Determination of serum Bilirubin level
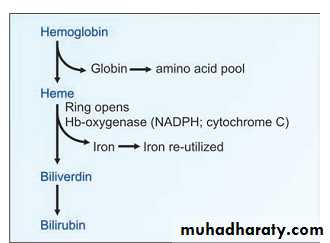
Generation of BilirubinThe end-products of heme catabolism is bilirubin. Bilirubin has nofunction in the body and is excreted through bile. The senescent RBCs breakdown and liberating the hemoglobin, the globin chains are separated, and the amino acids are channelled into the body amino acid pool. The iron liberated from heme is reutilized. Lastly, the porphyrin ring is broken down in reticuloendothelial (RE) cells of liver, spleen and bone marrow, to form biliverdin which is green in color. In mammals biliverdin is further reduced to bilirubin, a red-yellow pigment, by an NADPH dependent biliverdin reductase as figure below reveals.
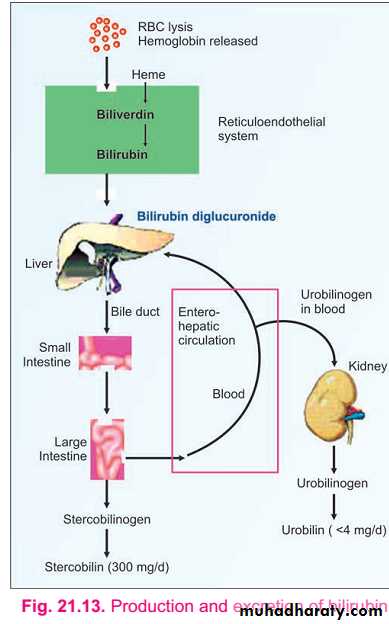
The bilirubin formed in the reticuloendothelial cells is insoluble in water. The lipophilic bilirubin is therefore transported in plasma bound to albumin. Inside the liver cell, the bilirubin is conjugated with glucuronic acid, to make it water soluble. The water soluble conjugated bilirubin is excreted into the bile. The conjugated bilirubin reaches the intestinethrough the bile. Intestinal bacteria deconjugate the conjugated bilirubin.This free bilirubin is further reduced to a colorless tetrapyrroleurobilinogen (UBG) ,further reduction of UBG leads to formation of stercobilinogen (SBG) . The SBG is mostly excreted through feces. 20% of the UBG is reabsorbed from the intestine and returned to the liver by portal blood. The UBG is again re-excreted (enterohepatic circulation). Since the UBG is passed through blood, a small fraction is excreted in urine. UBG and SBG are both colorless compounds but are oxidized to colored products, urobilin or stercobilin respectively by atmospheric oxidation.
Both urobilin and stercobilin are present in urine as well as in feces. The normal color of feces is due to these compounds. If intestinal flora is decreased by prolonged administration of antibiotics, bilirubin is not reduced to bilinogens, and in the large gut, it is re-oxidized by O2 to form biliverdin. Then green tinged feces are seen, especially in children.
Normal plasma bilirubin level ranges from 0.2–0.8 mg/dl. The unconjugated bilirubin is about 0.2–0.6 mg/dl, while conjugated bilirubin is only 0–0.2 mg/dl. If the plasma bilirubin level exceeds 1 mg/dl, the condition is called hyperbilirubinemia.
When the bilirubin level exceeds 2 mg/dl, it diffuses into tissues producing yellowish discoloration of sclera, conjunctiva, skin andmucous membrane resulting in jaundice. Icterus is the Greek term for jaundice.
HYPERBILIRUBINEMIASDepending on the nature of the bilirubin that elevated, the condition may be grouped into conjugated or unconjugated hyperbilirubinemia .
Based on the cause it may also be classified into congenital and acquired.
1. Congenital HyperbilirubinemiasThey result from abnormal uptake, conjugation or excretion of bilirubin due to inherited defects.A. Crigler-Najjar SyndromeHere the defect is in conjugation.
B.Gilbert's DiseaseThe defect is in the uptake of bilirubin by the liver.
C. Dubin-Johnson Syndromethe defect in excretion of conjugated bilirubin.
D. Rotor Syndrome
Bilirubin excretion is defective.
2. Acquired HyperbilirubinemiasA. Physiological Jaundice
It is also called as neonatal hyperbilirubinemia. In all newborn infants after the 2nd day of life, mild jaundice appears. This transient hyperbilirubinemia is due to an accelerated rate of destruction of RBCs and also because of the immature hepatic system of conjugation ofbilirubin.
B. Breast milk jaundice
In some breast-fed infants, prolongation of the jaundice has been attributed to high level of an estrogen derivative in maternal blood, whichis excreted through the milk. This would inhibit the glucuronyl transferase system.
3. Hemolytic Jaundice
Hemolytic disease of the Newborn, this condition results from incompatibility between maternal and fetal blood groups. Rh +ve fetus may produce antibodies in Rh –v mother.
4. Hepatocellular Jaundice
The most common cause is viral hepatitis, caused by Hepatitis Viruses A, B, C, D or E. In pure hepatocellular disease, conjugation in liver isdecreased and hence free bilirubin is increased in circulation. However, inflammatory edema of cell often compresses intracellular canaliculi at the site of bile formation and this produces an element of obstruction. When conjugated bilirubin level also increases, mixed type of jaundice
results (conjugated and unconjugated).
5. Obstructive Jaundice
Conjugated bilirubin is increased in blood, and it is excreted in urine. If there is complete obstruction, UBG will be decreased in urine or even absent. In total obstruction of biliary tree, the bile does not enter the intestine. Since no pigments are entering into the gut, the fecesbecome clay colored. The common causes of obstructive jaundice are:
a. Intrahepatic cholestasis. This may be due to:
a-i. Chronic active hepatitisa-ii. Biliary cirrhosisa-iii. Lymphomasa-iv. Primary hepatomab. Extrahepatic obstruction. This may be due to:b-i. Stones in the gall bladder or biliary tractb-ii. Carcinoma of head of pancreasb-iii. Enlarged lymph glands in the porta