1
Fifth stage
Gynecology
Lec
Dr.Ahmad
//2017
Benign and malignant conditions of vulva and vagina
-The vulva-
Pruritus vulvae:
Is a common symptom which is an irritation of vulva sufficient to lead to scratching
Causes
1. Infections: trichomonas vaginalis or candidiasis, Parasites such as scabies and lice.
Threadworms
2. Skin conditions may affect vulval skin: eczema, psoriasis, lichen simplex, lichen planus,
and lichen sclerosus.
3. Sensitization of the vulval skin to drugs or chemicals as soap and disinfectant, chemical
spermicide, ointments.
4. Medical disorders: Diabetes, chronic renal failure, polycythemia, liver cirrhosis,
Hodgkin's disease., Urinary incontinence.
5. Non neoplastic epithelial disorder as lichen sclrosus, squamous hyperplasia
6. Neoplasia: VIN, carcinoma, lymphoma, Paget's disease
7. Excess or inappropriate hygiene.
8. Psychogenic causes.
Diagnosis:
• History:
• Carfull history ,including the use of any substance which might lead to allergy.
Examination
• general examination of the patient including inspection for dermatological lesion of
face, mucous membrane, hands, wrist, elbows, trunk,and knees
• Any evidence of systemic disease
• Gynaecological examination including inspection of cervix and vagina and vulva
urethral meatus and anal area
• Colposcopic examination of cervix and vagina and vulva
• Palpation of inguinal lymph nodes.
2
Investigations
• Bacteriological examination of vaginal secretions and scraping from the skin.
• Full blood count.
• Blood sugar
• Biopsy of the skin of vulva.
Treatment
successful treatment depends on two cardinal principles:
1. to remove any underlying cause.
2. to stop further damage to the skin by scratching.
• The help of dermatologist may be sought in difficult cases.
• Great care should be taken in prescribing any of anti-pruritics
• Corticosteroid applications sometimes used.
Vulval ulcer
• Aphthous ulcer
• Herpes gentalis.
• Primary syphilis.
• Crohn's disease.
• Behcet's disease.
• Lymphgranuloma venereum.
• Chancroid.
• Tuberculosis.
• Malignant ulcer.
Vulval lumps
• Most vulval lumps are benign and can be treated conservatively.
• Excisional biopsy is indicated in solid lesions or when the diagnosis is uncertain.
3
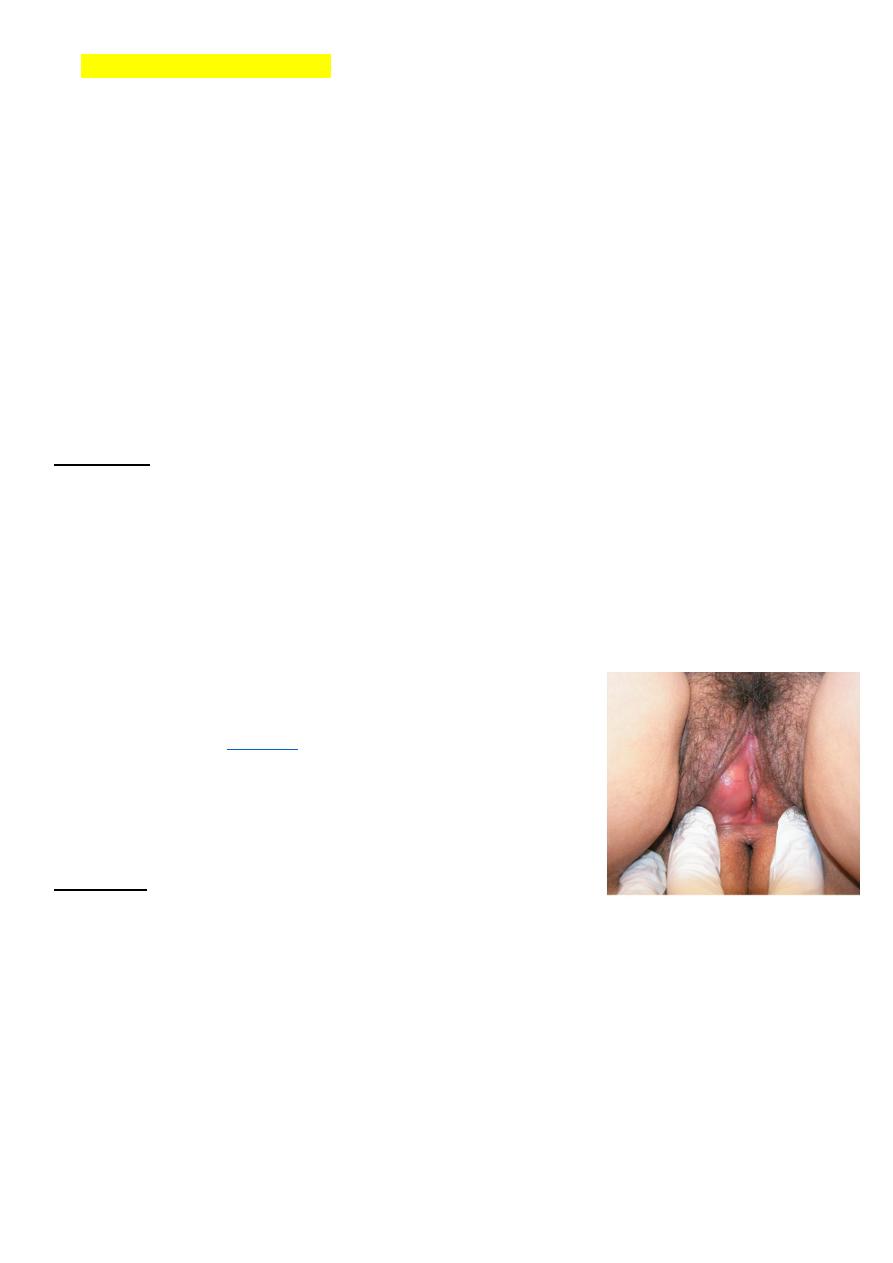
Bartholin's cyst and abscess
• Bartholin's glands lies on each side of the vagina and it's duct opens into the posterior
part of the vestibule..
Bartholin's cyst
• Is the most common vagial vulvar tumour. Cyst may arise from the duct of the
Bartholin's gland that lies in subcutaneous tissue below the lower third of labium
majorum. Cysts can develop if the opening of bartholin duct becomes blocked and
distended with mucoid secretion.
• It present as painless swellings or some time present with discomfort posterolaterally
in the introitus and usually unilaterally. It may become infected, to form an bartholin's
abscess.
treatment:
• marsupilizeation the cyst (permit adequate drainage and mostly the function of the
gland is retained).
or
• cyst excision.
Bartholin's abscess
• Bartholin's abscess involves an accumulation of pus that
forms a lump(
• the gland may be infected by gonococci, staphylococci,
streptococci or a mixture of organisms.
• it causes severe discomfort when walking or sitting.
Diagnosis:
• Symptom: it causes severe discomfort when walking or sitting.
• Physical examination:
• Diagnosis of a Bartholin abscess is made primarily upon the following physical
examination findings:
• the position of the labial swelling at the junction of anterior two third (2/3)and
posterior one third(1/3) of the labium majorum is diagnostic
• painful red swelling with reddens of the surrounding tissue and odematous.
• the swelling is hot, tender and fluctuant
4
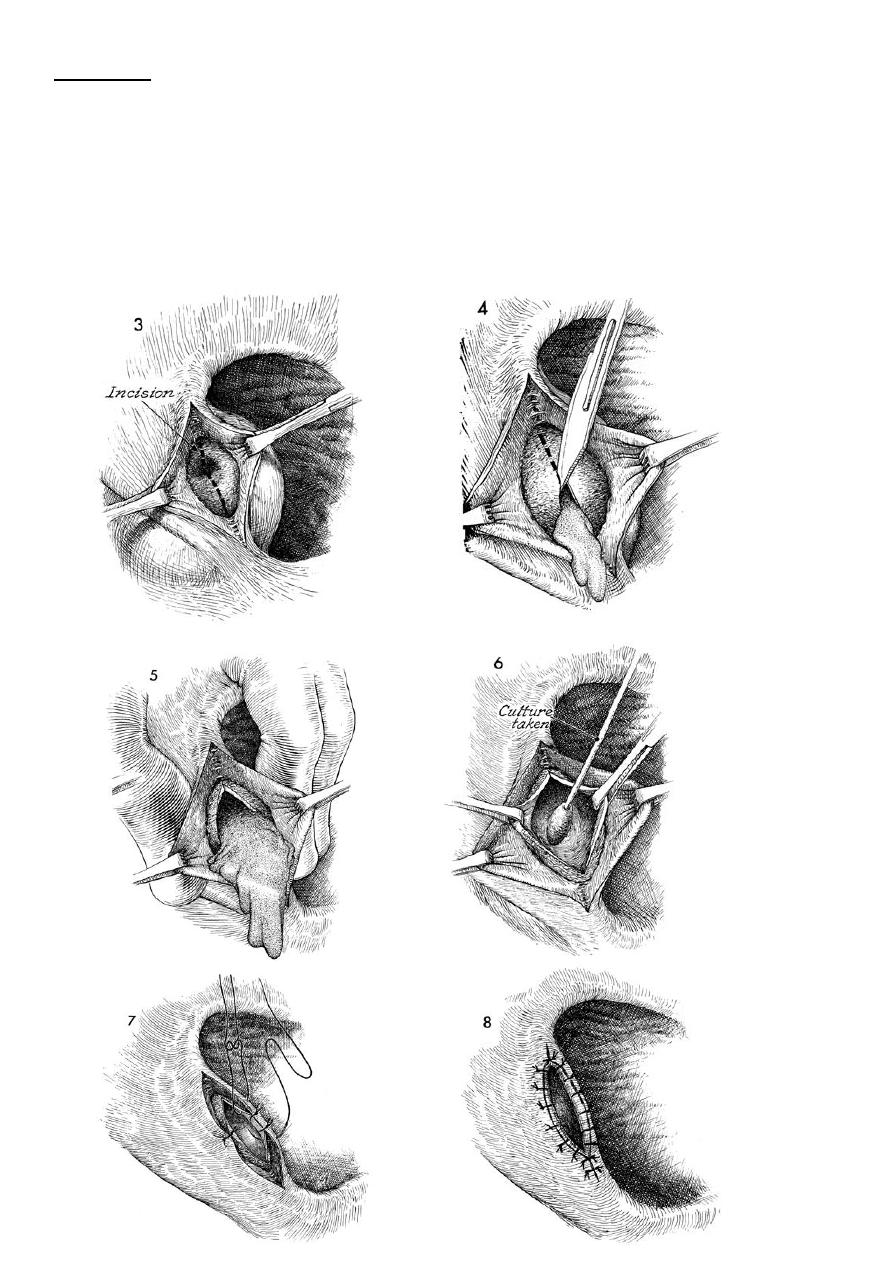
treatment
:
• drain the abscess by marsupilzation (pouch making).
• Antibiotic therapy.
• the drained pus should be sent for culture.
• biopsy may be recommended in older women to rule out an underlying Bartholin's
gland tumor.
5
Vulvae intraepithelial neoplasia(VIN):
• It may present at any age
• It dose not have the same malignant potential of that of CIN.
• It usually asymptomatic but it may present as Pruritus vulvae.
• colposcopic examination and biopsy are important.
• observation with regular follow up is required.
• Vulval Intraepithelial neoplasia: there are three grades from mild to sever dysplasia as
for CIN but doesn’t have the same malignant potential
Clinical features in VIN III
• Itching is the most common symptom.
• Half of patients are asymptomatic.
• Most have visible or palpable abnormalities of the vulva (20% are warty, and
multicentric in about two third of cases).
• Most lesions are elevated ,of different color : may be white , red ,pink , or brown.
Diagnosis:
inspection for abnormal areas.
colposcopic examination of the entire vulva after 5 % acetic acid will highlight
additional acetowhite areas.
biopsy will confirm the diagnosis.
Management :
-regular follow up with multiple biopsy
-local superficial surgical excision with safe margin with primary closure.
-for extensive lesions skinning vulvectomy with replacement by split –thickness skin
graft with the subcutaneous tissues are preserved.
-Laser ablation is used for multiple small lesions involving the clitoris, labia minora and
perineum.
6
Carcinoma of vulva
• It is uncommon (accounts 5% of genital cancer). It is a disease primarily of the older
age group with the majority of cases presenting between the ages of 60 and 75 .
Presentation:
• ulcer or swelling on the vulva with soreness or irritation.
• slight bleeding may occur.
• offensive purulent discharge .
• enlarged inguinal glands.
Examination:
• Ulcer or hypertrophic growths in vulva .
• Lymph node examination
Investigation:
• The diagnosis is made by biopsy.
• As well as investigate patient as in other carcinoma
staging
FIGO staging system is a surgical staging system revised in 1994:
Stage 0 carcinoma in situ ,intraepithelial carcinoma.
Stage I tumors confined to vulva or perineum ,lesion =or <2 cm; no nodal metastasis.
Ia stromal invasion <or = 1 mm
Ib stromal invasion > 1 mm.
Stage II tumors confined to vulva or perineum , lesion >2 cm, no nodal metastasis.
Stage III any size tumors with adjacent spread and or unilateral l.N.
metastasis.
7
Stage IV
IVa invades any or combinations of the following :upper urethra
,bladder mucosa ,rectal mucosa ,pelvic bones or bilateral
regional L.N.
IVb any distant metastasis including pelvic L.N.
Treatment
• radical excision of the vulva and inguinal lymph nodes on both sides.
• radiotherapy in special situation.
Survival rate:
• Overall 5 years survival is about 70%.
• Survival correlates significantly with the lymph node status regardless the stage,
one L.N. involvement 50% 5 years survival
no L.N. involvement 90% 5 years survival
-Vagina-
foreign bodies in the genital tract:
• The foreign bodies could be:
• A. Therapeutic agents:
o 1. Packs and dressing of various kinds may be left in vagina after operation.
o 2. Supporting pessaries.
o 3. Contraceptive device: (Sponges, occlusive caps, condoms which have slipped out).
• B. Articles inserted by the patient or entering accidentally.Mostly in mentally retarded
patient and children.
• C. instruments for inducing abortion and labour as: laminaria tents, chatheter.
• D. menstrual tampone.

8
Effects
• it is varies from irritation to local vaginitis result in ulceration of the vaginal walls
and perforation and pressure necrosis and this can involve neighboring structure to
cause urinary and faecal fistulae.
• infection may spread to produce salpingitis and peritonitis.
• carcinoma of vagina is a late squeal.
• The condition present as offensive vaginal discharge with blood stained as the main
symptoms.
treatment:
the foreign body must be removed
VAGINAL DISCHARGE:
• A vaginal secretion is normal in women in the reproductive age group.
• It consists of transudate containing desquamated vaginal epithelium, mucous secreated
by cervical glands and endometrial glands.
• The amount of discharge varies from woman to woman and varies throughout the
menstrual cycle(There is a cyclical variation of the amount of secretion).
• Normal discharge is usually clear or white. Infections may cause discharge of varying
color, consistency, amount and odor. A sudden change in discharge may signify
pathological condition.
Physiological discharge can be increased in:
• pregnancy.(due to increased estrogen production and greater blood flow to the area
around the vagina).
• in oral contraception users.
• At mid menstrual cycle
• During sexual intercourse.
• Exccesive vaginal discharge is a common gynaecological complaint and can cause
vulval symptoms. Comprehensive clinical assessment is essential.
Excessive Vaginal discharge could be due to:
1. Physiological.
2. Infection.(bacterial vaginosis, candidases, trichomonal vaginosis)
9
3. Foreign bodies as tampon, vaginal ring.
4. malignant (endometrial ,cervical, vaginal cancer).
5. Fistula.
6. Atrophic vaginitis.
7. large cervical ectropion
Vaginal atrophy
• It typically occurs in women of any age who experience a fall in estrogenic
stimulation to the urogenital tissues as in
• Menopausal women.
• Premenopausal women.
• Postpartum period.
• Lactation.
• During administration of antiestrogenic drugs (breast cancer hormonal treatment).
• Prior to puberty.
Symptoms:
• The patient may Present with vaginal bleeding, vaginal discharge, or vaginal
• dryness and dyspareunia (pain during sexual intercourse).
• Superficial infection, with Gram-positive cocci or Gram-negative bacilli, may be
• associated.
Examination:
• Shows pale, thin vaginal epithelium with loss of rugal folds and prominent
subepithelial vessels, sometimes with adjacent petechial haemorrhage or ecchymoses.
Treatment:
• Requires oestrogen to restore the vaginal epithelium and pH.
• This is usually by topical oestrogen cream, but care must be taken to avoid excessive
absorption through the thinned mucosa.Vaginal cream inserted nightly for a week and
repeated monthly to prevent atrophy.
• Alternatively in postmenopausal women, hormone replacement therapy(HRT)can be
used.

10
Fistula
A fistula may be due to:
• Trauma.
• Carcinoma.
• Crohn’s disease.
• Childbirth :(Fistula of the anterior wall is now uncommon in association with
childbirth, but rectovaginal fistula may follow an obstetric tear or extension of an
episiotomy, and an incomplete or inadequate repair).
• Gynaecological surgery Fistulae involving ureter, bladder or rectum may follow
gynaecological surgery.
Vaginal intraepithelial neoplasia(VAIN):
• It is seldom seen alone and is usually a vaginal extension of CIN (Cervical Intra
epithelial Neoplasia).
• Classification of intraepithelial neoplasias of the vagina parallels that of the cervix
VaIN 1, VaIN2, and VaIN 3.
• VaIN is usually asymptomatic and is diagnosed by abnormal cytologic testing.
Infrequently women complain of postcoital staining or unusual vaginal discharge
• VaIN usually occurs in the upper third of the vagina on the posterior wall
• VaIN lesions may be either single discrete or multifocal.
• Diagnosis is made by colposcopy.
• The usual treatment involves laser vaporization.
Carcinoma of the vagina:
• It is rare gynaecological tumours accounting for 1-2% of all gynaecological cancers.
• The peak incidence is between age 60 & 70 years.
• Vaginal carcinoma may be primary or secondary.
PATHOLOGY
• Only 10-20% of vaginal carcinomas are primary.
• Squamous cell carcinoma is the most common malignant tumor of the vagina
• Clear cell adenocarcinoma is found in women who had exposure to diethylstilbesterol
in utero (DES) and to a lesser degree in post menopausal individuals.
• Metastatic tumors are the most common cancer found in the vagina.

11
Secondary carcinoma can arise by:
• direct extension from the cervical carcinoma.
• Endometrial cancer.
• Choriocarcinoma.
• From vulva.
• From rectum or anus.
• Distant metastasis may occur from primary carcinoma in the breast or gastrointestinal
tract.
Clinical features:
• Usually occurs after the menopause and most commonly affects the upper posterior
wall.
• Vaginal bleeding mainly post coital.
• Offensive watery discharge.
• Fistula (rectum, bladder).
staging
•
FIGO staging used of vaginal carcinoma staging.
Stage I invasive cancer confined to the vaginal mucosa.
Stage II subvaginal extension not involving the pelvic side wall.
Stage III extends to pelvic side walls.
Stage IVa extends to mucosa of bladder &rectum
Stage IVb spread beyond the pelvis.
treatment:
•
Surgery:
removal of whole vagina ,uterus,and pelvic lymph nodes
• Radiotherapy in some cases.

12
-
Lesion of urethra-
Urethral Caruncle:
• Small, fleshy bright red out-growths of the distal edge of the urethra.
• It is always single lesion arises from the posterior wall of urethrra
• Usually seen in post-menopausal women. there is high rate of recurrence after
treatment.
It cause:
1.No symptoms
2.Symptomatic:
A. Very tender causing dysparunia or pain on micturition.
B. Slight bleeding may occur.
Treatment by:
• Topical estrogen therapy.
• If no response biobsy should be done to exclude serious morphology. Once
malignancy ruled out, it can be treated by surgery either by:
• Excision or destruction by diathermy.
Urethral diverticulae
• It usually found in the distal third of posterior urethral wall bulging towards the
vagina. It's incidence is 3%.
Clinical presentation:
• It is vary but usually include frequency , dysuria, dysparunia, voiding difficulties and
recurrent urinary tract infection. Post micturition dribble is classical symptom.
• Vaginal examination can show:
• No physical sign.
Or
• suburethral mass.
• Tenderness can be palpated.

13
Investigation:
• Voiding cystourethrogram.
Treatment:
• Surgical repair if patient affected by symptoms. Treatment by marsupilization and
vaginal diverticulectomy.
Diethylstibestrol (DES) - Related Lesions
• DES is a drug that was administered frequently to pregnant women who were at high
risk for early pregnancy loss during the 1940’s through the 1960’s.
it can be the cause of :
1.
Vaginal Adenosis
• Vaginal adenosis refers to the replacement of the normal squamous epithelium of the
vagina by columnar epithelium. It is asymptomatic and presents as red, granular
patches on the vaginal mucosa.
• Benign but rarely, may give rise to clear cell adenocarcinoma.
2.
Structural changes of the cervix and vagina and uterus.
These are in the form of:
• Transverse vaginal septum.
• Cervical hypoplasia.
• T-shaped uterus.
• others
3.
Exposed individual have an increased risk of abortion, preterm labour, ectopic
pregnancy.
4.
Clear cell adenocarcinoma
• It affects young women, average 17 years old. Two thirds of patients have history of in
utero DES exposure. The risk in exposed population is 1 in 1000.
