Community
L7
Dr. Muslim N. Saeed
1
Obesity
*Overview
*Assessment
*Demographics
*Determinants of Obesity
*Medical Complications
Overview
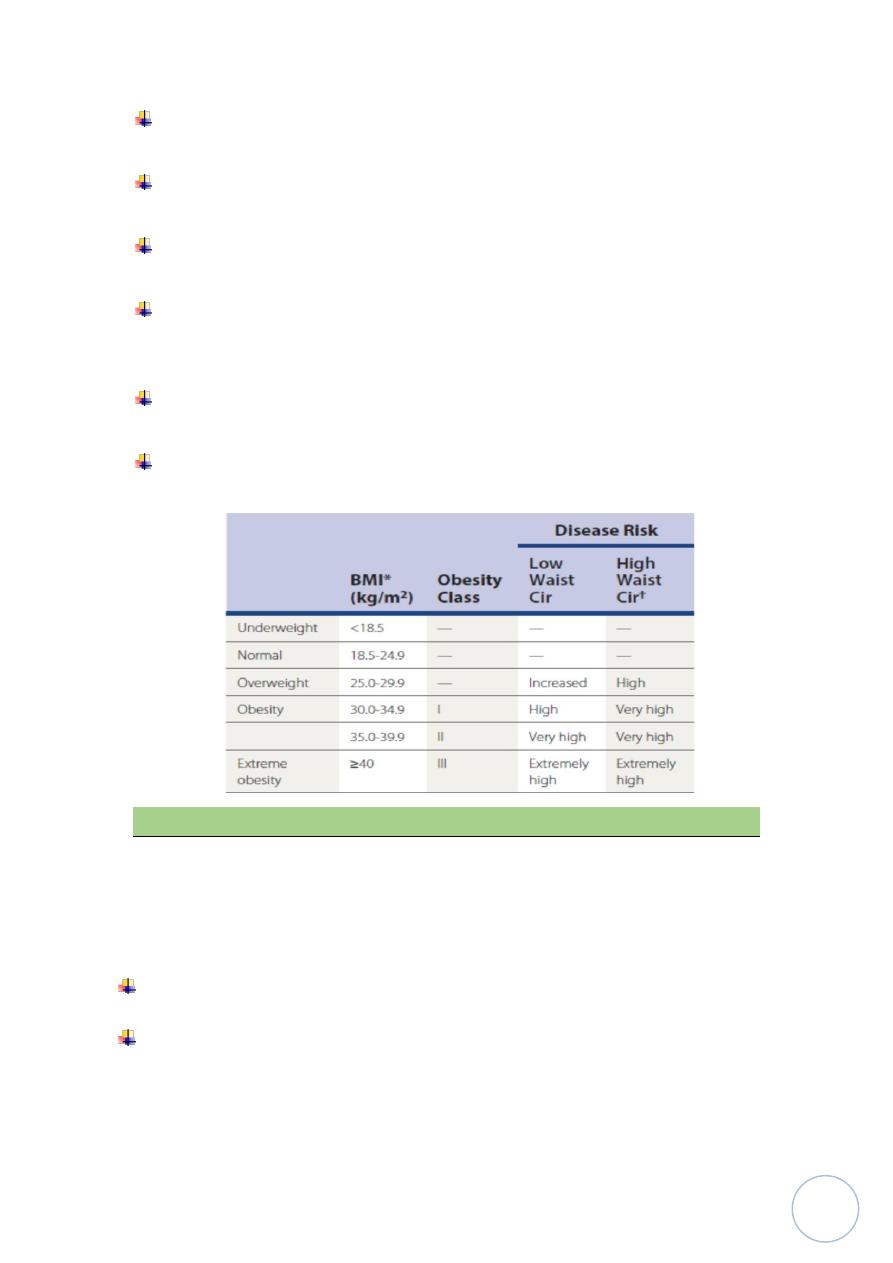
Body mass index (BMI) determines the classification of obesity for clinical
use.
Waist circumference reflects the distribution of adipose tissue and helps
determine obesity risk.
WC should be less than 101 cm in male, and less than 88 cm in female.
Assessment
The primary parameter used to categorize weight is BMI:
BMI= body Wt.(Kg)\ squared Ht. in meters
Ex. Wt= 70 , Ht=180 cm.
BMI= 70\ (1.8*1.8) =70 \ 3.24=21.60 kg\m2
-18.5 and 24.9 is normal in adults
-25 to 29.9 is overweight
-30 to 34.9 is class I obesity, 35 to 39.9 is class II obesity.
Class III, “severe,” or “extreme” obesity is 40 and higher. Calculated from
height and weight and expressed in kg/m2.
BMI is a recommended parameter to assess obesity, but an imperfect tool
to measure adiposity.
A high value may reflect greater lean body mass rather than adiposity in
muscular individuals.
In addition, BMI does not reflect distribution of body fat, a factor that
influences risk.
Body fat percentage is a more precise assessment of adiposity.
The techniques of skin fold measurements and bioelectric impedance assays
can be used, Cutoff levels for body fat percentage selected by WHO are used
to stratify health risks associated with overweight and obesity.
From birth to age 2 years, overweight is assessed by the weight-for-length
percentile; at or above the 95th percentile is considered overweight or
obese.
Community
L7
Dr. Muslim N. Saeed
2
For the pediatric population age 2 to 19 years, percentile ranks based on
CDC growth charts to define overweight and obesity.
The CDC defines overweight between ages 2 and 19 years as a BMI between
the 85th and 95th percentiles for age and sex.
A child or adolescent with BMI at or above the 95th percentile is considered
obese.
Central obesity, also referred to as visceral, abdominal, or android obesity,
is associated with a greater risk of complications, including the metabolic
syndrome.
gender- specific waist circumference, taken at the level of the iliac crest, has
proved to be a better assessment of the distribution of body fat.
Health risks increase above a waist circumference of 35 inches (88 cm) in
women and 40 inches (101 cm) in men.
Demographics
Men are more likely than women to have central obesity.
Obesity is inversely related to education and socioeconomic status.
Obesity is more prevalent in rural than urban areas.
1- Gender Differences:
Men are more likely than women to be overweight, whereas women are more
likely to be obese.
Men, however, are more likely to have central obesity, associated with greater
health risks.
2- Race and Ethnic Origin.
Community
L7
Dr. Muslim N. Saeed
3
3- Socioeconomic Status: The prevalence ranges from approximately 2% in
the least developed countries to over 30% in the most developed countries.
In developed countries, however, lower socio-economic status is associated
with an increased risk, because of reduced access to medical care, healthy
foods, and exercise facilities among lower socioeconomic groups.
4- Education Level:Education level is inversely related to the risk of obesity,
which may partly explain the decreased risk with increased socioeconomic
status in developed countries.
5- Rural and Urban Differences:
the prevalence of obesity is greater in rural than urban areas. Factors that
reduce physical activity may play a role.
Reduced availability of healthy food choices is also thought to contribute.
6- Age:
The incidence of overweight increases steadily after age 20 until the seventh
decade of life.
At that point, it levels off and begins a gradual decline.
The increased prevalence of overweight is especially alarming in the pediatric
population. More than 30% of children and adolescents are overweight or
obese.
Determinants of Obesity
Obesity results from the interaction of genetic makeup, environment, and
lifestyle.
Genetic factors are estimated to account for 30% to 40% of the variability
in adult weight.
Genetic influence is polygenic.
Specific metabolic or endocrine disorders account for less than 1% of the
obese population.
Genetic Factors
Most of the genetic influence on obesity is poly-genic. More than 250
genes and chromosomal regions are associated with phenotypic obesity.
Single-gene mutations related to obesity often
involve leptin and melanocortin.
There are a number of congenital syndromes in which obesity is part of the
phenotype.
Community
L7
Dr. Muslim N. Saeed
4
Modulation of Appetite
Many hormonal factors are involved in appetite, as well as in the absorption,
storage, and use of calories.
Factors providing input to the brain include leptin levels, vagal afferent
activity, and fluctuation in plasma glucose levels.
Neuropeptides and monoamine neuro-transmitters are also involved in
appetite control.
Lifestyle Influences
Increased caloric intake is related in part to “portion distortion,” linked to
eating away from home.
Smoking cessation is associated with weight gain of 4 to 5 kg (on average).
Many antidepressants, neuroleptics, and anticonvulsants are associated
with weight gain.
Decreased overall physical activity (not just “exercise”) is a major factor
associated with the increasing prevalence of overweight and obesity.
obesity develops when caloric intake exceeds caloric expenditure against a
background of genetic influences.
The chief determinants of energy imbalance are lifestyle factors.
Individual total energy requirements depend on the basal metabolic rate
(BMR), thermic effect of food, and energy needed for the day’s physical
activities.
The chief determinant of BMR is the amount of lean body mass, which can
be difficult to increase.
Physical activity (exercise and activity through -out the day) is the most
variable component of energy expenditure. The major reasons for weight
gain are therefore excessive calorie intake and decreased overall physical
activity.
Caloric Intake:
-tendency to consume more calories needed.
-Some of this increase is related to increased portion size.
-Energy density also plays a role.
-The frequency of meals may play a small role. Eating smaller meals more
frequently is associated with less overweight.
-Large meals are associated with more insulin release.
Community
L7
Dr. Muslim N. Saeed
5
Activity Changes
Decreased energy expenditure may play a greater role in the development
of obesity than increased caloric intake.
most of the decrease in physical activity energy expenditure has occurred
in daily physical activities, not exercise.
Smoking Cessation:
Often cited by smokers as a reason to continue smoking, stopping
cigarette smoking does lead to weight gain.
The average weight gain is 4 to 5 kg over months
Typically, the person gains 1 to 2 kg in the first few weeks after cessation.
Medications
A number of medications are associated with weight gain, including
antidepressants, antipsychotics, anticonvulsants, and hypoglycemic agents.
Tricyclic antidepressants, monoamine oxidase inhibitors are the anti-
depressants most likely to cause weight gain.
-Chronic systemic steroid use can cause a cushinoid type of obesity.
-Insulin, as well as oral hypo-glycemics that increase production or release
of insulin, promote weight gain.
-It should be noted that metformin, which increases insulin sensitivity, is
associated with modest weight loss and may ameliorate the weight gain
from other hypo-glycemics.
Endocrine and Metabolic Factors
Specific identifiable endocrine or metabolic disorders known to cause
obesity account for less than 1% of the obese population, contrary to what
is commonly believed.
Hypothyroidism
-in children, associated with slow statural growth and developmental delay.
-More common among adults and more often seen in women,
hypothyroidism is a relatively rare cause of obesity.
Community
L7
Dr. Muslim N. Saeed
6
Neuroendocrine Factors
The rarely seen neuroendocrine causes for obesity result from injury to the
ventromedial hypothalamus, due to tumor, trauma, or surgery to the
posterior fossa.
Cushing’s Syndrome
This endocrine disorder is associated with central obesity and “buffalo
hump” along with axillary striae, glucose intolerance and hypertension.
Polycystic Ovary Syndrome
More than 50% of women affected by this relatively common disorder are
obese.
Insulin resistance is a consistent finding, even in the absence of obesity.
Growth Hormone Deficiency
Although growth in height is impaired in growth hormone deficiency, there
is also an increase in truncal obesity.
Medical Complications of obesity
Obesity is more closely related to elevated triglycerides and low HDL
cholesterol than elevated total and LDL cholesterol.
Weight loss is the most effective lifestyle change to lower blood pressure.
Up to 80% of cases of type 2 diabetes mellitus are attributable to
overweight and obesity.
Obesity plays a role in 14% of cancer deaths in men and 20% in women.
Hypertension:
The obesity-related increase in blood pressure (BP) is associated with an
increase in vascular resistance as well as sodium resorption.
Controlling overweight would reduce the incidence of hypertension by an
estimated 28% - 48%.
Weight loss is the most effective lifestyle change to decrease blood
pressure.
Dyslipidemia
Obesity is associated with elevated TG levels, reduced (HDL-C), and an
increase in the more atherogenic, small, dense LDL particles.
This weight loss is generally accompanied by a decrease in total cholesterol
and LDL-C.
Type 2 Diabetes Mellitus
Community
L7
Dr. Muslim N. Saeed
7
The risk of T2DM is lowest below a BMI of 22 to 23 kg/m2. At a BMI of 31,
the risk for women
is 40-fold greater than in women with a BMI
less than 22.
For men, the risk of Type 2 DM above a BMI of 35 kg/m2 was increased 60-
fold. Up to 80% of cases of T2DM can be attributed to overweight and
obesity.
As weight increases, insulin resistance and compensatory insulin secretion
also increase. At some point, the body’s ability to secrete insulin does not
meet requirements, and blood glucose rises. Weight loss is recommended
to lower
elevated glucose levels in overweight and obese persons with T2DM.
Metabolic Syndrome
The metabolic syndrome brings together a number of the comorbidities
associated with obesity.
Definition:
BP elevation of at least 130/85 mm Hg,
(2) serum TG level higher than 150 mg/dL,
(3) HDL-C level less than 50 mg/dL in women and 40 mg/dL in men,
(4) fasting blood glucose level at least 110 mg%,
(5) waist circumference more than 35 inches in women and 40 inches in men.
-WHO add increased urinary albumin excretion and require the presence of
impaired glucose tolerance or T2DM.
Heart Disease
The presence of obesity in the absence of other risk factors may lead to
cardiomyopathy and congestive heart failure (CHF) as the workload of the
heart increases.
For women with BMI more than 29 kg/m2, CAD risk increases 3.3-fold
compared with women with BMI less than 21 kg/m2.
Cancer
Obesity may be the largest avoidable cause of cancer for non smokers.
Cancers of the esophagus, colon, kidney, gallbladder, and pancreas, as well
as multiple myeloma and non-Hodgkin’s lymphoma.
Community
L7
Dr. Muslim N. Saeed
8
Also, increased risk of prostate, gastric, ovarian, and endometrial cancers.
Obstructive Sleep Apnea
Excessive weight is a major risk factor.
About 70% of OSA patients are obese.
Pulmonary Disease
Obesity can have an impact on overall lung function, It increases the work
of breathing.
Obesity increases pressure on the diaphragm, reducing lung function.
Asthma is exacerbated with increased weight, and obesity-hypoventilation
syndrome and cor pulmonale is associated with marked degrees of
obesity.
Fatty Liver Disease
Fatty liver disease is the most common reason for elevated serum liver
enzymes. First described in obese diabetic females, fatty liver disease is
widely recognized as a complication of obesity.
Orthopedic Disorders
Overweight children have an increased risk of slipped femoral capital
epiphysis, genu valga, pes planus, and scoliosis.
In adults, degenerative joint disease, particularly of the knee, is related in
part to mechanical factors resulting in increased compressive forces on the
knee.
Gallbladder Disease
Obesity, hyper-insulinemia and the metabolic syndrome, are risk factors
for gallbladder disease, because cholesterol production increases with
weight gain, and cholesterol is excreted into bile.
The increased cholesterol relative to bile acids can lead to the formation of
stones.
Psychological Impact
Self-awareness of overweight and the associated psychological impact can
be seen in children as young as 5 years old and can result in poor self-
esteem.
This may result in poor body image, especially
in young women. Eating disorders, can complicate the management of
obesity. In adults, obesity is associated with depression in women.
