Principles of plastic surgery
Dr.Osama Esmaeel Al-MushhadanyWound Healing
Body attempt to restore tissue to its structural and functional pre injury state.Wound healing either by regeneration or repair
Wound Healing
All tissues repair except?Liver and bone
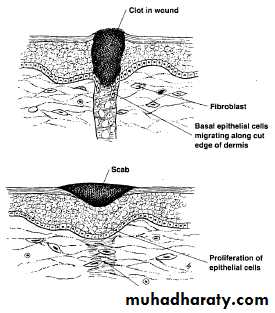
Wound Healing Normally Proceeds in an Organized Process• Four Phases of Wound Healing
• 1-Hemostasis
• 2-Inflammation
• 3-Proliferation
• 4-Remodeling (maturation)
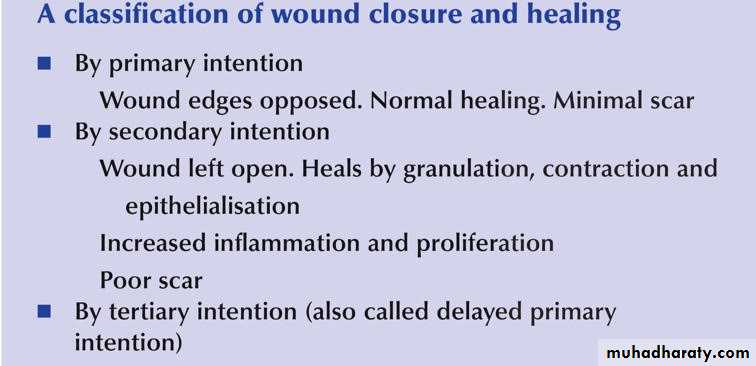
Classification of wound closure and healing
The final appearance of a scar is dependent on many factors:
Features of good scar
1- Fine line scar2- Absence of contour irregularities
3- No pigmentary irregularities
4- No contracture or distortion
.Age.
Who will have better scar a child or elderly patient?Obtaining A Fine-Line Scar
.Age.
Loss of elasticity combined with changes in the subcutaneous tissue, produce wrinkling, which makes scars in older individuals less obvious and less prone to stretching.Child: raised red scar.
Old age : flat white scar.
Obtaining A Fine-Line Scar
Obtaining A Fine-Line ScarType of skin:
Type of skin should also be taken into account. Skin that is oily or pigmented, or both, produces more unsightly scars..
Obtaining A Fine-Line Scar
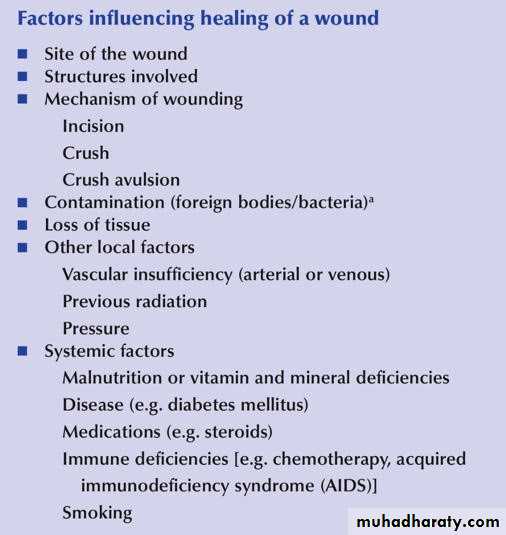
Certain anatomic areas produce unfavorable scars that tend to become hypertrophic or widened. The shoulder and sternal area are notable examples. On the other hand, eyelid scars almost always heal with a fine-line scar• Nutritional status can affect wound healing.
• Wounds gain strength less rapidly in the face of protein depletion.• Vitamin A reverses the healing retardation caused by steroids.
• Vitamin C deficiency has long been known to cause scurvy, characterized by a failure of collagen synthesis.
• Zinc is required for epitheliazation and fibroblast proliferation.
• Ferrous iron and copper are necessary for normal collagen metabolism.
Obtaining A Fine-Line Scar
Obtaining A Fine-Line Scar
Co-morbid conditions such as anemia,ureamia and Diapedus can retard wound healing. .
Obtaining A Fine-Line Scar
Atraumatic technique by:Minimizing damage to the skin edges with atraumatic technique
Debridement of necrotic or foreign material
Good irrigation of traumatic or contaminated wounds.
• Careful handling of tissue.
• No crushing or dryness.
• No strangulation or tension.
• Hemostasis.
• Sharp knife.
• No hot sponges.
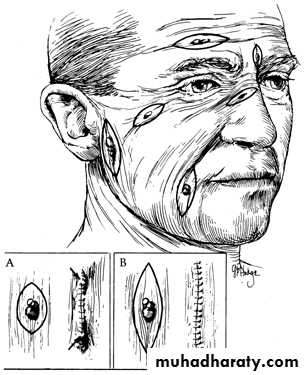
Skin lines
The lines of tension in the skin were first noted byLanger(1861) who described the normal tension lines of the skin, called “Langer’s lines”. Or called “relaxed skin tension lines”Excision of lesions is planned when possible so that the final scar will be parallel to the relaxed skin tension lines. Maximal contraction occurs when a scar crosses the lines of minimal tension at a right angle. Wrinkle lines are generally the same as the relaxed skin tension lines.
Obtaining A Fine-Line Scar
Method of homeostasis
Electro-cautery.
Ligature.
Pressure and time.
Clamping and twisting.
Vasoconstrictor.
Fibrin foam.
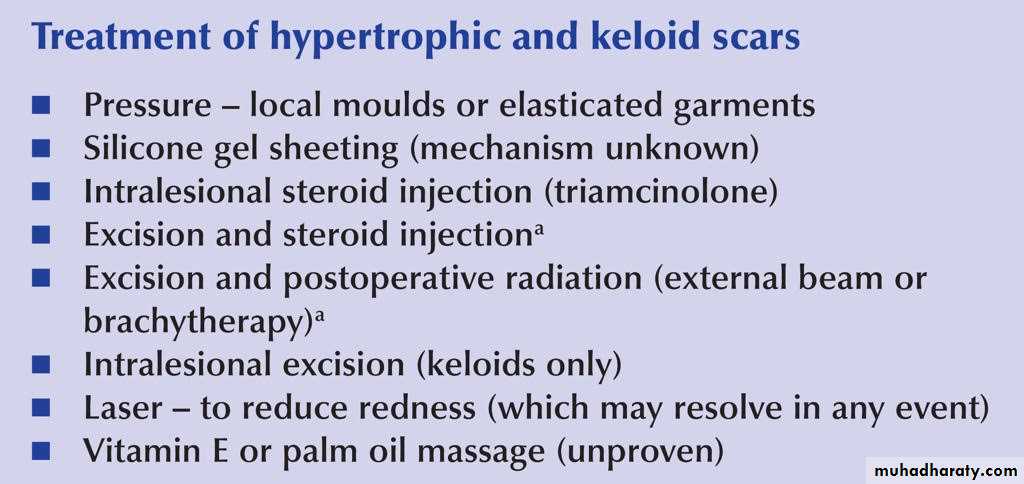
Abnormal scars:-
1- Atrophic scarThin, shiny scar occur over tension area treated by excision and resuturing with good realigment.
2-Hypertrophic scar
Elevated, with over growth but not extend beyond the inscion line.
The growth of the scar stop before 6 months.
3-keloid .over growth which extend beyond the inscion ,and continue to grow after 6 months.
Methods of suturing
A. interrupted.B. Vertical mattress.
C. Transvers mattress.
D. Subcuticular .
E. Continous.
Factors determine the severity of suture markers
• 1.Time of removal of stitches .
• 2.Diameter of the suture .
• 3. Relation to wound edges.
• 4. Region of the body.
• 5.Absence of infection.
• 6. Propensity for keloid.
•
When to remove the Stitches from different body sites?
Sutures• Are the most common materials used to close a wound.
• They are 2 types:
• Absorbable:
• Natural :
• Catgut (plain , chromic) from submucosa of sheep intestine.
• Collagen suture from flexors of beeves.
• Synthetic:
• Polyglycolic A.(Dexon ).
• Polyglactin 910 (Vicryl ).
• PDS (polydiaoxonon suture).
• Non-absorbable:
• Natural : silk, cotton. stainless steel.
• Synthetic:
• Polyamide (nylon): degrade 20 % / year.
• Polyester (Dacron, Ethibond)
• Polypropylene ( Prolene).
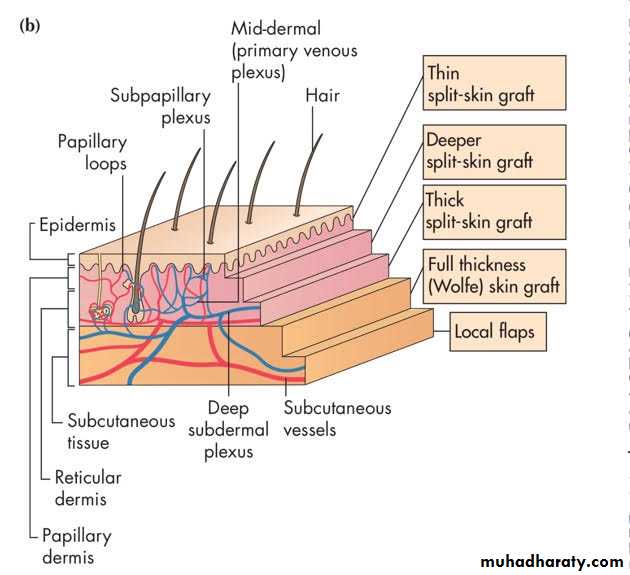
Skin graft
Definition: is a segment of epidermis and dermis that is removed without its blood supply from donor site transferred into a recipient siteTypes: according to:
Split-thickness graft(Thiersch graft):
Full thickness graft (Wolfe graft).
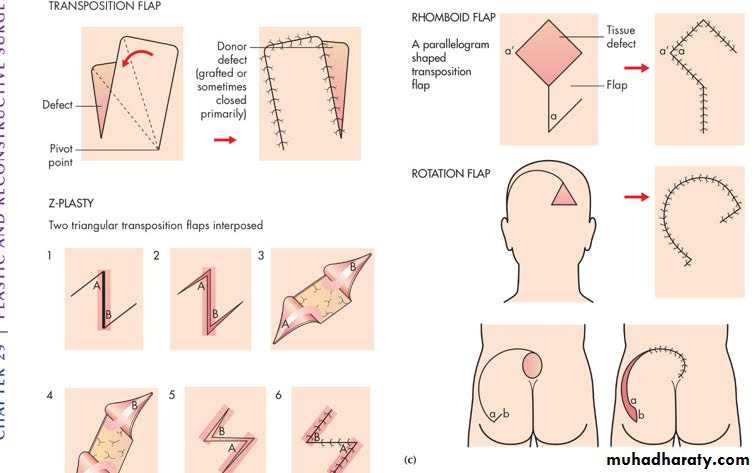
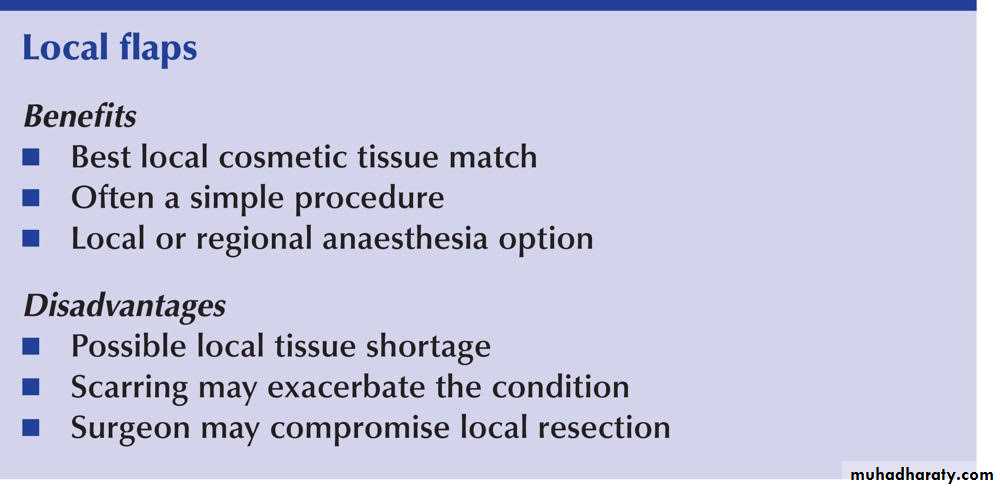
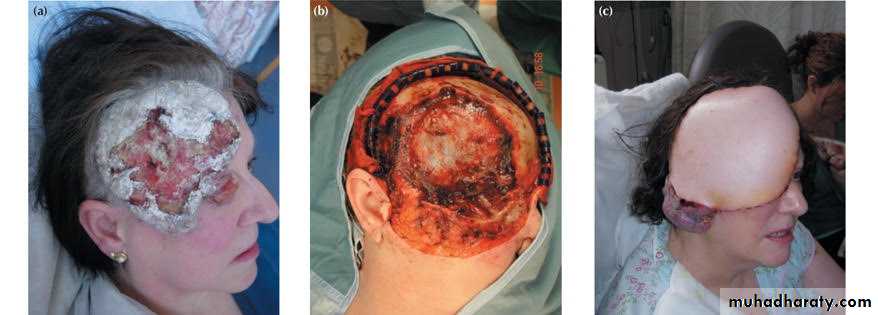
Flaps
“ part of tissue which retains its vascular attachment to body, transplanted to reconstruct a defect.”
The flap donor site closed by suture or SSG.
Tow main types)-1-local flaps.
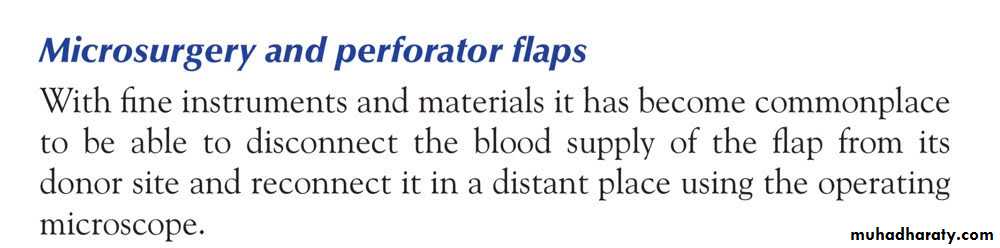
2-Free flaps(free tissue transfer)
Free tissue transfer(free flaps)
Skin tumors
Cleft lip and palateOne of the most frequently encountered congenital facial defects
Embryology: result of breakdown in the normal lines of fusion during the early stage of fetal development
Etiology of the clefts
The cause of the cleft lip and palate is multifactorial involving both genetic and environmental factors
15% of the cleft cases are syndromatic with more than 170 syndrome have it as a feature
Smoking is now well known to increase the incidence of clefting
Multivitamine and folic acid in the 1st four months of pregnancy is protective
Types of cleft lip and palate
Types of cleft palate
Common questions asked by the family
1-How to feed the baby
2-Timing of surgery
3-How many operation needed
Feedings
It is important to keep the cleft clean
Breast feeding is extremely challenging.
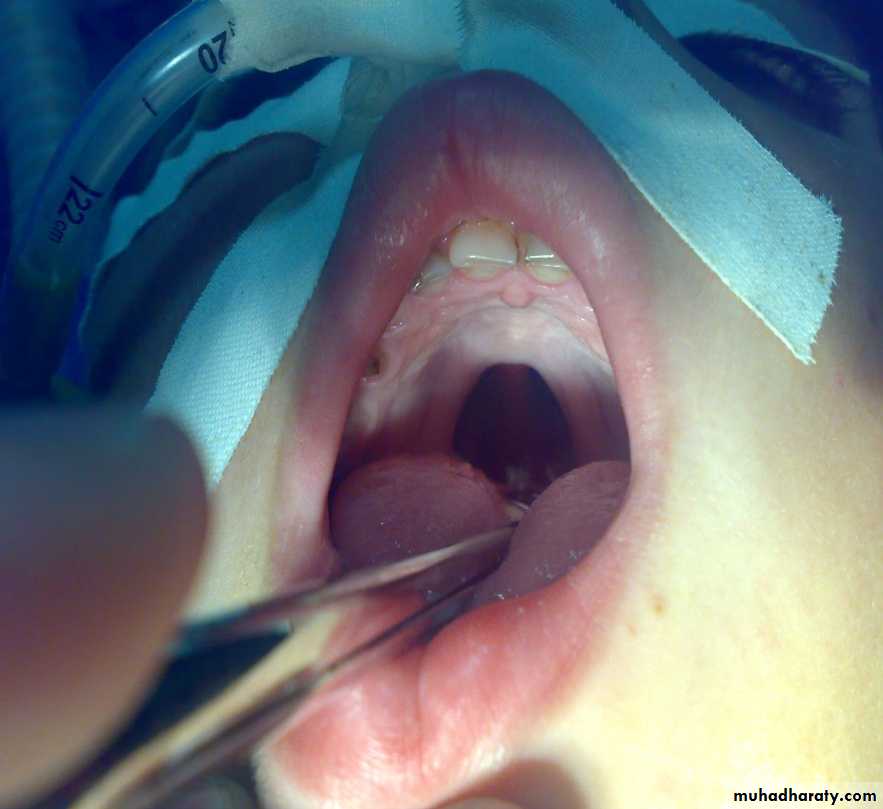
Repair :
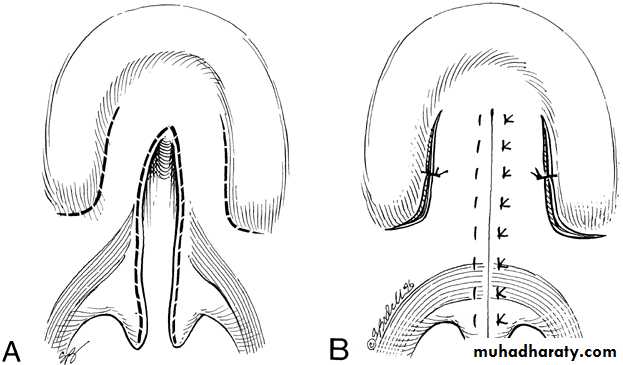
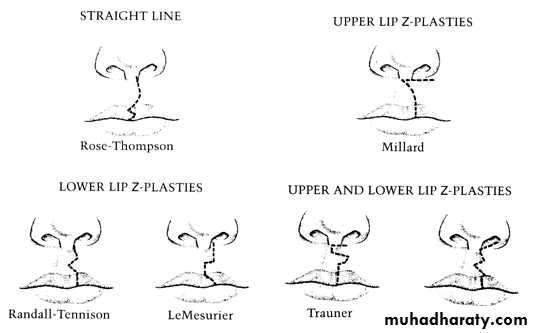
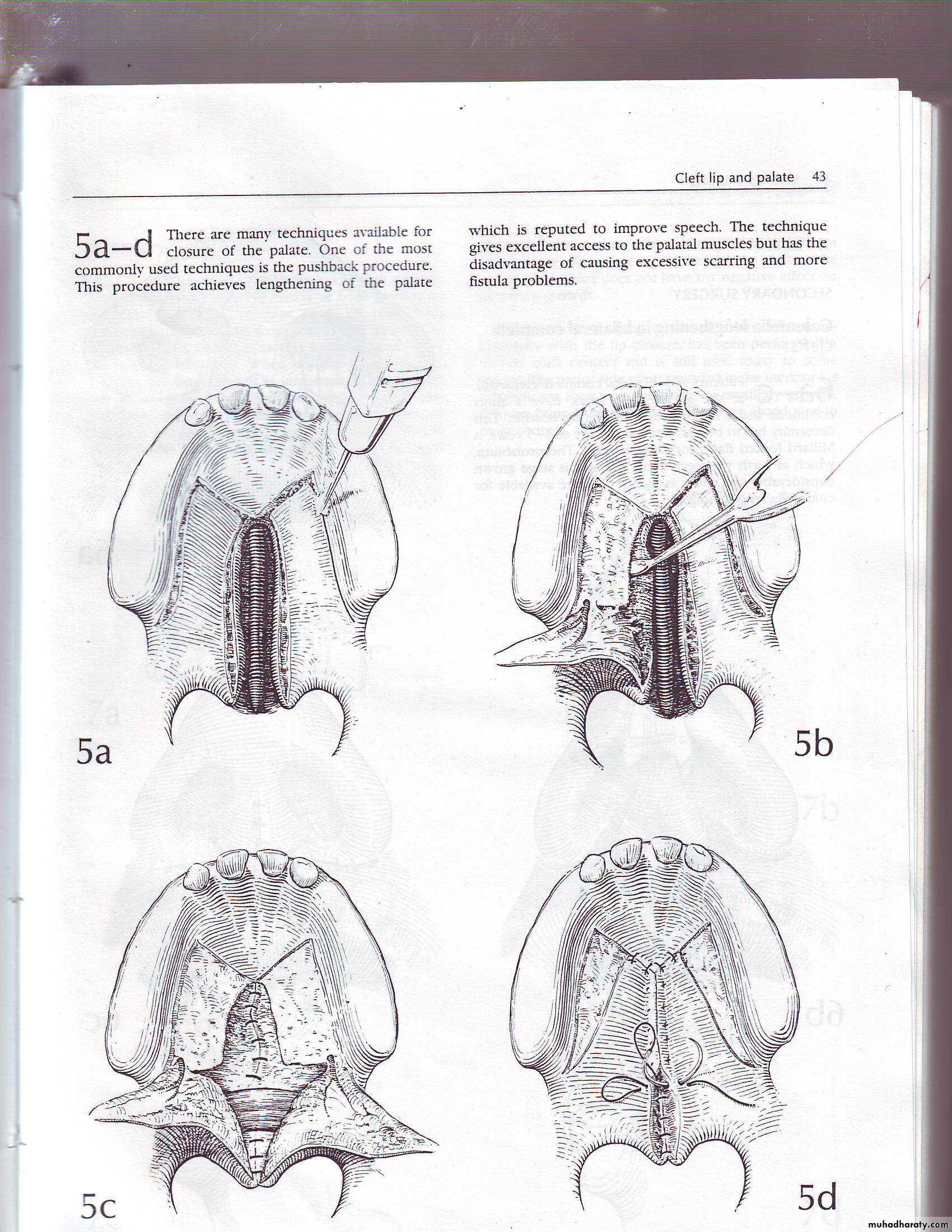
lip at 3 months or rule of 10 (10 pounds weight, 10 gm Hb, 10 weeks old).Palate : at 12-18 months, by Veau-Wardil, 4 flaps, Langenbek.
Millard op.
Veau-Wardil op.Langenbek
Effects on child :
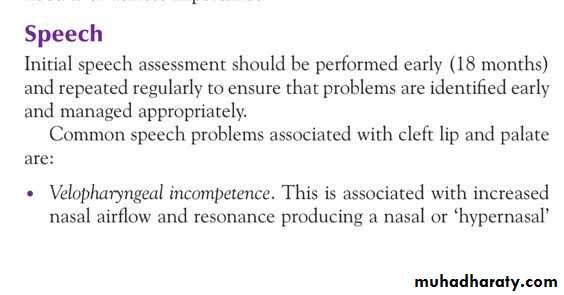
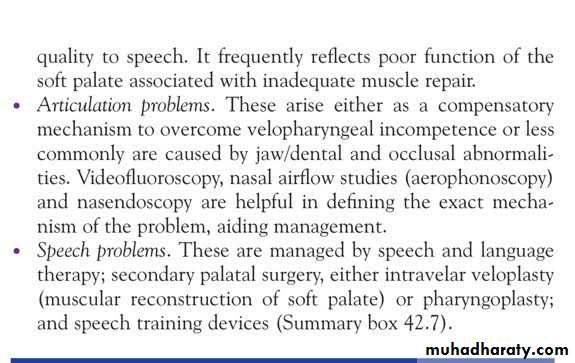
Hearing defectsSpeech –nasal.
Dentition deformity
Nose deformity.
.
Hearing
Eustachian tube dysfunction plays a central role in the pathogenesis of otitis media with effusion in babies and children born with a cleft palate.Basal cell carcinoma (BCC)
• Most common, 75% of skin tumors.• Arise from basal layer of epidermis.
• Affects white skin, Male: Female=3:2 .
• Occurs on exposed parts: face, neck, scalp.
• No metastasis.
• Commonly Caucasian male older than 60 years
Diagnosis: by biopsy (FNA, incisional biopsy , excisional biopsy)
Treatment:Surgery: excision with 2-5 mm. healthy margin, & repair defect by skin graft or flap.
Radiotherapy: in large lesion, oldman, refusing operation.
Cryotherapy: for primary lesion < 2 cm., but hypopigmentation, scarring are disadvantages.
Squamous Cell Carcinoma
(SCC) is second most common skin cancer.
arises from the malignant transformation of keratinocytes in the epidermis.
arise either in normal skin or in preexisting lesion as (actinic keratosis, leukoplakia, radiation keratosis, scars( where called Marjolin ulcer).
Clinically: present as irregular ulcer, everted edge, indurated base,attached deeply, blood-stained discharge,frequent lymph n. positive.
Treatment: biopsy done.
1- ExcisionSurgical excision with 10-mm margin
If lymph n. positive: excise lesion with lymph n. dissection.
2-Radiation therapy is best used in older patients,