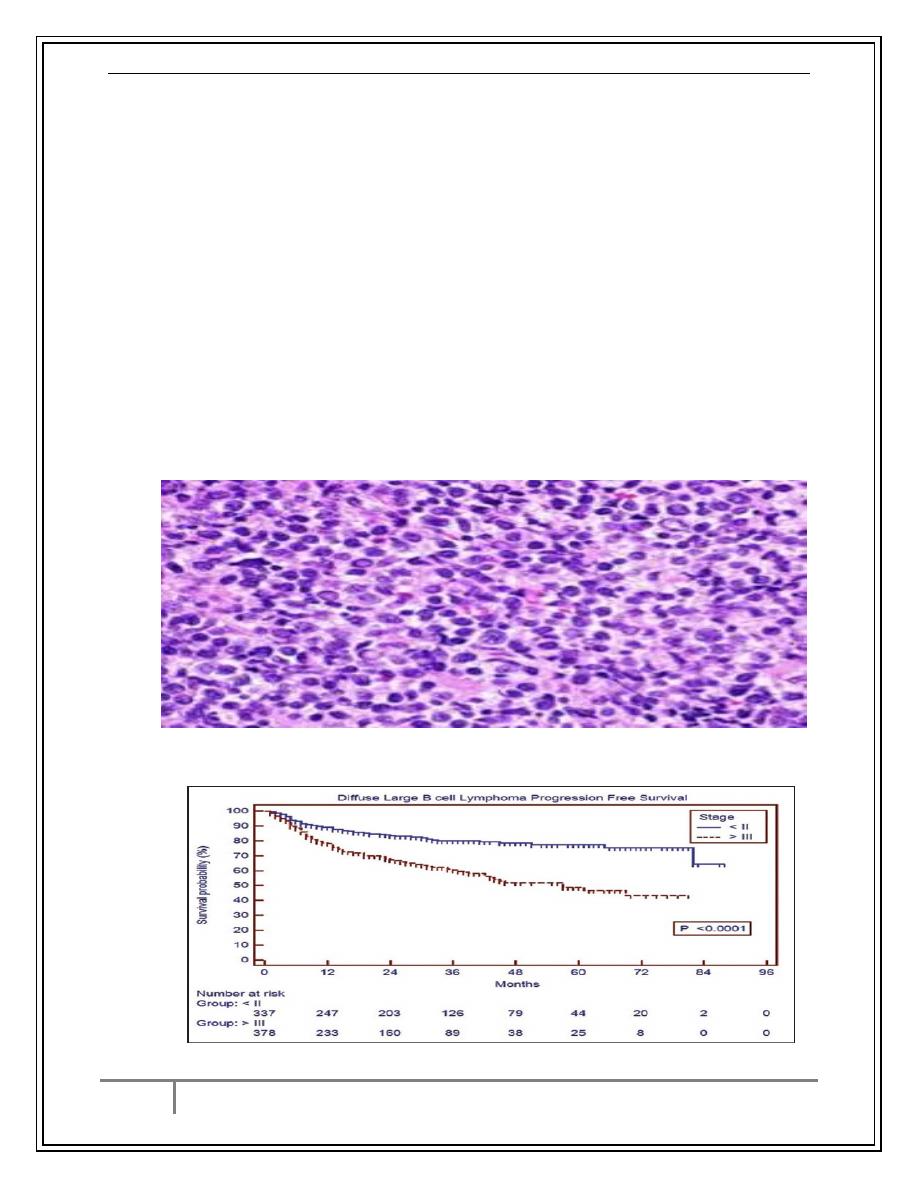
Aggressive B-Cell NHL
*Clinical Presentation: Rapidly progressive course
*Diffuse Large B-Cell Lymphoma (DLBCL):
Affects both sexes and different age groups.
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
9
By : taher ali taher
Patients present with cervical or other lymph node enlargement or extranodal
sites . BM is involved later on. May present with SVC obstruction or obstructive
jaundice or CNS involvement .Systemic B-symptoms are common.
Diagnosis and staging: same as other lymphomas. prognosis by IPI score
*L. Nodes will show infilteration by large lymphoid cells CD20+ve.
Treatment: potentially curable.
1-Rituximab+CHOP regimen
2-Local radiotherapy for obstructive lesions
3-Auto-BMT for relapsed cases
Prognosis: bad for old age ,high LDH ,extranodal involvement, bulky.
*Burkitts lymphma: may present with abdominal or jaw mass or acute
leukemia picture and treated as so, mostly in children, very aggressive and fatal
if not treated aggressively.
DLBCL
Survival of DLBCL
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
10
By : taher ali taher
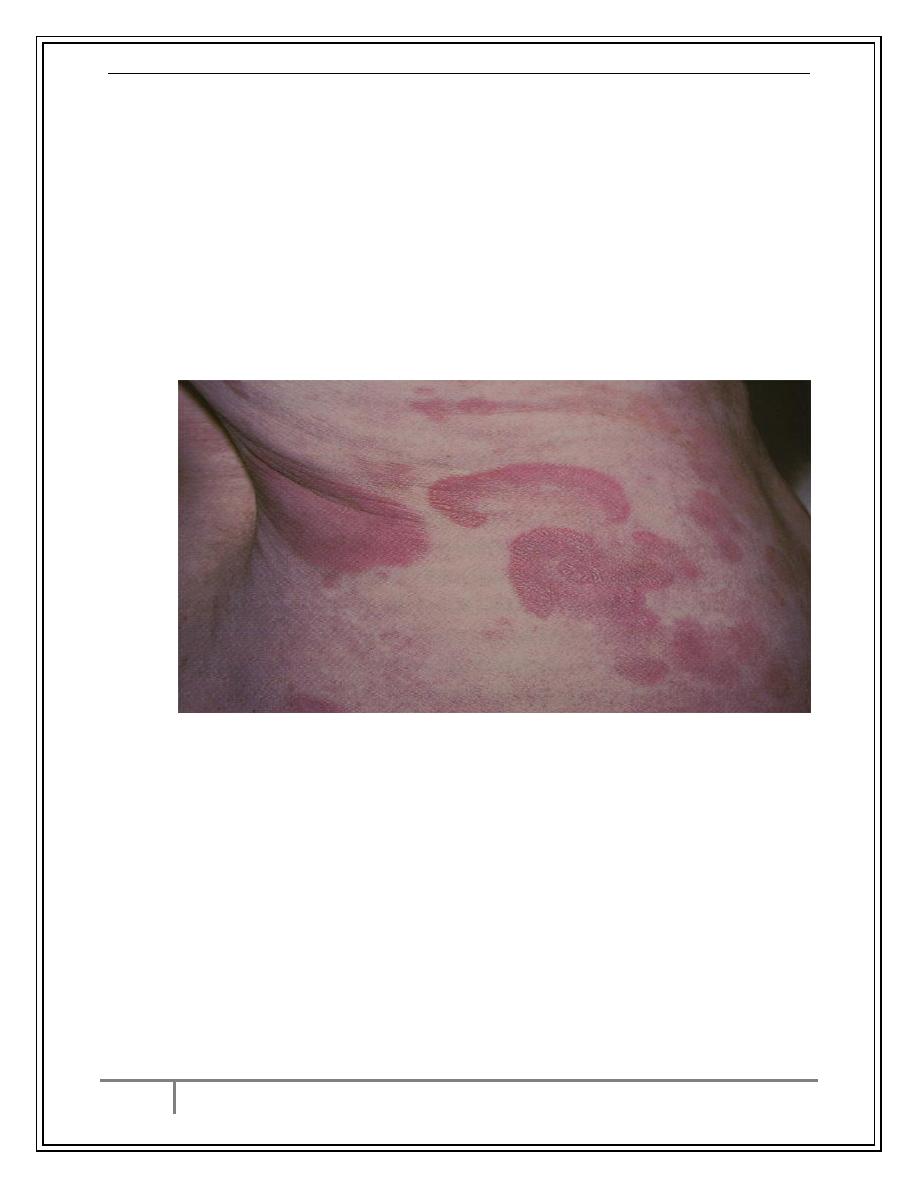
Cutaneous T-cell NHL (Mycosis Fungoides)
*Malignant disease due to proliferation of Helper T-lymphocytes
*It affects mainly the skin, the course is indolent.
*Presents with Itching, Skin macules and then nodules.
*Peripheral blood involvement is called Sezary syndrome.
*Visceral involvement is late
Treatment: Psoralin+UV light (PUVA), Topical corticosteroids ,Low dose
methotrexate, Photherapy, alfa interferone, Vitamin A analogues.
Mycosis Fungoides
Plasma Cell Myeloma
Neoplastic proliferation of a single clone of plasma cells (the most
mature cells of B-lymphocytes) producing a monoclonal
immunoglobulin
The clone proliferates in the bone marrow and results in:
Skeletal destruction with osteolytic lesions, osteopenia, and fractures.
Epidemiology :-
o 1% of all malignant Diseases
o >10% of all hematologic malignancies
o Annual incidence of 4/100,000
o Slightly more frequent in men than women
o Median age at Diagnosis is 66 yrs.
o Median survival changed greatly with the introduction of new
treatments.
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
11
By : taher ali taher
Clinical Features
Anemia
Fatigue
Bone pain
Spine
Ribs
Pathological bone fractures
Repeated infections due to loss of normal Ig:
Pneumonia
UTI
Weakness and numbness in limbs.
Hyperviscosity.
Manifestations of Hypercalcemia.
Laboratory Investigations
CBC + blood film
A. Normocytic, Normochromic Anemia.
B. Rouleaux Formation >50% of patients, very high ESR
Increase blood urea, serum creatinine and uric acid and calcium in some
patients.
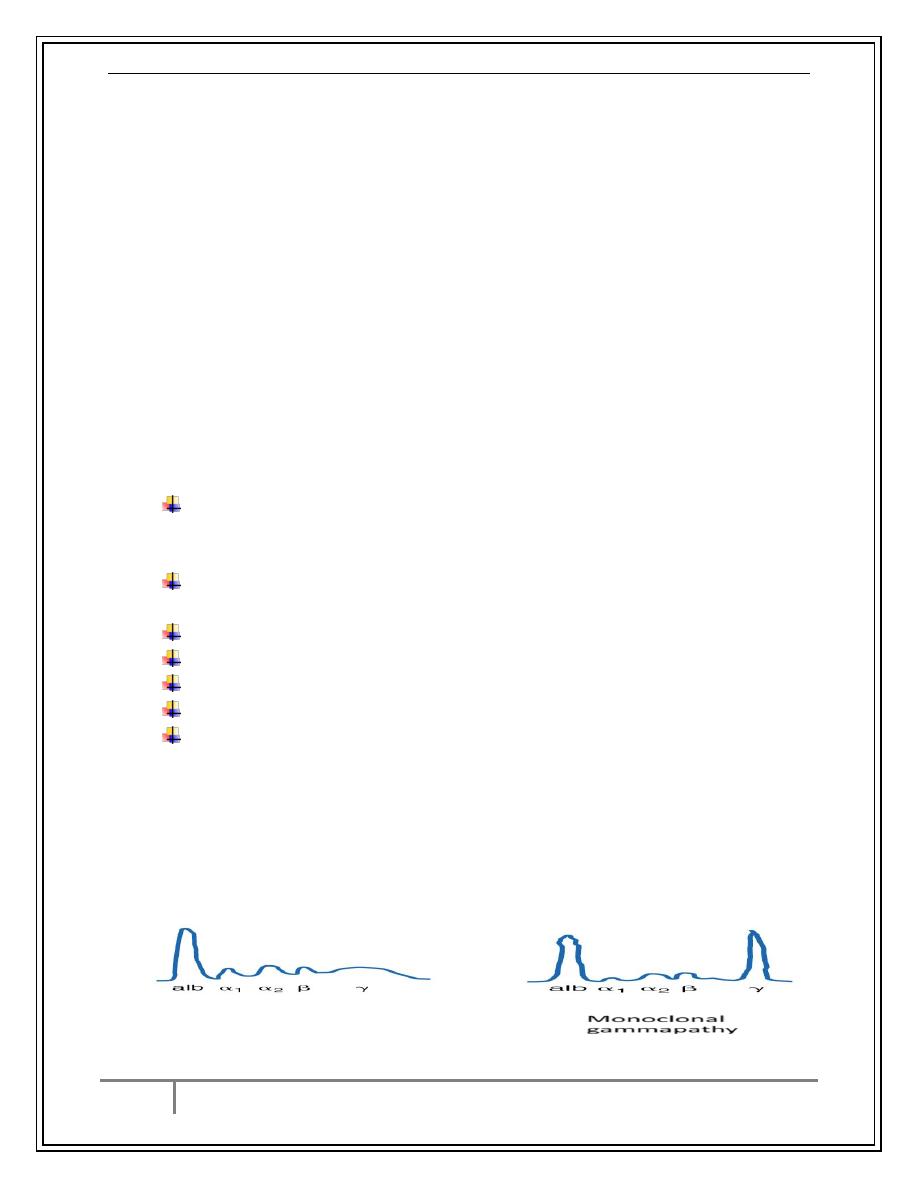
SPE – Monoclonal Protein (M-protein)
Immunoglobulin assay: mostly IgG type then IgA and IgD.
Urine for Bence-Jons Protein.
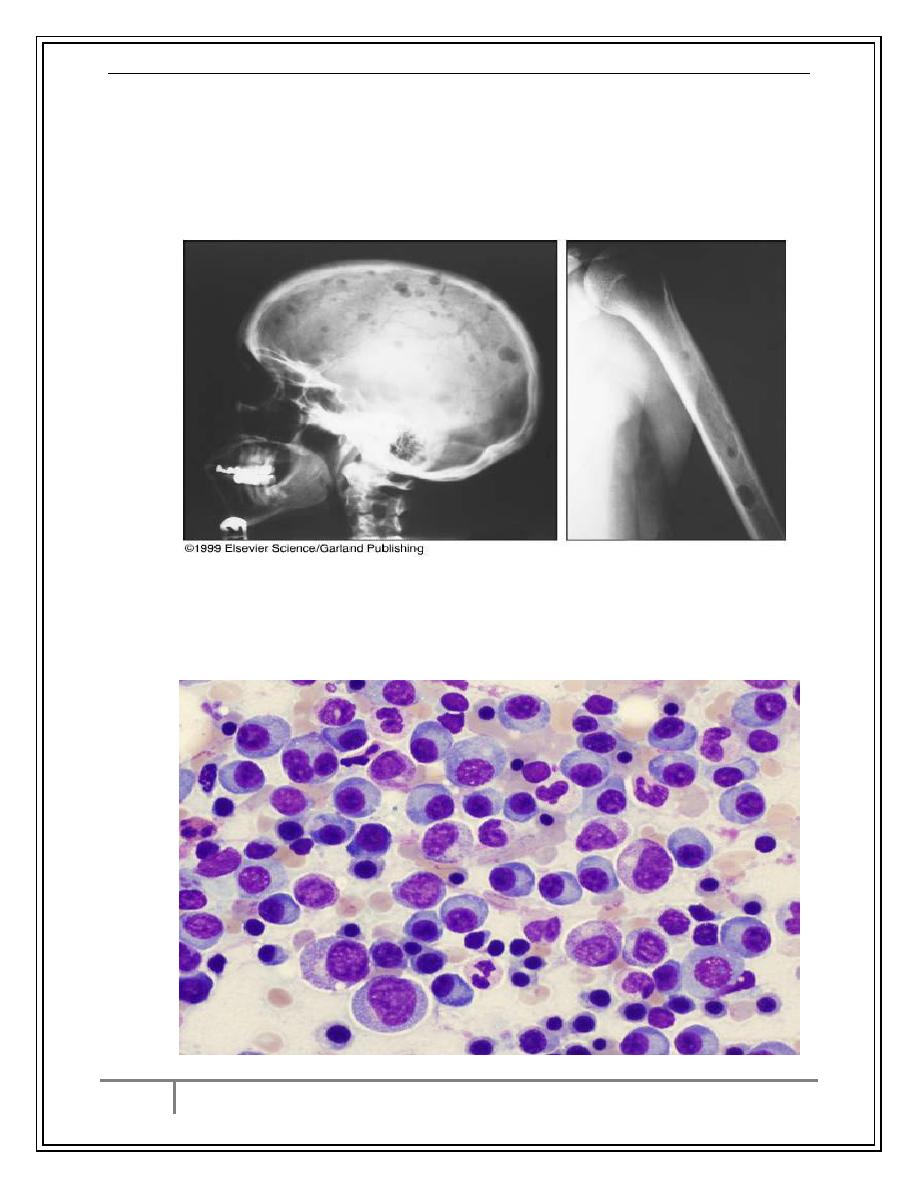
Osteolytic bone lesion by radiology and MRI of skeleton
Bone Marrow aspirate+ Biopsy : plasma cells > 10%
Diagnosis
The classic triad of myeloma:
1) marrow plasmacytosis (>10%),
2) lytic bone lesions,
3) serum and/or urine M component.
Norma
Monoclonal
gammapathy
Electrophoresis of serum
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
12
By : taher ali taher
Osteolytic Lesions
Plasma Cells in BM
Dr.Ali.M
Hodgkin's Disease, non-Hodgkin's Lymphoma & Plasma Cell Myeloma 16/3/2017
13
By : taher ali taher
Treatment
1-Supportive: good hydration, correction of anemia, allopurinol, zoledronic
acid.
2-Chemotherapy: not curable but induces remission and may prolong survival.
Thalidomide and Linalidomide
Bortezomib
MP (melphalan and prednisone)
VAD (vincristine, doxorubicin, and dexamethasone)
3-Radiotherapy: for localized bone lesions or fractures.
4-Autologous BMT: after chemotherapy.
Poor Prognostic Factors
Serum albumin < 3 g/dL
Serum Creatinine ≥ 2.0 mg/dL
Age ≥ 70 years
Beta-2-microglobulin >4 mg/L
Serum Calcium ≥ 11 mg/dL
Hemoglobin <10 g/dL
Certain chromosomal abnormalities.
Monoclonal Gammopathy of Undetermined Significance (MGUS)
Increasing incidence with advancing age.
Asymptomatic and discovered incidentally.
Monoclonal protein in serum or urine is Present.
Serum M Protein <3 gm/dL
Bone Marrow Plasma Cells <10%
Absence of Anemia, Renal failure, Hypercalcemia, Lytic Bone Lesions
16% of patients will progress to PCM
Needs observation only
Conclusion
1-Hodgkin disease is a neoplasm of B-cells that presents mainly with
lymphadenopathy. RS cells are present in LN sections . The disease can be
cured by chemo (±radiotherapy) in a good number of patients.
2-non-Hodgkin lymphoma is a heterogenous group of B (and less common T )
lymphocytes.The most important factors that determine behavior is the cell
origin and grade .Aggressive B-NHL can be cured with chemotherapy.
3-Plasma cell myeloma is a malignancy of plasma cells. It affects elderly and is
non curable but can be controlled for a period of time with biological
treatment, chemotherapy and radiotherapy.(THE END)
